Official Journals By StatPerson Publication
|
Table of Content - Volume 5 Issue 1 - January 2018
A study of prevalence of psychiatry morbidity in the relatives of the patients with suicide attempts in private setup at district level
Hemant J Baxi
Assistant Professor, Department of Psychiatry, Government Medical College, Gondia, Maharashtra, INDIA. Email: hemantbaxi@gmail.com
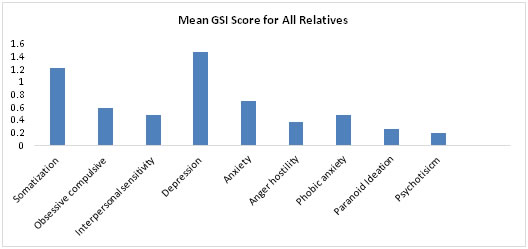
Abstract Background: World Health Organization (WHO) defined Suicide attempt as “any act arising from a deliberate wish of self-destruction, no matter whether the intention to die was strong, ambivalent or vague” Aims and Objectives: To Study Prevalence of Psychiatry Morbidity in the Relatives of the Patients with Suicide Attempts in Private Setup at District Level. Methodology: This study was carried out in private hospital in 32 consecutive patients who were referred to Psychiatry OPD in 5 months. The detailed interview was carried out at first psychiatry referral within 1 week of Suicide attempt by patient after medical stability. Intermediate care takers and relatives of Suicide attempts (41 Males + 42 Females) were also included for study, their Semi Structured interview was taken. It included Spouse, In-laws, Parent, Sibling who were staying with patient for at least 6 months. Suicide Intent Scale devised by Dr. Mirnal. Result: Depression was found to be the highest, GSI rising above 1. GSI for Somatization also approached higher than 1. Other were Anxiety and Obsessive -Compulsive were more than 0.5 Conclusion: It can be concluded from our study that Depression was most common psychiatry morbidity followed by Somatization, Anxiety. Obsessive -Compulsivewere lest common thus Neurotic symptoms were seen in maximum number of relatives. Psychotic symptoms were not prominent. Key Words: Psychiatry Morbidity, Suicide Attempts, Depression, Somatization, Obsessive -Compulsive disorders.
World Health Organization (WHO) defined Suicide attempt as “any act arising from a deliberate wish of self-destruction, no matter whether the intention to die was strong, ambivalent or vague”.1 Data on Suicide in India are available from the National Crime Records Bureau (NCRB; Ministry of Home Affairs). The Suicide rates vary widely across the different states of India, ranging from 1.1/100, 000 in Bihar to 35.6/100, 000 in Puducherry against the recent national average of 11/100, 000 in NCRB report 2013.2 In certain Indian studies, Prevalence rates of psychiatry disorders in Suicide attempters have ranged from 11.6% to 93%.3,4 Western studies on attempted Suicide also have reported high prevalence of psychiatry disorders.5-12 Underlying causes of suicidal behavior are complex and interacting with each other. Psychiatry problems such as Mood Disorders and Somatoform Disorders play important role in suicidal behavior. Understanding the importance of Family and Family members in the treatment outcomes, in the etiology; may be genetic susceptibility or common psychosocial environment. The psychiatry illness is a big problem of Family, so the role of family members is very crucial to understand the psychopathology of the Suicide attempts in the patients so, this study was carried out.
MATERIAL AND METHODS This study was carried out in Private hospital in 32 consecutive patients who were referred to Psychiatry OPD in 5 months. The detailed interview was carried out at first psychiatry referral within 1 week of Suicide attempt by patient after medical stability. Intermediate care takers and relatives of Suicide attempts (41 Males + 42 Females) were also included for study, their semi structured interview was taken. It included Spouse, In-laws, Parent, Sibling who were staying with patient for at least 6 months. Suicide Intent Scale devised by Dr. Mirnal (Phd, M.Phil), Retired Professor Department of Psychology in Nagpur University Campus, was used to detect the Psyco-pathology and severity of symptoms n relatives. This scale is in the Hindi Language. Scoring : the raw data is obtained by calculating the GSI of the dimensions in SCL 90 and Graph is plotted comparing the distress level for each dimension. General Symptomatic Index (GSI) = Sum of all items/ No. of Items. Table 1: Age and Sex wise distribution of the patients relative
Male were 41 and majority were in the age group of 31-40 i.e. 39.02%, followed by 41-50 24.39%, for Females were 42 and majority were in the age group of 41-50 - 40.48%,51-60
Figure 1: Mean SCL GSI Score for All Relatives
Out of the nine symptoms, Depression was found to be the highest, GSI rising above 1. GSI for Somatization also approached higher than 1. Other were Anxiety and Obsessive -Compulsive were more than 0.5 rest of the symptoms were less prominent, thus neurotic symptoms were seen in maximum number of relatives. Psychotic symptoms were not prominent.
DISCUSSION In India there has been a long tradition of involving families in the treatment of mentally ill relatives. In 1957, Dr. Vidya Sagar, the then superintendent of Amritsar Mental Hospital, involved the family members of the mentally ill in the management, by allowing them to stay with their patients in open tents pitched in the hospital campus. He showed that the patients recovered fast and were taken back home. Based on this principle, family wards were established in Christian Medical College, Vellore. The benefits were fast recovery, low relapse rates, and family members served as change agents in their community as they identified other patients and guided their family members to approach psychiatry centers for help.13This system of utilizing the family in the care of the patient had the additional advantage of relieving the Psychiatryally trained staff, particularly nurses and attendants, from routine duties.14 However, the hospital-based, resource-intensive and infrastructure dependent nature of such programs meant that they were not the most appropriate models to adopt.15It was suggested that some culture specific characteristics should be included in the Rehabilitation programs to make them more successful in the Indian context e.g. focusing primarily on families of patients, supporting them, helping them cope and easing their burden.16 Nearly four decades ago, Bhaskaran observed that more than 75% of the patients living in mental hospitals had no contact with any family member.17 He reported that the burden of care for a chronic illness, the reduced work output of the patient and the stigma attached to mental illness were the main reasons for the "unwanted patient". Gupta et al. 18report that although 70% of the patients in the Agra Mental Hospital had one or more family members, more than half of them did not have a single visit from a relative in the previous two years. Surveys of the mental hospitals have also shown that large numbers of long-stay patients have practically no contact with the family.19 As most of Studied only the patients this study included patients relatives Psychiatry morbidity. In our study we have found that Depression was found to be the highest, GSI rising above 1. GSI for Somatization also approached higher than 1. Other were Anxiety and Obsessive -Compulsive were more than 0.5 rest of the symptoms were less prominent, thus neurotic symptoms were seen in maximum number of relatives. Psychotic symptoms were not prominent.
CONCLUSION It can be concluded from our study that Depression was most common psychiatry morbidity followed by Somatization, Anxiety. Obsessive -Compulsive were lest common thus neurotic symptoms were seen in maximum number of relatives. Psychotic symptoms were not prominent.
REFERENCES
|
|
||||||||||||||||||||||||||||||||||||
 Home
Home