Official Journals By StatPerson Publication
|
Table of Content - Volume 11 Issue 3 -September 2019
A comparison between us guidance versus nerve stimulator-assisted us guidance on the efficacy of supraclavicular brachial plexus block for upper limb surgeries
Ranjan Niharika1, Mane Rajesh2, Yenni Shreedevi3*
1Post graduate, 2Professor, Department of Anesthesiology, KLE University’s Jawaharlal Nehru Medical College and Dr. Prabhakar Kore Hospital, Belgaum- 590010, INDIA. 3Assistant Professor, Department of Anesthesiology, Jawaharlal Nehru Medical College, Belagavi 590010, Karnataka, India Email: shreeyenni@yahoo.co.in, drrajeshmane@gmail.com, ranjan.niharika@gmail.com
Abstract Background: Ultrasound (US) guidance and peripheral nerve stimulator for supraclavicular brachial plexus block have enhanced the success rates of the block with excellent localization. Nevertheless, only few studies are present on peripheral nerve stimulator-assisted US guidance for brachial plexus block in upper limb surgeries. Objectives: To compare US guidance with nerve stimulator-assisted US guidance for supraclavicular brachial plexus block in patients undergoing limb surgeries. Method: Patients (n = 70) undergoing elective upper limb surgeries by supraclavicular brachial plexus block were involved. Randomization of patients was done to perform supraclavicular brachial plexus block either under US guidance (Group A = 35) or under nerve stimulation-assisted US guidance (Group B = 35). Demographic data including age, gender, and weight of the patients, were recorded. Time of performance of block, onset of sensory and motor block, duration of sensory and motor block, and hemodynamic changes (pulse rate, systolic and diastolic pressure), were the parameters compared between the groups. Chi-square test and unpaired t-test were used to analyse the data. Results: Demographic data was comparable in both groups. The mean time taken for the performance of block by eliciting paraesthesia was significantly less in Group B compared to Group A (5.87 ± 1.07 vs. 10.22 ± 2.11 min; P < 0.001). The mean time taken for onset of sensory (6.79 ± 1.04 vs. 9.28 ± 1.86 min; P < 0.001) and motor blockade (14.56 ± 2.53 vs. 17.69 ± 1.45 min; P < 0.001) was also significantly less in Group B compared to Group A. Conclusion: Nerve stimulator-assisted US guidance for supraclavicular brachial plexus block is a feasible technique in patients undergoing limb surgeries, in terms of reduced time taken for the performance of the block, and the onset of sensory and motor block. Key Words: US; Brachial Plexus Block; Nerve stimulation; Paresthesia;Paresthesia; Hemodynamics.
INTRODUCTION Regional anesthesia has gained popularity as an alternative to general anesthesia. It offers advantages such as less postoperative pain, less utilization of resources, excellent muscle relaxation, shorter post-anaesthetic care, and greater patient satisfaction.1,2 Moreover, it is highly acceptable in elderly and high-risk patients, with lower healthcare cost and better patient outcome.3 Brachial plexus block is commonly performed for upper limb surgeries as it provides superior quality of anaesthesia and analgesia.4 Several approaches are developed to block desired parts of upper extremities such as supraclavicular and infraclavicular blocks.5 Although, supraclavicular block is the most preferred approach to anesthetize brachial plexus.6,7 Peripheral nerve stimulation is considered as the gold standard for nerve localization in regional anesthesia because of its high success and low complication rate.8,9 However, the use of ultrasound (US)-guided brachial plexus blockade has superseded because of its potential advantages against other nerve localization methods. The advantages include accurate needle placement, rapid onset of block, dynamic visualization of anatomical structures, and needle with local anesthetic spread in real time. 8Although US ensures high block quality, there are few nerves that cannot be visualized due to its depth or osseous interference. In such cases, US identifies the local osseous interface to guide the block and the peripheral nerve stimulator guides the needle tip to the proximity of the nerve plexus with electric current lower than 0.2 mA.10 Moreover, US is strenuous to perform in obese individuals and in patients with distorted anatomy, as it results in incomplete blocks or failure.11 Hence, nerve stimulator-assisted US guidance was used to achieve more efficient nerve localization using a low-intensity electric current.12 Very few studies are present regarding the use of nerve stimulator-assisted US guidance for brachial plexus block in upper limb surgeries. Hence the present study is intended to compare nerve stimulator-assisted US guidance with only US guidance for performing supraclavicular brachial plexus block in patients undergoing upper limb surgeries.
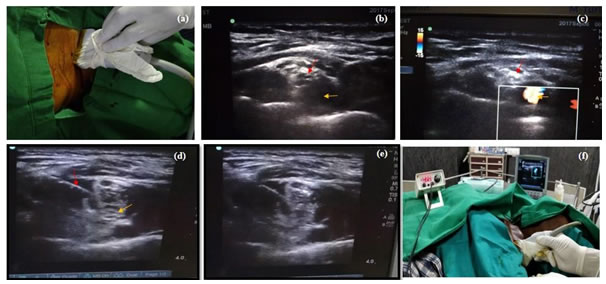
METHODOLOGY Design and patients The present one-year study (Jan–Dec 2017) was conducted at the Department of Anesthesiology of a tertiary care hospital. (Place of the hospital to be mentioned) Approval was obtained Institutional Ethical committee, before commencement of the study. Patients were briefed about the anesthetic procedure and a written informed consent was obtained, before their involvement in the study. Patients (n = 70) belonging to American Society of Anesthesiologists (ASA) grade I and II, aged between 18 and 60 years of either gender planned for elective upper limb surgeries under supraclavicular brachial plexus block were involved in the study. Patients with coagulation abnormalities, neurological deficits, infection at the site of block, severe cardiovascular and respiratory comorbidities, and patients allergic to local anesthetics were exempted from the study. All the patients were allocated randomly into two groups to receive supraclavicular brachial plexus block, either under US guidance (Group A = 35) or under nerve stimulator-assisted US guidance (Group B = 35). Randomization was done using computer-generated randomization list. Technique Routine pre-operative assessment and basic investigations were performed for all the patients. Adequate fasting of 8 hours was confirmed before the procedure. In the operation theatre, intravenous cannula was placed, and electrocardiogram, non-invasive blood pressure, and pulse oximeter (manufacture name to be mentioned) were monitored. On the operation table, the patient was placed in position for brachial plexus block via supraclavicular approach, supine position with head resting on ring, ipsilateral arm adducted, shoulder depressed, roller pack was placed in between the scapula, and the head was turned slightly too contralateral side. Local site was prepared under all aseptic precautions. After the needle was placed satisfactorily, both the groups received mixture containing 10 ml of 0.5 % Bupivacaine (manufacture name to be mentioned) and 10 ml of 2 % Lignocaine (manufacture name to be mentioned) with adrenaline. (Dosage and manufacture name to be mentioned) Following gentle aspiration, spread of drug and bulging of plexus were noted. For Group A, a high frequency linear array US (9-18 MHZ) was used. Clavicle, a proper landmark that is easily felt, was engaged to place the probe in supraclavicular fossa, superior to the clavicle and moved medially, laterally and in rocking fashion to pinpoint pulsating subclavian artery. The area lateral and superficial to subclavian artery was explored. The needle was inserted from the lateral side of the probe, first perpendicular to the skin and then at a shallow angle under the probe. The needle was then advanced under the US beam by plane technique till the plexus was observed with characteristic honeycomb appearance. Under US, the brachial plexus was observed as a bundle of hypoechoic round nodules (simulating cluster of grapes) just lateral and superficial to the subclavian artery. For Group B, the nerve stimulator was connected to the stimulating needle and set to deliver a current of 2 mA at 1 Hz frequency and 0.1 ms of pulse duration. Under US guidance, then the needle was inserted posteriorly, medially, and caudally. The needle was later slowly advanced under the palpating finger to elicit contraction of innervated muscle. Injection was administered when the elicited motor response of the fingers was obtained at 0.5 mA (Figure 1). STATISTICAL ANALYSIS SPSS v16 was used to analyse the data. Continuous data were represented as mean ± SD and the categorical variables were represented using the frequency table. Chi-square test was used to compare categorical variables. The Student unpaired t-test was used to compare continuous variables between the two groups. P < 0.05 was considered statistically significant. RESULTS AND DISCUSSION Figure 1: a) Position of the US Probe b) Brachial Plexus under US (red: Brachial Plexus; Yellow: Subclavian Artery) c) Doppler Mode for Confirmation of Subclavian Artery (Red: Brachial Plexus; Yellow: Subclavian Artery) d) Injection of Local anesthetic under US Guidance (Red: 23-Gauge Spinal Needle; Yellow: Brachial Plexus e) Brachial Plexus with Local Anesthetic f) Brachial Plexus Block with Nerve Stimulator-assisted US Guidance. The time taken for the performance of block, the onset of sensory and motor blockade, and duration of sensory and motor blockade, were the parameters noted. Hemodynamics were also monitored at regular intervals during the intervention. Sensory block, in all the nerve territories, was measured by pinprick test using a 3-point scale: 0 = sharp pin prick felt; 1 = dull sensation felt (analgesia); 2 = no sensation felt (anesthesia).13 Motor block was assessed by thumb — abduction (radial nerve), adduction (ulnar nerve), opposition (median nerve) and, flexion at the elbow (musculocutaneous nerve) on a 3-point scale for motor function: 0 = normal motor function with full flexion and extension of elbow, wrist and fingers; 1 = reduced motor strength but able to move fingers; 2 = complete motor block, with inability to move fingers. 14An inadequate block or failure of effect was noted and supplemented with general anesthesia. Any perioperative complications like hypotension, bradycardia, nausea, vomiting, respiratory distress, local hematoma, weakness, and hypoesthesia, due to nerve injury, pneumothorax, and surgical emphysema, were noted and treated.Demographic details of the patients are given in Table 1. Male predominance (71.42 %) was observed in Group B and female predominance (54.28 %) in Group A. Mean age was slightly higher among Group A patients whereas, mean weight was slightly higher among Group B patients. However, both the groups did not differ significantly with their age and weight (P = > 0.05).
Table 1: Demographic data of patients in both the groups
The mean time taken for the performance of block through eliciting paraesthesia was significantly less in Group B, compared to Group A (P < 0.0001; Table 2). The mean time taken for onset of motor and sensory blockade in Group B was significantly less compared to Group A (P < 0.0001; Table 2). Duration of motor and sensory blockade was significantly more in Group B, compared to Group A; however, not statistically significant (P > 0.05; Table 2).
Table 2: Comparison of block characteristics between both the groups
Group A: US Guidance; Group B: Nerve Stimulator-assisted US Guidance; #unpaired t-test;*statistically significant Hemodynamic changes including mean pulse rate and diastolic pressure did not significantly differ between both the groups (P > 0.05). While, mean systolic blood pressure significantly differed between the groups, before intervention and, at 0, 15, 20, 25, and 120 min, after the intervention (Table 3). Table 3: Comparison of hemodynamic changes between both the groups
*Statistically Significant
DISCUSSION In the present study, we compared and evaluated the efficacy of nerve stimulator-assisted US guidance with US guidance alone for performing supraclavicular brachial plexus block in patients undergoing upper limb surgeries. The evaluation was in terms of performance of block, time of onset of motor and sensory block, and duration of block. Supraclavicular block is most effective as well as the easiest to block brachial plexus.12 It blocks the entire sensory, motor, and sympathetic innervation of the upper extremities, below shoulder and facilities the upper limb surgeries.15 Hence, supraclavicular approach for the performance of brachial plexus blockade was preferred in our study. Whereas, few studies reported infraclavicular block is the rapidly preferred approach with high success rate.7, 16, 17In our study, US-aided nerve stimulation helped to lessen the time taken for the performance of the supraclavicular block, compared to US guidance alone. Similarly, in a study performed by Orenbough et al. 18 The mean time of performance of block using nerve stimulator was 6.5 mins and that with dual guidance was 1.8 mins. Based on our observation, it was found that the number of needle punctures were less in group B and patient comfort was better due to less procedural time. This finding was corresponding with Bomber et al. 19 who concluded that the combined use of US and nerve stimulation showed lower odds of unintended paresthesia (0.4 [0.2-0.8]; P = .007) compared to US alone. There were no vascular injuries observed in the either group, the use of Doppler and intermittent aspiration is always a rule whatever technique is employed.In our study, the faster onset of sensory and motor block was achieved in Group B compared to Group A. Shreshta et al.20, also found that the onset of motor block was 16 min in nerve stimulator-assisted US guidance group, which increased to 20 min in US guidance group alone. These findings prove that the use of US-assisted peripheral nerve stimulation significantly reduces the time needed for the onset of sensory and motor action. Distant spread of injectate from the site of action might be the reason for the delay in the onset of action in Group A whereas, accurate localization of the nerve bundle using nerve stimulation might be the reason for rapid onset of block in Group B. Moreover, dual guidance lowers the risk of pneumothorax, as the distance between skin and pleura can be easily measured under US before insertion of the needle and the nerve stimulator confirms the needle proximity to separate trunks. The mean duration of sensory and motor block was longer in Group B compared to Group A, however, not to a statistically significant degree. The longer duration effect of anesthesia might be due to precise delivery of medication closer to the brachial plexus. There was no significant change in the vital parameters such as pulse rate and blood pressure between the groups. Nevertheless, there are no similar kind of studies to support our findings. The sample size of the study was small. Hence, studies with sound sample size are recommended to validate the current findings and to reach definitive conclusion. The present combined technique (ultrasonography, neurostimulation, and injection pressure control) may be safer as well as successful than performing peripheral nerve block alone in less-experienced hands. In the future, machine recognition and 3-D imaging tools are also to be developed for accurate identification of nerve and to enhance the US-guided regional anesthesia. Liposomal mode of drug delivery for local anesthesia administration may prolong the duration of analgesia and, remove the requirement for perineural catheters, after the intervention.
CONCLUSION Nerve stimulator-assisted US guidance for supraclavicular brachial plexus block is a feasible technique in patients undergoing limb surgeries, in terms of reduced time taken for the performance of the block, and the onset of sensory and motor block. Moreover, this dual guidance technique reduces the patient discomfort and anxiety.
REFERENCES
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home