Official Journals By StatPerson Publication
|
Table of Content - Volume 11 Issue 2 -August 2019
Management of a case of posterior reversible encephalopathy syndrome in antepartum period
Vidya Tharu K1*, Bhupendra Singh2
11st year resident, 2Assistant Professor, Department of Anaesthesia, S. N. Medical College and hospital, Jodhpur, Rajasthan, INDIA.
Abstract Posterior reversible encephalopathy syndrome (PRES) is a neurotoxic state coupled with a unique CT or MRI imaging appearance. It is recognized in the setting of a number of complex conditions like pre-eclampsia/ eclampsia, allogenic bone marrow transplantation, organ transplantation, autoimmune disease and high dose chemotherapy. It’s a clinical radiological entity characterized by headaches, confusion, visual disturbances, seizures and posterior transient changes on neuroimaging. We present a case with the complaint of acute onset of convulsions in the antepartum period. Patient was brought to the hospital in unconscious state, with GCS E2V2M4. On auscultation FHS was not detected and on Doppler USG, IUD was confirmed. Immediately patient was taken for LSCS under general anaesthesia with antiepileptic measure. Postoperatively patient was shifted to ICU for further management. Key Word: Encephalopathy, hypertension, convulsions, eclampsia
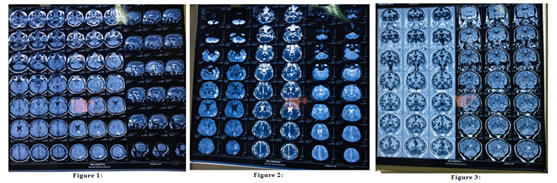
CASE HISTORY 21 year old female presented in the emergency department in unconscious state with GCS E2V2M4. Patient’s vitals were: pulse rate -130/min, BP-160/100 mm of Hg and oxygen saturation 85% on venti mask. Patient was having tachypnea, respiratory pattern was abdomino-thoracic, on auscultation B/L air entry was equal with no abnormal sounds and cough reflex was absent. Pupils were bilaterally mid dilated and sluggishly reactive to light. On neurological examination patient was responding to painful stimulus and plantar reflex was extensor bilaterally. On per vaginal examination os was closed. Patient was intubated and taken on ventilator support. All routine investigations were done .Liver enzymes and bilirubin were elevated with low platelet counts. ABG was within normal limits. History was provided by her maternal uncle. HOPI: Patient was apparently normal till seventh month of pregnancy. Suddenly she developed seizures with vomiting and recovery was uneventful. There were no residual signs or symptoms. Next morning she developed seizures again with frothing from mouth and up rolling of eyeballs and tongue bite, around 5-7 episodes over a period of 20 minutes and then she became unconscious. She was taken to a local hospital where symptomatic treatment was given. After 12 hours, she was referred to our hospital. Patient was intubated and USG was done which detected IUD. Patient was immediately taken for LSCS under GA. Post operatively patient was shifted to ICU. Past history: Patient did not receive any antenatal checkups. There is no history of diabetes, hypertension, TB, epilepsy and asthma or any chronic illness. Patient came to the emergency department with GCS E2V2M4, 18G IV lines were secured and immediate intubation was done. All routine blood investigations were done. She was treated with empirical antibiotics, IV fluids, sedation, inj labetalol and inj magnesium sulphate as anti-epileptic then she was shifted to OT for emergency LSCS under GA after detecting IUD on USG. In OT patient had two episodes of convulsions, which were controlled byinjthiopentone and inj midazolam. Intra operative period was uneventful. Post operatively patient was unconscious and had abnormal respiratory pattern, hence was shifted to the ICU where she was kept on ventilator support. Patient was given, antihypertensive, anti-epileptics, antibiotics and standard ICU care. Once the patient became stable MRI was performed, it showed- (figure 1, 2, 3) There are multiple areas of abnormal T2/FLAIR hyper intensity showing patchy restriction on diffusion sequence involving the left para sagittal frontal lobe. B/L parieto occipital and left high frontal region. Few of the lesions show focal areas of parenchymal infarction. There is no venous thrombosis. There is post ictal edema signals noted in the left hippocampal region.
Intravenous mannitol was added post-MRI and neurologist references was done. Platelet counts was 40,000 per microliter, liver enzymes and bilirubin were elevated. Chest X ray and ABG were within normal limits. Six units of RDP were transfused due to decreased platelet count. Her average BP was (SBP)130-145/ (DBP) 85-95 mm Hg. Patient was continued on labetalol infusion titrated according to BP. Pulse ranged from 80-100/min and SpO2 was 98-100%. On day 2, GCS –E2VTM4, patient continue on ventilator support and labetalol infusion with sedation and standard ICU care. Till day 4 same treatment was continued, every day sedation was stopped and assessment for weaning off from ventilator was done but it was not successful. On 5thday extubation was done. ABG was within normal limits. Patient was conscious but not well oriented. After two days, patient did not show any further improvement, so repeat MRI and neurological consultation was done. MRI showed-(figure 4, 5) There are multiple areas of abnormal T2/ FLAIR hyperintensities showing patchy restriction involving the left para sagittal frontal lobe. As compared to the previous report, findings were significantly reduced. There are multiple confluent areas acute infarction involving the left centrum semi ovale and left corona radiata, left trigone with contiguous up to left temporo occipital association area and occipital lobe on both sides. These findings were not appreciated on the previous scan. 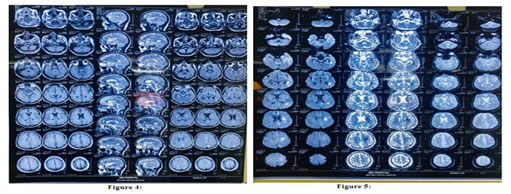
After two weeks of same treatment and all standard ICU care, patient became fully oriented and following verbal commands with no residual signs and symptoms of the previous illness. Then the patient was shifted to ward, observed and discharged after 5 days.
DISCUSSION Posterior reversible encephalopathy syndrome also known as reversible posterior leukoencephalopathy syndrome presents with rapid onset of symptoms including headache, seizures, altered consciousness, and visual disturbance 3,4. It is often but by no means always associated with acute hypertension3,4. If promptly recognized and treated, the clinical syndrome usually resolves within a week 4,5and the changes seen in magnetic resonance imaging (MRI) resolve over days to weeks 4,6. Commonly, PRES evolves over a matter of hours, with the most common presenting symptoms being seizures, disturbed vision, headache, and altered mental state4. More than 70% of patients with PRES are hypertensive, though a significant proportion have normal or only mildly raised blood pressure 5. The cause of PRES remains controversial, but the most popular theory is that severe hypertension causes interruption to brain autoregulation4,7. Cerebral blood flow is usually regulated by dilatation and constriction of vessels to maintain adequate tissue perfusion and to simultaneously avoid excessive intracerebral hypertension. Uncontrolled hypertension leads to hyper perfusion and cerebral vessel damage, resulting in interstitial extravasation of proteins and fluids, causing vasogenic edema7. Irreversible damage is seen at mean arterial pressures above 200 mmHg7.PRES is usually reversible, but permanent damage can occur if cerebral ischemia or hemorrhage occurs.8 An alternative theory is that PRES is a result of a systemic inflammatory state causing endothelial dysfunction 7. That postulate is supported by the observation that PRES is usually associated with a systemic inflammatory process such as sepsis, eclampsia, transplantation, and autoimmune disease. The differential diagnosis of PRES is broad, and history may be limited. Venous sinus thrombosis or subdural, intracerebral, or subarachnoid hemorrhage can all present with headache, seizures, reduced consciousness, and focal neurologic signs. Infective encephalitis or meningitis, particularly herpes simplex encephalitis, should be considered, and rapid treatment with intravenous acyclovir and antibiotics may be lifesaving while a diagnosis is still being pursued. It is important to consider the diagnosis of posterior circulation stroke, because its treatment (which may include urgent thrombolysis) and prognosis both differ from those in PRES. Basilar artery thrombosis can present with progressive neurologic deficits and can result in tetraparesis, coma, or locked-in syndrome. Radiographic features: Most commonly there is vasogenic edema within the parito-occipital regions, relating to the posterior cerebral artery supply. The edema is usually symmetrical. Despite being termed posterior, PRES can be found in a non-posterior distribution, mainly in watershed areas, including within the frontal, inferior temporal, cerebellar and brain stem regions9.Both cortical and subcortical including within the frontal, inferior temporal, cerebellar and brainstem regions There are three main imaging patterns
Other uncommon patterns of PRES in <5% include- purely unilateral, or “central” (brainstem or basal ganglia lacking cortical or subcortical white matter involvement). Parenchymal infarctions and hemorrhage are associated with PRES in respectively 10-25% and 15% of cases. Timely radiological imaging, diagnosis and administration of treatment is highly essential for the early recovery of the patient. If there is a delay in presentation to the higher center, associated co morbidities like in our case, it results in slow recovery and prolongation of the treatment. The improved knowledge and research about factors influencing the outcome of PRES will result in better early management, less morbidity and mortality.10 Delayed recognition of PRES can cause secondary complications such as intracranial hemorrhage, status epilepticus and ischemic infarction, therefore its of great importance to find out the cause triggering the seizures and minimize it as soon as possible by detecting the underlying cause.11,12
REFERENCES
|
|
 Home
Home