|
Table of Content - Volume 18 Issue 1 - April 2021
Medical comorbidity among patients diagnosed with schizophrenia spectrum disorders- A hospital based cross sectional study
B Hari Manasa1*, G Gopalakrishnan2, Kasthuri P3
1,2,3Department of Psychiatry, MVJ Medical College and Research Hospital, Bangalore -562114, Karnataka, INDIA. Email: harimanasa9@gmail.com
Abstract Background: Medical comorbidity is higher among persons with persistent mental illness due to various factors. When compared to general population, patients with schizophrenia have a shorter life expectancy with a difference of 10-25years and mortality rate is higher. Hence it is important to determine which chronic medical conditions are most common in patients with schizophrenia to deliver preventive and primary care at the earliest. Aims and Objectives: To study the prevalence of medical comorbidity in patients with schizophrenia spectrum disorders. Material and Methods: Patients aged between 20-40 years attending psychiatry OPD and IPD services in MVJ MC and RH who were diagnosed with schizophrenia spectrum disorders according to ICD-10 criteria were included in the study Informed consent was obtained. Data was entered in the sociodemographic proforma and scales like BPRS and CGI were applied to assess the severity of symptoms clinically. Participants were screened for any medical morbidity by physical examination and routine blood investigations were carried out. Chi-square test was applied and p-value was obtained to study the association .Results :100 patients were assessed of which 69 had one /more had medical comorbidity .The most Common was Diabetes mellitus(32%) ,hypertension(28%) and metabolic syndrome(17%) ,hypothyroidism(19%), nutritional deficiencies(39%) ,skin manifestations(16%) ,respiratory conditions (3%), cardiovascular(3%) ,gastrointestinal conditions(4.3%) , hyperprolactinemia (3%) and HIV(1.4%).Significant association was found with diabetes mellitus, metabolic syndrome , skin manifestations and hypothyroidism in patients with schizophrenia spectrum disorders.It was found to be more common in females than males in the age group of 31-40 years and subjects from low socioeconomic status and rural background were more effected .Conclusion: Treatment gap in patients with schizophrenia is high. Detection and management of medical/physical illness in patients with schizophrenia should be done at the earliest to improve the socio-occupational functioning. Keywords: chronic medical condition , schizophrenia spectrum disorders
INTRODUCTION Psychosis is defined as a severe mental disorder in which thought and emotions are so impaired that contact is lost with external reality. Psychosis includes schizophrenia spectrum disorders. Schizophrenia spectrum disorders include schizophrenia, acute and transient psychotic disorder, schizotypal disorder, delusional disorder, other nonorganic psychotic disorders, unspecified nonorganic psychosis and schizoaffective disorder both mania type and depressive type. Schizophrenia is a major mental disorder that encompasses a wide range of emotional, social and thought impairments.1 schizophrenia is a debilitating mental illness that affects about one percent of the population in all cultures and it has varied and ominous symptoms that usually begins in late adolescence or early adulthood and is generally chronic. 2 it is often associated with comorbid diseases and a cause of major public health concern worldwide. Medical comorbidities associated with these disorders involve respiratory system, cardiovascular system, gastrointestinal system , endocrinological and urogenital system. Substance abuse is high among these patients which further contribute to medical comorbidities. The patients with schizophrenia spectrum disorders , have about 15 to 20 years reduced life expectancy compared to the general population and excess mortality in these patients is also well documented.3,4 they have a 2-3 fold increased risk of dying, and this mortality gap associated with schizophrenia compared to the general population has widened in recent decades.5 a meta-analysis showed 60% of the excess mortality in patients with schizophrenia is attributable to physical illness.6 the causes of death comprises a broad range of conditions, similar to the general population, but however death occurs as a result of cardiovascular (cv) complications represents the leading natural cause of excess mortality in patients with schizophrenia.7,8 a review by mitchell aj et.al has identified four main reasons for the shorter life expectancy; 1) an unhealthy lifestyle, including reduced physical activity, smoking, poor diet and alcohol; 2) adverse effects of antipsychotic medicines; 3) delayed diagnosis and insufficient treatment of physical illness; and 4) a higher risk of suicide and accidents.9 The greatest research need at the moment seems to be identification of these specific risk factors responsible for the excess mortality among patients with schizophrenia.10 to help the psychiatrists to focus more on these cardiovascular risks in patients with schizophrenia, the concept of metabolic syndrome (mets) has received a lot of attention in psychiatric literature.11 the metabolic syndrome is a constellation of different conditions which are predictive of cardiovascular disease risk. 12 metabolic syndrome is a cluster of risk factors which includes increased abdominal obesity, impaired glucose tolerance, dyslipidemia and high blood pressure that causes increased cardiovascular disease and type 2 diabetes mellitus.12,13 A number of explanations like lifestyle and dietary habits that facilitate the development of obesity among patients with schizophrenia spectrum disorders, direct antipsychotic drug action on lipid and carbohydrate metabolism, the tendency to accumulate intraabdominal adiposity and fat, certain alterations of the hypothalamic pituitary-adrenal axis (hpa) producing hypercortisolemia and its genotypic expression in the form of truncal obesity, poor blood glucose control and possible associated alterations in hippocampal volume have been proposed.11 schizophrenia brings together a series of socio-demographic, clinical and metabolic parameters which are predictive of cardiovascular disease risk. For the increased risk of medical comorbidities in patients with schizophrenia, three complementary and partially overlapping causes are put forward in the literature: lifestyle factors, aspects of the psychotic disorder and antipsychotic medication. Age, gender, ethnicity, socioeconomic status, education, employment, marital status and residence; all of these factors have been found to influence in various studies. Clinical variables like age at onset, genetic risk factors, total duration of illness, family history, number of hospitalization, co-morbid medical and psychiatric disorders, sedentary life style, eating habits, substance use, chronic stress and use of psychotropic agents (particularly antipsychotics), have all been implicated in contributing to the pathogenesis of many comorbidities in patients with schizophrenia.16-20 early screening and knowledge about these co-morbidities can help primary (prophylactic), secondary (ameliorative), or tertiary (mitigating) prevention. The association between schizophrenia spectrum disorders and the medical comorbidities is emerging as a public health question of importance to both mental health and primary care practitioners. In order to address the above issue, the current study was carried out with an aim to evaluate the association of medical comorbidities in patients with schizophrenia spectrum disorders and to evaluate which is the most common comorbidity. There are some studies from india till date, which have focused on the prevalence of metabolic syndrome and other medical comorbidities among patients with schizophrenia spectrum disorders. As medical comorbidities are common among these patients and as these conditions are identified in a general hospital setting we would like to take up this study.
MATERIALS AND METHODS Study design: Cross-sectional descriptive study. Source of data: Patients who were attending psychiatry OPD and IPD services in MVJ Medical College and Research Hospital diagnosed with schizophrenia spectrum disorders will be considered for the study after obtaining informed consent. This study was conducted for a period of one year from October 2019 to October 2020. Sample Size = 100 Age group: Age: 20-40 years. Method of collection of data The study participants were 100 patients who met the International Classification of Diseases, Tenth revision (ICD-10) criteria (F20-29) for schizophrenia spectrum disorders. They were recruited by convenient sampling from the psychiatry outpatient and inpatient services of MVJ Medical College and Research Hospital over a period of October 2019 to October 2020.Ethical clearance was obtained from institutional ethics committee. Before participation all participants provided written informed consent. Diagnosis and symptom severity of participants with schizophrenia spectrum disorders were determined by using brief psychotic rating scale (BPRS) and clinical global impression scale (CGI) Sampling procedure Purposive sampling is defined as a type of non-probability sampling method. It involves determination of persons as per the requirements of the researcher. The requirement is generally based upon several criteria which also includes information about the research issue or ability and motivation of the sample group to participate in the research. Patients with schizophrenia spectrum disorders attending psychiatry IPD and OPD services in MVJ MC and RH will be included in the study. They will be screened through BPRS and CGI to assess the severity of symptoms. Inclusion Criteria Patients aged 20-40 years. Both males and females. Suffering from schizophrenia spectrum disorders, Qualifying ICD-10 criteria for the disorder will be considered. Those who agreed to participate in the study gave a written, informed consent. Exclusion Criteria Patients suffering from mental retardation. Patients who don’t give consent for the study. Instruments Informed Consent. Semi-Structured proforma for Socio-Demographic Profile. General Physical Examination including weight, height, BMI and blood pressure. ICD 10 diagnostic guidelines for diagnosis of Schizophrenia (F 20). BPRS. CGI. Basic blood investigations. A self-designed Informed consent form which explained the nature of the study was used. It was explained in the language best understood by the patient. Written informed consent was obtained on the form. STATISTICS The data was entered first into Microsoft Excel 2016 into tabular form. Statistical analysis of the data was done on the SPSS version 22.0 (Statistical Package for Social Sciences software). The tables depicting prevalence and correlation between variables were made using SPSS version 22.0. Frequency distribution was done for the sociodemographic variables. Qualitative variables will be presented as percentages and quantitative variables will be presented as mean±SD. P-Value and Chi-square test are applied to see the association.
RESULTS Out of 100 subjects, 69 were found to have one or more comorbidities and 31 did not have any. Out of 100 subjects, 32 were in the age group of 20-30 years and 47 were in the age group of 31-40 years. Out of 69 around 22 subjects are in the age group of 20-30yrs and 47 subjects were in the range of 31-40 years. Out of 100 patients, 38 subjects were males and 62 subjects were females. As mentioned in table 1, 69 subjects had comorbidities out of which 26 were males and 43 females respectively with comorbidities. 36 subjects were educated up to primary school or below out of which 22 had comorbidity and 64 were educated up to high school and above among whom 47 subjects had comorbidities. In the current study population 85 subjects were from rural background out of whom 25 had comorbidity and 15 were from urban background among whom 9 had comorbidity.
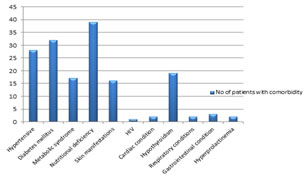
Table 1: Distribution of different medical comorbidities in the study population
Figure 1: The above table and graph depicts the percentage and number of subjects with comorbidities out of 100 patients with schizophrenia spectrum disorders was found to be 69 i. e. Hypertension 28 subjects (40.5%), Diabetes mellitus in 32 subjects (46%), metabolic syndrome in 17 subjects (25%), nutritional deficiency in 39 subjects (57%), skin manifestations in 16 subjects (23%), HIV in one subject (1.4%), cardiac conditions in the form of heart block and myocardial infarction in 2 subjects(3%), hypothyroidism in 19 subjects (28%). Significant association was found with diabetes mellitus, metabolic syndrome, skin manifestations and hypothyroidism in patients with schizophrenia spectrum disorders
DISCUSSION The main objective was to study the prevalence of medical comorbidities in patients suffering from schizophre spectrum disorders. Schizophrenia afflicts approximately one per cent of the population worldwide and is among the most disabling diseases in the young age group. Although the disability due to schizophrenia is coming down with advances in treatment, physical comorbidities such as cardiovascular, respiratory, neurological, infectious and sexually transmitted diseases remain cause for concern. Comorbid physical illnesses are one of the potential reasons for reduced life expectancy in schizophrenia. Various risk factors associated with lifestyle and treatment such as obesity, smoking, hypertension, dyslipidemia, hyperglycemia and neuroleptic medications add to the risk for developing physical illnesses.112,113-115 The prevalence of physical comorbidities in patients with schizophrenia has been reported to be high compared to the general population with odds ratios varying from 2.62 to 7.54.The patients are often unable to seek adequate physical care due to social isolation, lack of insight, lack of employment, difficulty in communication and reduced pain sensitivity. The present study was conducted in the Outpatients Visiting Department of Psychiatry, MVJ MC and RH suffering from schizophrenia spectrum disorders in the age group of 20-40 years to assess the presence of common physical comorbidities in patients with schizophrenia, their clinical and socio-demographic correlates and impact on functioning. One hundred patients (38 males and 62 females) were included in the study. The mean age was 32.94±5.65 years. Regarding educational status around 47 subjects out of 69 with comorbidities are educated up to high school. In terms of demographic status we found 60 subjects out of 69, belong to rural background and 9 belong to urban. Occupational status showed 68 subjects with comorbidity were unemployed out of 69 subjects. Marital status showed out of 69 patients with comorbidity 51 patients were married, 31 were unmarried and 5 were separated. We found that patients with schizophrenia were over-represented in areas of higher social deprivation. It is well documented that socioeconomic disadvantage and urban residence contribute to the risk of developing a psychotic disorder.116 Additionally, we found that women with schizophrenia were more likely than men with schizophrenia to have multiple comorbidities-this gender difference was also observed in the Swedish National Cohort Study noted above. People with schizophrenia and other mental illnesses have high rates of preventable risk factors and physical co morbidity accounts for 60% of premature deaths. In the present study in 69% patients, comorbid physical illnesses were detected on history and physical assessment. Koran et al. estimated that 45% of patients in California’s public mental-health system had physical disease. A study by Koranyi et al. of psychiatric clinic patients revealed that 43% of patients had physical illnesses. Hall et al. found that 46% of patients admitted had an unrecognized physical illness that either caused or exacerbated their psychiatric illness. Common comorbidities included hypertension (40.5%), diabetes mellitus (46%), metabolic syndrome (25%), nutritional deficiency (57%), hypothyroidism (28%) and skin manifestations (23.1%). A study by Holt and Pevler reported that diabetes occurred in 15% patients with schizophrenia lower as compared to present study (46%). Increased risk in people with schizophrenia of developing glucose regulation abnormalities, insulin resistance and type 2 diabetes mellitus found to be due to lifestyle factors (poor diet, sedentary behavior); and all antipsychotic agents (atypical more than typical) increase the propensity to develop diabetes. People with severe mental illness have 2-3 times more risk for cardiovascular disorders than the general population. People with mental illness have higher rates of cardiovascular and respiratory disorders than the general population; antipsychotic agents contribute to metabolic syndrome X (hypertension, hyperlipidemia, hyperglycemia, insulin resistance and obesity); lifestyle factors (smoking, alcoholism, poor diet, and lack of exercise) contribute to increased risk of cardiac problems. Mortality due to ischemic heart disease, cardiac arrhythmias and myocardial infarction is higher in people with mental illness. The present study reported prevalence of endocrinological abnormalities to be higher (28%) than the cardiovascular morbidity at 3%. Our findings are consistent with a study conducted by Smith DJ et al. who reported that people with schizophrenia had lower recorded rates of cardiovascular disease as compared to other physical health comorbidities. It is a well-known fact that both typical and atypical antipsychotics though are main stay of treatment for schizophrenia, are also associated with their side effects. In the present study out of 100 patients 72 patients were using antipsychotic drugs Gupta et al. (2003) reported a prevalence rate of 30% for hypertension, 17% for diabetes and 43% for lipid abnormalities in 208 patients with psychotic disorders who were receiving anti-psychotic medications.. Risk of metabolic syndrome also found to be higher in patients being treated with atypical antipsychotics. Heiskanen et al. (2003) found that 37% of patients with schizophrenia receiving antipsychotic medications developed metabolic syndrome higher as compared to present study (25%). Tarricone et al. (2006) found that patients treated with atypical antipsychotics had higher mean glycaemia and triglyceridemia and a significantly higher risk of receiving a diagnosis of hyperglycemia and hypertriglyceridemia than the reference group.
LIMITATIONS OF THE STUDY The study was cross-sectional and descriptive with no intervention or follow up. Our study had a limited sample size. The study population was hospital based and not representative of the community. Use of a basic set of physical investigations and lack of a control population. It showed presence of physical comorbidities in a substantial number of patients with schizophrenia even with a limited number of investigations. There is a need for multicentric nationwide studies with a larger sample and an expanded battery of investigations to reach to a valid conclusion.
CONCLUSION Our study concludes that: People with schizophrenia have high rates of multiple physical comorbidities, emphasizing the importance of an integrated approach to their care. As shown by this study, patient with schizophrenia spectrum disorders reported comorbid diabetes mellitus, hypertension, and metabolic syndrome among many others. Schizophrenia patients often receive inadequate medical care and low rates of treatment for co‑morbidities like HTN, DM, dyslipidemia and obesity. Sometimes the physical comorbidities remain unrecognized in such patients so integrated approaches such as assessment of medical illness by physician and psychiatric diagnosis by psychiatrist require to prevent and treat the comorbid disorders. Ultimately, to improve treatment outcomes and to reduce the suffering of people with schizophrenia, it is crucial to treat physical comorbidity promptly and assertively from the appearance of the first symptoms of psychotic disorder. Further research is needed to provide more insight into the risk factors and treatment modalities.
REFERENCES
Policy for Articles with Open Access: Authors who publish with MedPulse International Journal of Pediatrics (Print ISSN: 2579-0897) (Online ISSN: 2636-4662) agree to the following terms: Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution License that allows others to share the work with an acknowledgement of the work's authorship and initial publication in this journal. Authors are permitted and encouraged to post links to their work online (e.g., in institutional repositories or on their website) prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work.
|
|
 Home
Home