Official Journals By StatPerson Publication
|
Table of Content - Volume 6 Issue 2 - May 2018
Impact of depression on quality of life in asthmatic patients
Samyuktha G1, Ajaykumar Dhage2*
1Consultant Psychiatrist, Ameya healthcare HSR layout Bangalore, Karnataka, INDIA. 2Assistant Professor, Department of Psychiatry, M. R. Medical College, Gulbarga, Karnataka, INDIA. Email: veda26@gmail.com
Abstract Background: Depressive disorders and anxiety disorders are associated with worse asthma-related quality of life. Less asthma self-efficacy, more depressive symptoms, and unrealistic expectations predict worse asthma outcomes. These relatively unexplored patient-centered variables in asthma are potentially modifiable and may offer new ways to intervene to improve asthma outcomes. Aim: To study the impact of depression on quality of life in asthmatic patients. Material and Methods: A total of 70 asthmatic patients between the age group 18-65 years were studied. Patient Health Questionnaire (PHQ9) was used to screen the subjects for depression. Quality of life was assessed using Mini - Asthma Quality of Life Questionnaire (MINI-AQLQ). These scales were administered at baseline, 3rd and 6th months post-treatment. Appropriate treatment was given for depression and asthma as per standard guidelines. Asthmatics with depression and without depression were compared to assess the impact of depression on quality of life. Results: There was a significant negative correlation between depression and quality of life at baseline (r=-0.5090, P=0.003), 3 months (r=-0.7058, P<0.0001) and 6 months follow up (r=-0.8718, P<0.001). Asthmatics with depression had significantly higher MINI-AQLQ scores than asthmatics without depression at baseline and at 3 months follow up but not at 6 months follow up. Conclusion: Asthmatics with depression had poorer quality of life than asthmatics without depression at baseline and 3rd months follow up. At 6th months follow up quality of life did not differ between groups implying that treatment of depression played a role in improving the quality of life of asthmatics with depression. Screening all asthma patients for depression and treating them appropriately will improve their quality of life and asthma control. Key Words: Asthma, depression, quality of life, Patient Health Questionnaire, Mini - Asthma Quality of Life Questionnaire.
INTRODUCTION Depression in the present world is a major contributor of morbidity and mortality, with life-time prevalence in the general population of almost 20%. The Disability adjusted life years (DALY) of depression accounts to a total of 4.4% in all ages and gender. Years of Life Lived with disability (YLD) for all ages and both sexes attributable to depression is 11.9%1 Asthma is a chronic medical condition and a serious public health problem in industrialised countries, associated with significant morbidity and functional impairment, currently affecting ~300 million people globally.2 The Disability adjusted life years (DALY) of asthma is 1.4% and a total YLD of 2.1%.1 Recent reviews have found that depressive symptoms are more common in asthma patients than the general population.3,4 Nearly 50% of asthma patients have a positive screen for depressive symptoms.5 Depressive disorders and anxiety disorders are associated with worse asthma-related quality of life, but only depressive disorders are associated with worse asthma control.6 Less asthma self-efficacy, more depressive symptoms, and unrealistic expectations predict worse asthma outcomes. These relatively unexplored patient-centered variables in asthma are potentially modifiable and may offer new ways to intervene to improve asthma outcomes.7Literature search indicates a gross paucity of Indian research data pertaining to the issue of impact of depression on quality of life in asthmatic patients and thus there is a need to conduct further studies.
MATERIAL AND METHODS This prospective comparative study was conducted at the Departments of Psychiatry and Respiratory medicine in a tertiary care health center in Puducherry, India. Inclusion Criteria
Exclusion Criteria
Methodology Case selection Step 1
Step 2
Baseline measurements PHQ (Patient Health Questionnaire)
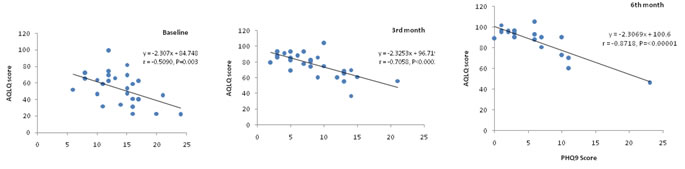
MINI AQLQ (Mini Asthma Quality of Life Questionnaire): It is a 15-item self-administered questionnaire derived from a 32 item AQLQ used to assessment the quality of life of asthma patients. In this scale 5 questions cover symptom domains, 4 questions assess activity limitation, 3 questions pertaining to emotional functioning and 3 questions for environmental stimuli. Follow up: PHQ, spirometry, ACQ, and AQLQ were repeated at the 3rd and 6th month of follow-up, to monitor the clinical courses of asthma and depression. Besides the administration of the aforementioned measurement tools at the 3rd and 6th month of follow-up, all subjects also attended routine outpatient follow-up in accordance with the standard protocols of the Departments of Respiratory Medicine and Psychiatry. Statistical Analysis: The heterogeneity χ2test was used to compare Group differences in categorical variables. One-way Analysis of variance (ANOVA) was used to compare the mean scores of MINI-AQLQ at baseline, 3 and 6 months post-treatment within each group. Data analysis was performed using the Statistical Package for Social Sciences (SPSS v 13.0), EPIINFO v. 6.0d and Microsoft Excel software. RESULTS A total of 62 adult asthma patients participated in the study. The median (mean) ages were 35.5 (39.4) and 42.5 (40.8) years for male and female patients respectively in Group 1 and the corresponding figures were 30 (means: 34.2 for male and 31.4 for female) years for both genders in Group 2. Neither the median (95% CIs about median for genders overlap for both the Groups) nor the mean (Student’s t-test for independent samples, P>0.5 for both comparisons) ages differ significantly between genders for both Groups 1 and 2. In both the Groups a large proportion of the participants were married (Groups 1 and 2: 78.1 and 70.0%) when compared to single (12.5 and 26.7%) or windowed 9.4 and 3.3%). However, the distributions of single, married and widowed patients were independent of Groups 1 and 2. The majority of the participants belong to lower upper lower income in both the Groups 1 (50%) and 2 (60%) followed by middle lower middle with corresponding figures of 31.3 and 26.7% respectively. A large proportion of the study participants were from rural (56.3% in Group1 and 60% in Group 2) compared to those from urban (43.7% and 40%). Of the 70 asthmatic patients registered initially for the study, 40 had depressive disorders giving an overall prevalence of 57.1% with 15.7, 24.3, 14.3 and 2.9% had mild, moderate, moderately severe and severe degree of depressions respectively. The prevalence of depression was higher among females (65.9%) than in males (42.3%). Among married persons the prevalence was 59.6% and that among unmarried, it was 38.5%. Of the five widowed persons four had depression. The prevalence was 51.9 and 60.5% among participants from upper or middle and lower socio-economic classes, 61.3 and 53.8% from urban and rural respectively. Statistical analysis showed that the prevalence did not differ significantly among different levels of socio-demographic variables (marital status, socio-economic classes and area of domicile; Heterogeneity χ2 test, P>0.05 for all comparisons).The somatic form and anxiety disorders were observed among 3 and 6 of the 70 patients giving an overall prevalence of 4.3 and 8.7% for the two forms disorders respectively. Asthmatic patients with depression Associations of PHQ9 score with MINI-AQLQ scores Figure 1 shows the associations of PHQ9 score with MINI-AQLQ score. The association of MINI-AQLQ score with PHQ9 score is negative and significant at base line (r=-0.5090, P=0.003), 3 months (r=-0.7058, P<0.0001) and 6 months post-treatment (r=-0.8718, P<0.001). The values of the correlation coefficients suggest that the strength of association increases negatively with increasing duration of post-treatment. It was observed that of out the 40 asthmatic patients with depression, only one patient had complete remission (PHQ9 score-0), eight had minimal depression (PHQ9 score- 1 to 3) and one patient did not respond to the treatment. The MINI-AQLQ scores at baseline, 3 and 6 months post-treatment for Group 1 are 3.5, 5.3 and 6.3 respectively.
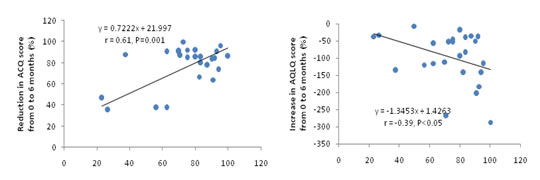
Figure 1: Association of PHQ9 score with AQLQ score at base line, 3 and 6-months post-treatment among asthmatics with depression Figure 2 shows the relationships of the extent of improvement in depression with quality of life and objective score of asthma control. PHQ9 score has a significant negative association with MINI-AQLQ (r=-0.39, P<0.05). The contribution of PHQ9 on MINI-AQLQ at 3 months post-treatment, 18.2%, was significant (F=6.44, P=0.017) but its contribution at 6 months post-treatment was not significant and 10.8% (F=3.16, P=0.087). Figure 2: Extent of improvements in AQLQ scores at 6 months post-treatment in relation to that of PHQ9 score
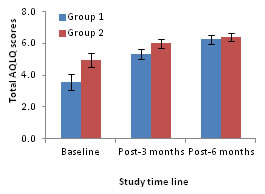
Asthmatic patients without depression The PHQ9 score had significant negative associations with the scores of MINI-AQLQ (r=-0.4940, P=0.005) at 3 months post-treatment. However, these variables did not significantly associate at baseline or 6-months post-treatment. The mean scores of PHQ9 and MINI-AQLQ significantly declined at 3 and 6 months post-treatment when compared to their corresponding scores at baseline (one way ANOVA followed by post-hoc test based on LSD, P<0.05 for all comparisons). Whereas the scores of MINI-AQLQ significantly increased from baseline to 3 and 6 months post-treatment (one way ANOVA followed by post-hoc test based on LSD, P<0.05 for all comparisons). Figure 3 compares the total MINI-AQLQ scores between Groups 1 and 2. The MINI-AQLQ scores at baseline, 3 and 6 months post-treatment for Group 1 are 3.5, 5.3 and 6.3 respectively and the corresponding values for Group 2 are 5.0, 6.0 and 6.4 respectively. The scores indicate that for both the groups the asthma quality of life improved as a result of treatment and the quality of life for Group 1 was almost similar to Group 2 at 6 months post-treatment. Statistical analysis showed that the quality of life differed significantly at baseline (Two-way ANOVA; P<0.001) and at 3 months post-treatment (P=0.5) but the difference was not significant at 6 months follow up (P=0.4). (Error bars are 95% confidence intervals)
Figure 3: Total AQLQ scores (mean) as a function of asthmatic patients DISCUSSION Through this study, an attempt was made to study the prevalence of depression among asthmatic patients attending a tertiary health care center, the impact of depression on quality of life. The study sample showed female preponderance, and male to female ratio was 1:1.5. In this study, group1 (asthma with depression) had more females than group 2 (only asthma). This is comparable to several other studies, where female asthmatic patients were more than males.6,8 Most of the subjects were married. The number of widowed and unmarried people in the study sample was small. The marital status did not differ between groups. However, other similar studies had a study population of predominantly single individuals.6,9The majority of the participants belonged to lower upper lower socio-economic class in both Group 1 (50%) and Group 2 (60%), followed by middle lower middle socio-economic class. This was similar to another study wherein most of the study population belonged to the lower income group.9 The socio-economic distributions of the patients were not significantly different between Groups 1 and 2.A large proportion of the study participants were from a rural area. Area of domicile was comparable between two groups. Area of domicile has not been specified in the reviewed studies. Majority (n=40) of the asthmatic patients registered initially for the study, had depressive disorders (prevalence = 57.1%). 15.7%, 24.3%, 14.3% and 2.9% had mild, moderate, moderately severe and severe degree of depressions respectively. This can be compared to similar studies which reported high prevalence of depression among asthmatics. A study by Yakar et al10 reported mild depression in 27% of asthmatics, moderate depression in 9% of asthmatics and severe depression in 7% of asthmatics. The prevalence rate reported in the literature varies from 8%6,11 to 55.01%.12 Contradicting this, a review done by Opolski et al3 reported mixed results as to whether persons with asthma are more likely to be depressed than those without asthma. Higher scores of MINI-AQLQ imply better quality of life and lower scores imply poor quality of life. The depression score is inversely proportional to quality of life scores among asthmatic patients. The values of the correlation coefficients suggest that the strength of association increases negatively with increasing duration of treatment. Higher scores of asthma are associated with low scores of quality of life. Association of depression with quality of life was significant at baseline, 3 months and 6 months post-treatment. A study by Deshmukh et al13 showed similar findings that depression symptoms independently showed a significant negative association with AQOL. Depression had a significant negative impact on quality of life among asthmatic patients. The quality of life scores among asthmatics with depression was always higher than that of asthmatic patients without depression. The difference between the two groups was significantly higher at baseline and 3rd month follow up but not at 6th months follow up. This finding implied that with treatment of depression, the quality of life of asthmatic patients with depression was similar to that of asthmatic patients without depression. Various studies had similar findings where depressive symptoms were associated with poorer asthma-specific quality of life.9,14 Other studies using different scales to assess quality of life of asthmatic patients with depression have reported lower quality-of-life scores.6,15 An extensive review of literature by Opolski et al3 revealed similar results. Thus, it can be safely inferred that depression does have a significant adverse impact on the quality of life of asthmatic patients. Moreover, treatment of depression in asthmatic patients improves the quality of life among asthmatics. The depressive scores could predict asthma quality of life scores at 3rd month follow up and its contribution at 3 months post-treatment was significant (18.2%), but its contribution at 6 months post-treatment was not significant (10.8%). Similarly, a study by Schneider et al16 found that depressive disorder predicted the AQLQ scale score. Mancuso et al9 reported that GDS scores had the greatest effects on patient-reported health-related quality of life, accounting for 36% and 11% of the variance, respectively, for the composite AQLQ. Asthma quality of life scores improved as a result of treatment. The quality of life for asthmatic patients with depression was poor compared to asthmatic patients without depression. However, at 6 months follow up quality of life of asthmatics with depression was almost similar to asthmatics without depression, implying that treatment of depression had a favorable impact on asthma quality of life. Two studies by Brown et al17,18 reported a reduction in depressive symptoms after treatment with Citalopram and Bupropion, which was associated with improvement in quality of life. Treatment of depression among asthmatics improves the asthma control and quality of life to a level similar to those without depression. CONCLUSION Depression has a significant adverse impact on the quality of life of asthmatic patients. Moreover, treatment of depression in asthmatic patients improves the quality of life among asthmatics. Depressive scores at baseline could predict asthma control (composite scores) and quality of life scores at 3rd month. Treatment of depression among asthmatics improves the asthma control and quality of life to a level similar to those without depression. The results indicate the need to screen all asthma patients for depression and other psychiatric co-morbidities and treat them appropriately to improve their quality of life and asthma control. Limitations of the study: One of the main limitations of this study was the relatively small size of the study sample. Lack of control group due to ethical issues limited our analysis regarding impact of treatment of depression per se on MINI-AQLQ. Only newly registered cases of asthma were included in our study. This limits the generalizability of the findings.
REFERENCES
|
|
 Home
Home