Official Journals By StatPerson Publication
|
Table of Content - Volume 10 Issue 2 -May 2019
Mangal Swathi V1, Suganthi C2*, Murugan T3
1Assistant Professor, Department of Anaesthesiology, Institute of Social Obstetrics And Government Kasturba Gandhi Hospital for women and children, Chennai, INDIA. 2Assistant Professor, Department of Anaesthesiology, Tamil Nadu Government Multi Super Specialty Hospital, Omandurar Estate, Chennai, INDIA. 3Professor, Department of Anaesthesiology, Government Kilpauk Medical College and Hospital, Chennai, INDIA. Email: dr.suganthi86@gmail.com
Abstract Background: Regional anaesthesia is the most commonly used technique for lower abdominal and lower limb surgeries as it is very economical and easy to administer. A number of adjuvants, such as opioids and alpha 2 agonists, have been studied to prolong the effect of regional anaesthesia which is of utmost importance for post operative pain relief. Also the quest for searching newer and safer anaesthetic agents has always been one of the primary needs in regional anaesthesia. Keeping these factors in mind, it was proposed to study the S (−)-enantiomer of bupivacaine, levobupivacaine and its effects when added with dexmedetomidine. Aim of the Study: The aim of the present study is to evaluate the effects of addition of fixed dose of Dexmedetomidine 50 micrograms to epidural 0.5% isobaric Levobupivacaine solution on the time of onset of sensory blockade to T10 level, Maximum level of sensory blockade and time taken to achieve that level, Onset of motor blockade, Degree of motor blockade achieved, time taken to achieve the same, Haemodynamic changes, Side effects, Intraoperative sedation scores, Duration of analgesia, sensory and motor blockade. Materials and Methods: Sixty patients of either sex belonging to ASA I and II in the age group of 25-45 years scheduled for infraumbilical and lower limb surgeries were randomly divided into 2 groups (30 each) Group A received 0.5% isobaric levobupivacaine 20 ml epidurally with 0.5 ml distilled water and Group B 0.5% isobaric levobupivacaine 20 ml plus 0.5 ml dexmedetomidine 50 micrograms. Results: Maximal sensory level(T4), maximal motor blockade (Bromage 3) were achieved with the addition of dexmedetomidine(50 micrograms). Duration of analgesia, sensory and motor blockade were prolonged when levobupivacaine is combined with dexmedetomidine epidurally. Conclusion: The use of dexmedetomidine 50 micrograms as an adjuvant to levobupivacaine in epidural/spinal anesthesia seems to be a good alternative to the use of opioids with minimal side effects. Key Word: Epidural anesthesia, Levobupivacaine, Dexmedetomidine, infraumbilical surgeries, lower limb surgeries.
INTRODUCTION Epidural anaesthesia and analgesia has always been one among the best-accepted techniques for lower abdominal and lower limb surgeries as it provides good sensory and motor block with contracted bowels retaining adequate spontaneous respiration, reduces the perioperative stress responses to surgery, provides hemodynamic stability.1 Bupivacaine is a long-acting, effective local anaesthetic used via epidural route but is associated with cardiotoxicity and neurotoxicity. The laevorotatory isomers were shown to have a safer pharmacological profile. The advantages of levobupivacaine over bupivacaine are decreased cardiovascular toxicity2 and there is also a relatively decreased motor nerve fiber penetration and block, thereby a decreased post-operative motor blockade and thus early ambulation of the patients can be achieved. Efforts to find a better adjuvant in regional anaesthesia are underway since long.3 Dexmedetomidine, made up of medetomidine’s dextrogyrous enantiomer, is currently considered a super selective alpha-2 adrenergic agonists prototype. Dexmedetomidine is 1600-folds more selective for the alpha-2 receptor than clonidine.4 It also has hemodynamic stabilizing effects and reduction of anesthetic drug requirements. Its epidural administration is associated with sedation, analgesia, hypnosis, and sympatholysis.
MATERIALS Sixty patients of either sex belonging to ASA I and II in the age group of 25-45 years weighing between 50-70kg with BMI ranging between 19-24 scheduled for infraumbilical and lower limb surgeries were randomly divided into 2 groups (30 each). Group A received 0.5% isobaric levobupivacaine 20 ml epidurally with 0.5 ml distilled water and Group B 0.5% isobaric levobupivacaine 20 ml plus 0.5 ml dexmedetomidine 50 micrograms. This study evaluated the time of onset of sensory blockade to T10 level, maximum sensory blockade achieved and time taken to achieve the same, onset of motor blockade, degree of motor blockade, time taken to achieve maximal motor blockade, duration of analgesia, sensory and motor blockade, hemodynamic changes, intraoperative sedation scores and side effects if any.
EXCLUSION CRITERIA
METHODOLOGY A randomized controlled double-blinded study was conducted in Govt Kilpauk Medical College Hospital and Govt Royapettah Hospital after obtaining proper Institutional ethical committee clearance. Sampling was based on the statistical record of surgical cases done at KMCH and GRH. According to the annual operative statistics, around 1200 surgical cases (lower abdominal and lower limb surgeries) have been performed (inclusive of both hospitals) over a period of 6 months. So based on the above data, out of 600 cases, 60 patients (30 each group) who fulfilled the inclusion criteria were chosen for the study over a period of 6 months with valid prior informed consent. Parameters Observed Were6,7: Baseline pulse rate, SpO2 at room air, noninvasive blood pressure. ardiorespiratory parameters were monitored continuously and recordings were made every 5 minutes until 30 min and at 10 min interval for the 1st and 2nd hour. Intraoperatively, the incidence of bradycardia (heart rate<50beats per minute) was treated with 0.6mg of injection Atropine IV and hypotension (systolic blood pressure falling more than 20% from the baseline value) was treated with injection Ephedrine 6 mg IV. Time interval between the end of the administration of anaesthetic and the onset of cutaneous analgesia at T10 was evaluated using midline bilateral pinprick every minute till complete loss of cutaneous sensation at T10 at which point surgery proceeded. Maximum sensory dermatome reached and time taken to achieve the same. Time of onset of motor block and degree of motor blockade was assessed using modified Bromage scale. Sedation scores were recorded just before the initiation of surgery and every 30 minutes using Ramsay 5-point scale. Duration of analgesia was recorded as the time interval from the completion of anesthesia to the time when the patient complains of pain at the surgical incision site with VAS score >3. Duration of sensory blockade was noted as time interval from the epidural administration of anaesthetic agent till the regression of sensory level to S1.Duration of motor blockade was noted as the time interval from the epidural administration of anaesthetic agent till regression of motor blockade to modified Bromage scale 0.During the surgical procedure, adverse effects like nausea, vomiting, dry mouth, dizziness, headache, respiratory depression, pruritis, and shivering were recorded. Any postoperative untoward side effects were noted for 48 hours. Statistical analysis: The results were tabulated using the Statistical Package for Social Sciences version 16. Appropriate statistical analysis of data was done using the following tests: Student t test for parametric data,Chi-square test for non-parametric data. P<0.05 was considered as statistically significant. Results on continuous measurements are presented on Mean SD and results on categorical measurements are presented in percentage(%). Chi-square test has been used to find the significance of study parameters on a categorical scale between two groups. Student t test has been used to determine the significance between two group means. RESULTS Time of onset of sensory block to t10: The time of onset of sensory block to T10 level was slightly lesser with group B (11.4 minutes) than group A (12.5 minutes) but was not statistically significant between the two groups with p-value is 0.224.
Graph 1 Graph 2 Graph 3
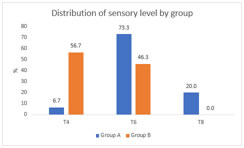
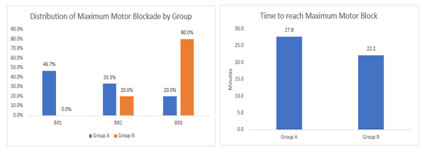
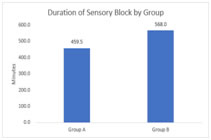
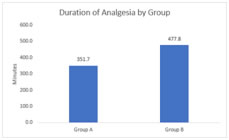
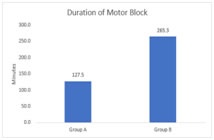
Graph 1: Shows that maximum sensory height; Graph 2: maximum motor blockade achieved; Graph 3: time taken to achieve maximal motor blockade; Graph 3: maximum motor blockade achieved; Graph 3: time taken to achieve maximal motor blockade; Graph 4: duration of sensory blockade; Graph 5: duration of analgesia; Graph 6: duration of motor blockade
Graph 1 shows that maximum sensory height attained was T4-T6 for group B and T6-T8 for group A with much statistical difference between the 2 groups (p-value-0.00004) Onset time of motor blockade: The time of onset of motor blockade was statistically significant between the two groups with a p-value of 0. 000 with group B showing shorter time of 14.5 mins than group A (19.33 mins). Graph: 2 maximum motor blockade achieved: Maximum motor blockade achieved showed statistical significance (p-value 0.0000) between the two groups with Bromage scale of 2 to 3 achieved in group B and Bromage scale of 1 to 2 achieved in group A. Time taken to achieve maximum motor blockade was significantly shorter with group B (22.17 minutes) compared to group A (27.83 minutes) which is statistically significant (p-value-0.006). Graph 4 shows that the duration of sensory blockade was prolonged in group B (568 minutes) when compared to group A (459.5 minutes) which is statistically significant, p value 0.000 Graph 5: Duration of analgesia was prolonged with group B (477.83 minutes) when compared to group A (351.67 minutes) which shows statistical significance with a p-value of 0.000. The duration of motor blockade is taken as the time for the motor blockade to return to Modified Bromage scale 0 which was statistically significant between two groups with P value of 0.000. Adverse effects and sedation score: Overall 30% of the patients in group B experienced adverse effects (dry mouth, nausea, vomiting including hypotension and bradycardia) which is statistically insignificant as compared to 16.67% in group A patients. None of the patients in group B had profound deep sedation or respiratory depression with the addition of dexmedetomidine.13,14,15 But hypotension/bradycardia (fall of >20% from the baseline) requiring treatment with Inj Ephedrine / Inj Atropine) were found to be statistically insignificant while comparing the two groups. Mode sedation score in group B (Dexmedetomidine group) was found to be 2 at all points of time as per Ramsay scoring.
DISCUSSION Regional anaesthestic techniques are superior to systemic opioids with regard to analgesic profile and adverse effects. Levobupivacaine is a preferred local anaesthetic due to its early onset and prolonged duration of sensory block, shorter duration of motor block, and lesser cardiac toxicity.8 In previous studies, it was concluded that the addition of dexmedetomidine to levobupivacaine produces effective analgesia and prolonged the duration of motor and sensory block along with better postoperative analgesia and fewer side effects.9This study compared the effects of addition of epidural dexmedetomidine (50 micrograms) to epidural 0.5% levobupivacaine 20 ml for infraumbilical and lower limb surgeries. Demographic parameters such as age, sex, height and weight showed no statistically significant difference between the two groups. Distribution of ASA status was also similar in both groups. Onset of sensory block was slightly earlier with group B (11.4 mins) but was not found to be statistically significant (p-value 0.224) .Maximum sensory height reached ranged from T6 to T8 in group A compared to T4 to T6 in group B with a p-value of 0.00004 which is statistically significant.10This study found that the mean time to onset of the motor blockade as 19.33 minutes in group A as opposed to 14.5 minutes in group B which is statistically significant with a p-value of 0.000. The onset time to motor blockade is slower with 0.5% levobupivacaine with mean onset time being 20+/-5 minutes but is hastened with the addition of dexmedetomidine (14.24+/5.52 minutes). Group B patients had a maximum degree of motor blockade (Bromage 3) than in group A patients (Bromage 2). The fall in heart rate in group B was maximum between 25 minutes to 100 minutes which showed statistical significance compared to group A. Similarly fall in systolic, diastolic and mean arterial blood pressure in group B was maximum from 5 to 60 minutes.11 Though there was fall in systolic blood pressure, fall below 20% baseline was statistically insignificant and also their mean arterial blood pressures never went below 60 mmHg which correlates with the study conducted by Kim JE, et al with the use of epidural dexmedetomidine. Also, postoperatively, heart rate and blood pressure remained stable in both groups.12 The stable hemodynamics can be explained on the basis of the concentration of levobupivacaine used and the selection of a suitable dose of dexmedetomidine. Overall 30% of the patients in group B experienced adverse effects (dry mouth, nausea, vomiting including hypotension and bradycardia) which was statistically insignificant as compared to 16.67% in group A patients. None of the patients in group B had profound deep sedation or respiratory depression with the addition of dexmedetomidine13,14,15
CONCLUSION This study concludes that combining dexmedetomidine 50 micrograms with 0.5% isobaric levobupivacaine epidurally helps in achieving a maximal sensory level of T4 to T6. Also, the onset time of motor blockade was shortened with the addition of dexmedetomidine and the maximal motor blockade was also intense with dexmedetomidine. Duration of analgesia, sensory and motor blockade were prolonged when levobupivacaine is combined with dexmedetomidine epidurally. Changes in hemodynamic parameters (blood pressure and heart rate) were very minimal in the dexmedetomidine group. Adverse effects encountered with dexmedetomidine were also acceptable with only mild discomfort to the patients. The use of dexmedetomidine 50 micrograms as an adjuvant to levobupivacaine in epidural/spinal anesthesia seems to be a good alternative to the use of opioids with minimal side effects.
REFERENCES
|
|
 Home
Home