Official Journals By StatPerson Publication
|
Table of Content - Volume 11 Issue 1 -July 2019
Hemodynamic stress response with laryngeal mask airway insertion and tracheal intubation in hypertensives patients undergoing mastectomy
Rekha N Solanki1, Nita D Gosai2*, Vidhi M Solanki3, Nishita M Shah4, Jayshree M Thakkar5
1Assistant Professor, 2Associate Professor, 3,4Resident Doctors,5Professor and HOD, ,, Department of Anaesthesia, Gujarat Cancer Research Institiude, B. J. Medical College, Ahmedabad-380016, Gujarat, INDIA.
Abstract Laryngeal and endotracheal intubation results in hypertension, tachycardia and arrhythmias and are more hazardous in patients with hypertension, myocardial infarction, coronary artery disease, cerebrovascular disease, penetrating eye injuries and intracranial lesion. Use of laryngeal airway requires neither visualisation of vocal cords nor the penetration of larynx with less sympathetic response and catecholamine release. Material And Methodology: Hundred Hypertensive (systolic BP </=140 mm Hg) female patients of 30-70 yrs of age , ASA I and II, with MPG I and II, posted for mastectomy were divided in two groups LMA (50),ETT (50). Heart rate, SBP, DBP were measured and post operative complication observed. Results: Heart rate, SBP and DBP increased in both group but in LMA group decreased to baseline in 3min and in ETT group decreased at 5min, Duration for insertion of LMA(12.76sec) was lesser as compared to ETT group(23.72sec). The incidence of postoperative sore throat, hoarseness, coughing is less in LMA group as compared to ETT group. Conclusion: hemodynamic response, was significantly in LMA group. Thus, LMA is a useful alternative to endotracheal intubation. Key Word: Laryngeal mask airway, Endotracheal intubation, Hypertension, Mastectomy, hemodynamic response.
INTRODUCTION Laryngeal and endotracheal intubation is the commonest method of securing definitive airway for administering anesthesia. This will increase sympatho-adrenal activity resulting in hypertension, tachycardia and arrhythmias.1,2,3,4 Although these hemodynamic response are more concerned in hazardous in patients with hypertension, myocardial infarction, coronary artery disease, cerebrovascular disease, penetrating eye injuries and intracranial lesion.4,5 Techniques that cause minimal oropharyngeal airway stimulation also attenuate the hemodynamic response.5 Use of laryngeal airway in place of endotracheal tube requires neither visualisation of vocal cords through laryngoscopy nor the penetration of larynx making the placement less stimulating than tracheal intubation and it may provoke less sympathetic response and catecholamine release.6 Thus this study was designed to compare hemodynamic stress responses to laryngeal airway insertion and endotracheal intubation, to evaluate the ease of laryngeal mask airway insertion, to evaluate the efficacy and usefulness of laryngeal mask airway over tracheal intubation and to study associated complications.
MATERIAL AND METHODOLOGY After getting institutional review committee approval and a written informed consent , a total of 100 hypertensive female patients undergoing mastectomy were randomly allocated to two groups: Inclusion criteria were hypertensive female patients of 30-70 years of age undergoing mastectomy , ASA I and II, MPG I and II, willing to participate in the study by giving consent, baseline systolic BP </= 140 mm Hg. Exclusion criteria were normotensive patients and hypertensive patients with baseline systolic pressure >140 mm Hg, ASA III and IV, MPG III and IV or having distorted or abnormal oral or supraglottic anatomy, h/o respiratory infections, difficult intubation ,angina , palpitations, syncopal attacks, hepatic and renal problems, regurgitation prone conditions, obese, full stomach patients and unwilling to participate in the study. Group LMA- LMA was inserted (50 patients) Group ETT- Endotracheal tube intubation was done (50 patients) Pre operative evaluation: All the patients were examined preoperatively and the procedures explained and written informed consent was taken. Routine investigations were done. They were kept NBM atleast 8 hrs prior to surgery. Premedication: Tab Lorazepam 1 mg given at 10 pm on the night before surgery. Antihypertensive drugs were given at 6 am on the morning of surgery. Monitoring: All routine monitors were applied before induction. Heart rate, systolic and diastolic blood pressure were noted. I.V line was secured, Inj. Ranitidine 1mg/kg and Inj. Glycopyrrolate Bromide 0.004mg/kg was given i. v Induction: Patients in both groups received preoxygenation via face mask for 5min.and were induced with inj. fentanyl citrate 2µg/kg, inj. Propofol 2mg/kg i.v and after confirming loss of eye lash reflex, Succinylcholine 2mg/kg i.v was given for Endotracheal tube (ETT) or Laryngeal mask airway( LMA) insertion. After the disappearance of fasciculations, LMA size 3 was inserted in group LMA and tracheal intubation with ET tube size 7.0/7.5 was done in group ETT. 2% Xylocaine gel was used as a lubricant for both the endotracheal tube cuff and LMA cuff. Air was injected into the endotracheal tube or LMA cuff as per recommendation. The position of LMA/ETT was assessed by chest rise on manual ventilation, equal air entry on auscultation and capnograph tracing. Duration of insertion / intubation was defined as the time from the start of insertion / intubation until inflation of cuffs. LMA insertion grading were done according to ease of insertion. Ease of insertion was classified as: Excellent (no resistance to insertion) Good (slight resistance to insertion ) Poor ( moderate resistance to insertion ) Impossible. Ease of intubation was graded I-IV according to the criteria of Cormack and Lehane.
Maintenance: O2 + N2O (50:50) + sevoflurane. No additional drugs were given till 5 mins. Before 30 mins of completion of surgery, Inj. Diclofenac sodium 1.5 mg/kg i.m and Inj. Ondansetron 0.1 mg/kg i.v were given. Reversal was done with Inj. Neostigmine 0.05mg/kg i.v + Glycopyrrolate 0. 4mg i.v. Observation: Heart rate, systolic and diastolic blood pressures are noted preoperatively and before induction and at Preintubation/insertion, intubation/insertion, 1 min, 3mins, 5mins after intubation/insertion. Intraoperative complications: Injury to tongue, lips, teeth was noted Post operative complications: Laryngospasm, regurgitation if any was accounted. Patients were asked about sore throat (constant pain independent of swallowing), hoarseness and or pain during phonation (as voice complaints). These along with cough were evaluated at 12 hrs and 24 hrs in both the groups. Statistical Analysis: Statistical analysis was done using graphed software. P value for age and height and time of insertion/intubation was calculated using student unpaired ‘t’ test. Statistical data for haemodynamic parameters was calculated using student paired ‘t’ test within the same group, between the groups using student unpaired ‘t’ test. P value for ease of insertion and intraoperative complications is calculated using chi –square test. P value for post operative complications is calculated using fisher’s exact test. P value<0.05 was considered significant. OBSERVATIONS AND RESULTS Table 1: Demographic data and mean duration of insertion/intubation of LMA and ETT
{ACE inhibitors= angiotensive converting enzyme inhibitors, ARBs= angiotension receptor blockers, CCBs=calcium channel blockers} The two groups were similar in terms of age, weight and anti hypertensive drugs with statistically insignificant P value. The mean duration of insertion of LMA and ETT was statistically significant (p<0.0001).
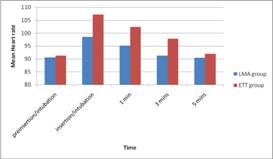
Figure 1: Comparison of Mean Heart rate between LMA and ETT groups The above chart shows changes in mean heart rate associated with LMA insertion and ETT intubation. Pre insertion/intubation values are taken as baseline values.
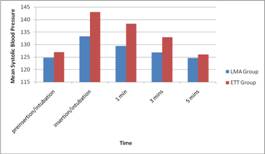
Figure 2: Comparison of Mean Systolic Blood Pressure between LMA and ETT Groups.
The above chart shows changes in Mean Systolic Blood pressure associated with LMA insertion and ETT intubation. Pre insertion/intubation values were taken as baseline values.
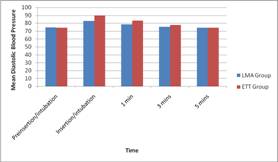
Figure 3: Comparison of Mean Diastolic Blood Pressure between LMA and ETT Groups The above chart shows changes in mean diatolic blood pressure associated with LMA insertion and ETT intubation Pre insertion/intubation are taken as baseline values.
The occurrence of injury to lip, tongue, teeth was more in ETT group(70%) compared to LMA group(20%) as p value is significantly higher (p<0.0001).
Table 4: Post operative complications
occurrence of sore throat was statistically significant (p-0.0439) at 12 hrs when compared between the two groups, which at 24 hrs is statistically insignificant (p-0.7858) The occurrence of hoarseness and coughing were also statistically significant in the ETT group at 12 hrs and 24 hrs.
DISCUSSION Laryngoscopy and tracheal intubation after induction of anaesthesia are associated with transient hypertension, tachycardia and arrhythmias. As mentioned earlier, laryngoscopic stimulation of oropharyngeal structures may be an important factor in the haemodynamic response associated with tracheal intubation. Laryngoscopy and intubation violate the patient’s protective airway reflexes, stimulate the pharyngeal tisseus and lead to a hypertensive ‘pressor’ response.10 These responses are transitory and not significant in normal individuals, but in patients with cardiovascular compromise like hypertension, IHD, cerebrovascular disease even these transitory changes in haemodynamic parameters can result in potentially harmful effects like left ventricular failure, pulmonary edema, myocardial ischaemia, ventricular dysrrhythmias and cerebral haemorrhage.11 Many pharmacological methods have been used to decrease these pressor response which include use of inhalational agents, lidocaine, opioids, direct acting vasodilators, calcium channel blockers, beta blockers but with little universal acceptance.7,8,9,12 Shribman concluded that‘ stimulation of the supraglottic region by tissue tension is the major cause of sympathoadrenal response and that placing a tube in trachea adds little further stimulation.13 Also methods like blocking glossopharyngeal and superior laryngeal nerves have been used to attenuate the cardiovascular response to laryngoscopy and endo tracheal intubation14 Non pharmacological methods like smooth and gentle intubation with a shorter duration of laryngoscopy, insertion of LMA in place of endotracheal intubation attenuated hemodynamic response.15 The effects of LMA cuff on the pharyngeal mucosa were explained by Marjot et al.. First, there was no sustained increase in transmitted lateral wall pressure and secondly, the transmitted lateral wall pressure decreased during the time the mask was insitu.16 Both the groups were comparable in terms of age, weight, antihypertensive medications being used by them. The time taken to perform laryngoscopy and ETT insertion was also more compared to time taken for LMA insertion. These results were similar to those of study done by Oczenski w et al.17 The response to ETT was significantly higher than to the insertion of LMA. This increased heart rate persisted for 5mins in ETT groups whereas it fell to baseline in LMA group by 3mins. SBP and DBP increase in both groups but the increase was sustained in ETT groups for 5min after the intubation as compared to LMA groups they returned to baseline levels at 3mins postinsertion. Wilson et al conducted study of 40 patients and compared cardiovascular response induced by insertion of LMA and ETT. The mean maximum increase in SBP after laryngoscopy and tracheal intubation and increase in maximum heart rate was similar, although heart rate remained elevated for longer time after tracheal intubation.18 Kiran et al also showed a highly significant increase in both SBP and DBP after airway instrumentation in both LMA and ETT. The values were significantly lower in LMA group than tracheal intubation at 1, 3 and 5mins.19 Higher incidence of trauma to lips, tongue and teeth was found following intubation with ETT as compared to LMA groups. Oral trauma was found more in laryngoscopy as compared to LMA group. There was greater and more significant incidence of a sore throat at 12hrs in ETT as compared to LMA group because of the placement of ETT to more sensitive tissues of the larynx and the trachea which causes sensitization to pain, thus contributing to a postoperative sore throat.20 It decreased to 18% in the ETT group as compared to 14% in the LMA group at 24 hrs. Christensen et al.21in there study reported a lower incidence of a sore throat. Horseness was observed to be more in the ETT group at 12 hrs and 24 hrs as compared to that in LMA group. Coughing was more in ETT group both at 12 hrs and 24 hrs as compared to LMA which was also supported by study of Holden et al22 in which intra-ocular pressure was measured before and throughout airway establishment with either LMA or ETT. No incidence of laryngospasm was found in our study which is in accordance with study of Masoomeh Tabari et al4. Regarding the possibility of gastric aspiration LMA was used for short duration in our study and we have no evidence of regurgitation in any patient. CONCLUSION:The LMA may be a suitable method for airway management of hypertensive patients with breast cancer undergoing mastectomy. LMA may be a good alternative to ETI with easier insertion and lower incidence of cardiovascular response.
REFERENCES
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home