|
Table of Content Volume 15 Issue 1 - July 2020
Clinical study of depression in obese individuals at a tertiary health care centre
T R Chandrashekar1, Arun Joshi2*, Rajendra Kumar Katte3, R G Viveki4, Bhagyashri Hungund5, A R Shantha6
1Associate Professor, Department Of Psychiatry. 2Associate Professor, Department Of Medicine. 3Professor, Department Of Psychiatry. 4Professor, Department Of Community Medicine. 5Associate Professor, Department Of Pathology. Email: drtrcshekar007@gmail.com
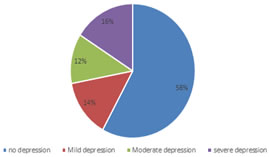
Abstract Background: Obesity is the rising health problem in world. Depression is most common mental disease. Prevalence of Both obesity and depression is increased in the world. Obesity and depression are inter related with each other. Obesity and depression together contribute a major burden on healthcare system. Aim and objective: To study the clinical profile of depression in obese individuals at a tertiary health care centre Methodology: A prospective study conducted on overweight and obese individuals attending general OPD of the tertiary health care centre. Data was collected with pre tested questionnaire by the investigator. Data included demographic data, clinical history, anthropometric measurements and data to assess depression. World Health Organization definitions applied to categories of overweight and obesity. Patient Health Questionnaire (PHQ‑9) was used to assess the Depressive symptoms. Data was analysed with appropriate statistical tests. Results and discussion: Mild, moderate and severe Depression was seen in 49(14%), 42 (12%) and 56(16%) patients respectively. Increase in BMI was significantly associated with increased severity of depression.(p<0.05) Key Word: xxxx, xxxxx
INTRODUCTION The World Health Organization (WHO) defines depression as a disorder characterized by sadness, loss of interest or pleasure, feelings of guilt or low self-worth, disordered sleep or appetite, decreased energy and poor concentration. 1,2 The Global Burden of Disease analyses of the WHO showed that depression is worldwide the third leading cause of disability at all ages and takes the first place in middle- and high-income countries. By 2030, depression is even expected to rank first in disease burden in the high-income countries.3 Depression impacts people of every age, sex, and ethnic background, with debilitating health care and disability costs. Obesity in adults is defined by the Centre for Disease Control and Prevention (CDC) as a body mass index (BMI) value of 30 or higher. 4 Recent studies suggest that obesity and depression may be bi-directionally linked. 5,6 Data from the National Health and Nutrition Examination Surveys, 2005–2010 showed that 43% of US adults with depression were obese, and adults with depression were more likely to be obese than adults without depression. 7 Like depression, obesity is significantly associated with increased risk for chronic diseases, such as type 2 diabetes and cardiovascular disease, and can lead to premature death. 8,9 The Patient Health Questionnaire (PHQ-9) Depression Screener used to evaluate depression. It includes questions about the frequency of overeating, lack of sleep and physical activity, suggesting several possible common links between the causes of depression and obesity. 10-12 Obesity and depression often coexist, and both can affect an individual’s health and productivity. Obesity with depression is associated with increased negative health outcomes, and higher mortality rates. 13,14 Effective treatment for concomitant depression helps to reduce overall health care costs, chronic disease rates, and improve health outcome. Present study was conducted to study the clinical profile of depression in obese and overweight individuals at a tertiary health care centre. Aim and objective: To study the clinical profile of depression in obese individuals at a tertiary health care centre
MATERIAL AND METHODS Present study was a prospective study conducted at tertiary health care centre. Study population was overweight and obese individuals attending general OPD of the tertiary health care centre. Inclusion criteria: 1. Patients with BMI ≥25 2.Patients above age of 18 years and below 60 years Exclusion criteria: 1. Patients below 18 years and above 60 years 2. Patients not willing to participate Study was approved by ethical committee of the institute. A valid written consent was taken from patients after explaining study to them. According to a study prevalence of depression among obese individuals was 23%.15 Sample size was estimated at 5% level of significance with an allowable error of 20% using formula
Where, n = Sample size p = Prevalence q = (1-p) L=Allowable error According to above formula sample size was 335. Considering the attrition problem we studied 350 patients. Data was collected with pre tested questionnaire by the investigator. Data included demographic data, clinical history, anthropometric measurements and data to assess depression. Weight of patients noted to the nearest kilogram and height noted to the nearest centimetre. BMI was calculated. World Health Organization definitions applied to categories overweight (25–29.9 kg/m2) and obese (>30 kg/m2). 16 Patient Health Questionnaire (PHQ‑9) was used to assess the Depressive symptoms. It is scored on a 27-point scale. Depressive symptoms were graded according to the following scores: (0-4) – no depression, score (5–9) – mild depression, score (10–19) – moderate depression and score (> 20) – severe symptoms of depression. 11 Statistical analysis Data entry and statistical analysis were conducted using the Statistical Package for the Social Sciences program version 21 (IBM Corporation, Chichago USA).
RESULT Total 350 patients were studied. Among these patients 227 (64.86%) were overweight and 123 (35.14%) were obese. Mean age of the patients was 42.54± 5.6 years. Minimum age was 18 years and maximum age was 57 years. Among all patients, 161(46.63%) were male and 189 (53.37%) were female. Male to female ratio was 0.85:1. In our study majority patients were from the age group of 41-50 years (36.86%) followed by 31-40 years (32.86%). Patients below 30 years were 16%. 51-60 years age group contributed 14.28% of all. Among the patients majority 290 (82.86%) were married and 17.14% were unmarried. (table 1) Fig 1 shows distribution of patients according to type of depression. Mild Depression was seen in 49(14%) patients. Moderate and severe depression was observed among 42 (12%) and 56(16%) respectively. Depressive symptoms were not seen in 203(58%) patients. Table 2 shows distribution of patients according to BMI and severity of depression. Among overweight patients mild depression was seen in 34 patients. Moderate depression was seen in 20 patients and severe depression was seen in 21 patients. 152 patients were without depressive symptoms. In obese patients 15 patients were with mild depressive symptoms. 22 patients were with moderate depression and 35 patients were severe Depression. 51 patients were without any symptom of depression. Prevalence of severe depression was 10% in obese patients in our study. In patients with mild depression 69.39% were overweight and 30.61% were obese. In moderate depression group 47.62% patients were overweight and 52.38% were obese. In patients with severe depression 37.5% patients were overweight and 62.5% patients were obese. Thus we can conclude that increase in BMI was associated with increased severity of depression. Severe depression was more common in obese patients than overweight patients. This difference was statistically significant. (p<0.05)
Table 1: Distribution oof patients according to variables
Figure 1: Distribution of patients according to type of depression
Table 2: Distribution of patients according to BMI and severity of depression
P <0.05 statistically significant
DISCUSSION Total 350 patients were studied. Among these patients 227 (64.86%) were overweight and 123 (35.14%) were obese. Mean age of the patients was 42.54± 5.6 years. In our study majority patients were from the age group of 41-50 years (36.86%) followed by 31-40 years (32.86%). Among the patients majority 290 (82.86%) were married and 17.14% were unmarried. In previous studies observed that more educated and unmarried group of individuals have worse mental health. 17,18 This was in contrast to our study. This difference was due to difference in the study population, difference in measurement procedures and measurement of depression. Advancing age was associated with depression which was also observed in earlier studies. 19 In our study Male to female ratio was 0.85:1. Females were more prone for development of obesity and depression. Females are more predisposed to depression through body image dissatisfaction, repeated dieting, and stigma. In our study, Mild Depression was seen in 49(14%) patients. Moderate and severe depression was observed among 42 (12%) and 56(16%) respectively. Prevalence of severe depression was 10% in obese patients in our study. In patients with mild depression 69.39% were overweight and 30.61% were obese. In moderate depression group 47.62% patients were overweight and 52.38% were obese. In patients with severe depression 37.5% patients were overweight and 62.5% patients were obese. Thus we can conclude that increase in BMI was associated with increased severity of depression. Severe depression was more common in obese patients than overweight patients. This difference was statistically significant. (p<0.05) our results are consistent with previous studies. L de Wit et al.... conducted a meta-analysis of community-based studies in which the association between depression and obesity was examined in adults and showed a significant positive association between depression and obesity in the general population, especially among women. 20 In a study by Keddie et al.... they observed an association between obesity and depression in severely obese women. 21 Dong et al.... suggested that extreme obesity is related to the increased risk for depression across gender and racial groups, even after controlling for chronic physical disease, familial depression, and demographic risk factors. 22 Luppino et al.... in a systematic review and meta-analysis of longitudinal studies demonstrated a reciprocal association between depression and obesity. They found that baseline obesity can increase following depression and this association is more robust for depressive disorder than for depressive symptoms and for Americans than for Europeans. 23 In contrast to our study Askari et al.... showed that obesity does not lead to depression.24 This inconsistency may be due to different population, different procedures used for measurements. According to previous studies the individuals with risk of mild depression to be treated with lifestyle modification, dietary advice, and involvement of pleasure-seeking activities. Individuals with risk of moderate depression need to be referred to psychological counselor for further investigation and counselling sessions. 25 In addition to weight management exercise improves mood of patients therefore exercise interventions are helpful for prevention of depression in obese individuals. 26,27
CONCLUSION Increased BMI is significantly associated with severity of depression so every overweight and obese individual should be screened for depression,
REFERENCES
Policy for Articles with Open Access |
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home