|
Table of Content - Volume 20 Issue 1 - October 2021
A cross sectional comparative study of physical comorbidities in patients with late onset psychosis and controls
Mahesh A Kumbhar1*, Srikala Bharath2
1Assistant Professor, Department of Psychiatry, Bharati Vidyapeeth Deemed University Medical College and Hospital Sangli, Maharashtra, INDIA. 2Ex-Professor, Department of Psychiatry, National Institute Of Mental Health & Neuro Sciences, Bangalore, Karnataka, INDIA. Email: kmaaol@gmail.com
Abstract Background: Psychiatric illnesses are associated with more medical comorbidities. This is significant in patients with schizophrenia and substance use. Lack of treatment, neglect, impaired self-care and stigma are few factors responsible for it. This is particularly true for older patients. Late onset psychosis is a under researched concept and needs more inputs. Hence, we have carried out this study. Methods: This is a cross sectional comparative study. Sixty-one patients with late onset psychosis and forty-two healthy controls were recruited. Extend of physical comorbidities was measured by using Cumulative index rating scale (CIRS). Also, association of various factors and CIRS score severity was assessed using appropriate statistics. Results: Physical comorbidities were significantly higher in patients with late onset psychosis than controls. Physical comorbidities were present in 55.09% of cases and 33.33% of controls (P value 0.037). Mean CIRS score which indicates overall burden of cumulative burden of physical illnesses was 4.18 and 0.33 among cases and controls respectively (P value <0.001). Earlier age of onset and duration of adequate treatment was associated with lesser physical comorbidities. Conclusion: Adequate evaluation and treatment of physical comorbidities is needed in patients with late onset psychosis. Early treatment of patients may result in lesser burden of medical comorbidities in these patients.
INTRODUCTION Psychiatric illnesses particularly schizophrenia impair persons functioning significantly. It leads to impairment in personal care. Patients with severe psychiatric illnesses have poor nutrition and neglect towards health. Also, accessibility of these patients for medical care is restricted. This may lead to increased incidence of chronic medical conditions. Patients with psychiatric illness have higher medical problems (Mpango et al., 2020)(Alrojolah et al., 2019; Zolezzi et al., 2017) The importance detecting and treating medical comorbidities in schizophrenia patients is often underrecognized(Jeste et al., 1996)(Batki et al., 2009). Among psychiatric illnesses Schizophrenia and substance dependence are more often associated with physical comorbidities (Batki et al., 2009; M et al., 2021) There are number of studies conducted which shows that Schizophrenia patients have more comorbid medical conditions than controls(Smith et al., 2013). Compared with normal population schizophrenia patients have shortened lifespan by more than a decade(Bitter et al., 2017). Compared to non-schizophrenic controls schizophrenia patients have more severe course of physical comorbidities, more number of emergency presentations, longer hospital stay, higher number of admissions and shorter survival period(Sundström et al., 2007)(Schoepf et al., 2014)(Šprah et al., 2017) There is lack of research in this area from India. As burden of chronic medical illnesses increases with age most of the research has been done on patients diagnosed schizophrenia early in life and assessed for comorbidities later in life. Late onset psychosis is considered when psychosis is diagnosed after 40 years of age. Late onset psychosis is having senile and degenerative aetiology. Thus, it may be associated with distinctive medical illnesses especially degenerative diseases. We have conducted this research to explore this unmet need.
METHODS This is a cross sectional comparative study. Study was carried out at National institute of mental health and neurosciences, a tertiary hospital Bangalore. Study was carried out between April 2010 and October 2011. Sixty-one consecutive cases of late onset psychosis and forty-two controls were recruited after taking informed and written consent. Patients with ICD 10 diagnosis of Schizophrenia, Delusional disorder and Unspecified nonorganic psychosis were recruited. Those with affective psychosis were excluded for homogeneity. Patients with age of onset after 40 years of age were only included and those having age of onset before 40 years of age were excluded. Patients with substance dependence in last 6 months were excluded. Controls with no psychiatric comorbidities were included. Patients and controls with dementia were excluded before recruitment. Data was analysed with the help of statistician. Continuous data was analysed using t test and discrete data was analysed using chi square test. P value less than 0.05 is considered significant.
RESULTS Table 1: Comparison of Physical Co-morbidity
* P ≤ 0.05; df = 1 Table 2: Comparison of CIRS scores
T test statistics* P≤0.05 Table 3: Common comorbidities between cases and controls
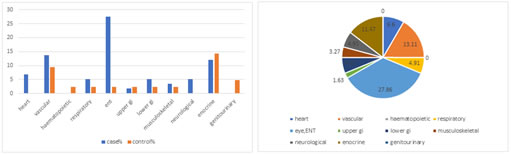
Figure 1: Comorbidities among cases and controls Figure 2: Distribution of comorbidities among LOP patients Table 4: Comparison of association of different variables between low and high CIRS score categories in Late onset psychosis cases
T test statistics* P≤0.05
Table 5: Comparison of association of different variables between low and high CIRS score categories in Late onset psychosis cases
DISCUSSION Physical comorbidities are present in 54.09% of patients with Late onset psychosis and 33.33% of controls. It is statistically significant (P value 0.037). The mean total CIRS (cumulative illness rating scale) score, which denotes the total amount of physical morbidity due to various illnesses was 4.18± 2.116for cases and 0.33±0.66 for controls and this was also significantly higher in cases than controls (P value 0.001). These high comorbidities in Late Onset Psychosis can influence the psychopathology by social isolation and increased amount of stress. Conversely psychiatric illnesses influence the decision to treat comorbidities in home or in institution. Also, psychiatric illnesses determine the self-care capacity and activities of daily living. Thus, presence of both psychiatric illness and high comorbid physical illnesses can interact and lead to higher rates of disability and institutionalization Earlier studies had reported increased prevalence of sensory impairment among the LOP (Cooper and Porter, 1976; Kay and Roth, 1961; Prager and Jeste, 1993). However, relation between other medical morbidities and LOP has not been established. In the current study various medical morbidities affecting different systems in LOP were scrutinized in a comparative manner. Nishant et al. found that hypertension, diabetes and anemia was more in schizophrenia patients(Nishanth et al., 2017). Studies on cardiovascular comorbidities have contrasting results (R et al., 2020; Smith et al., 2013). We found higher percentage of morbidities with Eye ENT and larynx, cardiac disease, vascular, lower gastrointestinal and respiratory categories of CIRS in the LOP group than the control group. We compared between low (<4) and high (≥4) CIRS score categories for various sociodemographic and illness related characteristics. No association was found for age, illness duration, education, Psychopathology at the time of assessment (PANSS score), and cognitive assessment. Age was expected to be associated with higher comorbidities. However, age was not a factor associated with medical comorbidities in our study. Similarly, duration of illness was not a factor associated with higher comorbidities. However, patients with low CIRS score had received treatment for significantly more duration (12.76 months) than those with high CIRS score (2.16 months) (P value 0.05). This may be because adequate treatment may improve functioning of the patient which leads to better self-care and management of medical illnesses. Thus, treating patients early and adequately may reduce the burden of medical comorbidities. Similarly, we found that patients with low score on CIRS have earlier onset of illness (53.38 years) than patients with high CIRS score (61.16) and it was statistically significant (P value 0.01*). Later age of onset is associated with higher medical comorbidities. Our study was able to highlight importance of assessing patients with late onset psychosis for medical comorbidities and adequate treatment for psychiatric illness. Limitations of our study are smaller sample size, hospital-based samples and cross-sectional study. Studies with higher sample size, community sample and longitudinal design may give better information. REFERENCES
Policy for Articles with Open Access
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home