Official Journals By StatPerson Publication
|
Table of Content - Volume 11 Issue 3 -September 2019
Anaesthetic management in tracheobronchial foreign body aspiration: A retrospective analysis
Feny Thakkar1*, Jigisha Badheka2, Vandana Parmar3
1Senior Resident, 2Associate professor, 3Head of Department, Department of Anaesthesiology, P. D. U. Medical College and Hospital, Rajkot, INDIA. Email: drfenythakkar@gmail.com
Abstract Background and Aims: Foreign body in paediatric airway is an emergency with serious consequences that requires immediate intervention. The choices of inhaled or intravenous sagents for induction and maintenance, spontaneous or controlled ventilation may vary with patient condition. Excellent cooperation and communication between the endoscopist and anaesthesiologist are essential for successful outcome of the procedure. This analytic study was carried out with the aim to seek a safe and effective anaesthesia and ventilation management for removal of foreign body aspiration in the tracheobronchial tree. Methods: A retrospective analysis of 60 children with foreign body aspiration managed under general anaesthesia was done during period of two year. Results: We found age ranges from 5 month to 11 year and above out of which 68% patients were between ages 5 month to 3 year. More than half of patients had positive history of aspiration. Sixty percent patient’s having vegetable type of foreign body out of which peanut being the commonest 52%. Bronchoscopy results were positive in 90% of patients, two patients required tracheostomy for removal of foreign body. Breathlessness and cough were most common symptoms. All underwent rigid bronchoscopy for the removal of the foreign body. Conclusions: For early reorganization of foreign body detail clinical history and X-ray chest are essential. Peri operative morbidity and mortality can be reduced with proper surgical and anaesthetic management. Key Word: tracheobronchial foreign body aspiration.
INTRODUCTION Foreign body aspiration is a common problem in children [1] and its important cause of morbidity and mortality. 2 It is potentially life threatening event and may also cause chronic lung injury if not timelymanaged.3The use of computerized tomography, virtual bronchoscopy, and flexible bronchoscopy is increasing now a days but traditionally rigidbronchoscopy is the diagnostic “gold standard” 4.Rigid bronchoscopy for extraction of foreign body provides better quality of image and larger channel for removal of the foreign body, thick andcopious secretion and bleeding from the airway.5,6This procedure requires specific attention because both the anaesthesiologist and operator share the same airway.7Bronchoscopy requires team effort to obtain an optimal condition for safe anaesthesia and successful procedure. Various methods of ventilation are available and the best option should be selected based on the need of the procedure, condition of the patient, the equipment available and expertise of the bronchoscopist. There are various anaesthetic techniques for successful management of tracheobronchial foreign body aspiration in literature search, but there is no general agreement to which technique is optimal. Various methods for maintaining ventilation and oxygenation during rigid bronchoscopy are apnoeic oxygenation, spontaneous assisted or controlled ventilation, manual jet or high frequency jet ventilation. Controlled ventilation combined with Intravenous drugs and for paralysis depolarising or non-depolarising muscle relaxants are most commonly used method for rigid bronchoscopy. In patients with bronchopleural, bronchoesophageal and Broncho mediastinal fistula jet ventilation technique is used. We did this retrospective analytic study to review safe and effective technique for management in tracheobronchial foreign body aspiration.
MATERIAL AND METHODS We reviewed medical records of 60children who underwent bronchoscopy for suspected foreign body aspiration who were admitted in Otorhinolaryngology department at our hospital during period of two years. The following data were collected, age, sex, availability of history of foreign body aspiration, type, sign and symptomsand radiological findings. Preoperative assessment including complete medical history, physical examination with airway assessment and chest radiographs were obtained prior to bronchoscopy. General anaesthesia was given to all patients after written informed consent. The need of tracheostomy was also explained to relatives and consent for it was also obtained. In operation theatre, continuous monitoringdone with pulse oximeter, electrocardiogram and non-invasive blood pressure and end tidal co2.After securing intravenous line, patients were premedicated with inj. glycopyrrolate4-5µgm/kg,inj. hydrocortisone 2mg/kg, inj. dexamethasone 0.2 mg/kg intravenously and inj. midazolam 0.05–0.07 mg/kg as anti-anxiety in selected cases. Anaesthesia was induced with thiopentone sodium (4-5mg/kg) or ketamine(2mg/kg) and propofol (1.5-2mg/kg) after preoxygenation for 3-5 minute. After induction, a rigid bronchoscope can beinserted in a non-paralyzed patient, but only under deep sedation. Ventilation was continued by connecting Jackson ree’s circuit to the bronchoscope with oxygen flow rate of 8-10litre/minute. Patients were maintained by repeated injections of intravenous anaesthetics, inhalational agent sevoflurane(1 to 4%) or halothane (1 to 3%) with 100%oxygen and ventilation was assisted manually in case of desaturation. Spontaneous assisted ventilation during induction is commonly practiced for proximal foreign body. Muscle relaxation, if desired was achieved with inj. succinylcholine when required or by bolus or intermittent doses of non-depolarising muscle relaxants (atracurium).In this controlled ventilation technique, the bronchoscope was used like an endotracheal tube for positive pressure ventilation. Manual ventilation with bag may be needed in most cases with careful watch over chest expansion because of risk of circuit leak. During the procedure and when Spo2 fell below 70% both the lungs were ventilated by bringing the bronchoscope at carina and occluding the proximal end of scope. Once the foreign body was removed intermittent positive pressure ventilation was withheld till it was taken out from larynx. If the attempt was not successful same procedure was repeated after oxygenating the child. Following the removal of the foreign body, a check bronchoscopy was done to look for pieces of foreign body. Intubation was done only if spontaneous breathing was inadequate or the patient was in bronchospasm and could not maintain Spo2.Reversal of residual neuromuscular block was done with inj. neostigmine and glycopyrrolate or atropine. Once the airway reflexes had returned and child was awake the endotracheal tube was removed after thorough suctioning. Post operatively nebulization was done with bronchodilators and steroids. After that child was given oxygen through face mask until awake and was continued @2-4 lit/minto all the patients postoperatively and kept under observation for about 10-20 minutes and then shifted to recovery room.
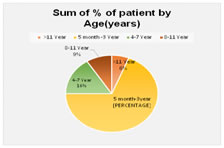
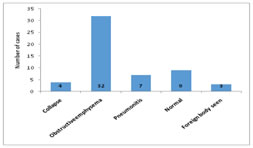
RESULTS Sixty cases were analysed for suspected foreign body aspiration. Most of patients 41(69%) were between the age group of 5 month to 3 year(Chart 1). Majority of them presented within 24-48 hrs of duration of history (Table 2). Table 1 shows that definite history of foreign body aspiration was present in 63.3% of cases. Other patients were presented with symptoms of breathlessness, cough, fever or wheezing. Common signs were tachypnea, unilateral diminished breath sounds and Rhonchi /crepitation (Table 3).The commonest radiological feature was obstructive emphysema in 34 cases. 10 cases were having normal chest X ray finding, 9 cases were with pneumonitis, 4 cases were having collapse and only 3 cases were having definitive foreign body (Chart 2).Vegetable foreign body was found in 60% patients whereas,40% patient had nonvegetable foreign body(Table 1). Bronchoscopy was positive in 54(90%) and negative in 6(10%) cases, only 2/60 patients require tracheostomy for removal of foreign body (Table 4).Table 5shows that 20(33.3%) patients were maintained on Intravenous and inhalational agents, in 34(56.6%) patients depolarising muscle relaxant was given and non-depolarising muscle relaxant was required in 6(10%) cases in which duration of procedure lasted more than 1 hour. Complication during bronchoscopy noted where hypoxia and post procedure airway oedema which were managed by mask ventilation in 3 cases and endotracheal intubation in 2 cases.
Figure 1: Distribution of age of the patient Figure 2: Radiological finding
Table 1: History and Type of foreign body ingestion
Table 2: Duration of presentation
Table 3: Symptoms and Signs
Table 4: Results of bronchoscopy and tracheostomy required
Table 5: Anaesthetic management with IV and Inhalational agent/Neuromuscular blockers
DISCUSSION Anaesthesia for rigid bronchoscopy in infants and children is a challenging procedure for anaesthesiologists as it is often difficult to maintain the airway for adequate ventilation and oxygenation due to presence of foreign body and secretion in the airway, along with the instrumentation and airway is to be shared. Foreign body aspiration occurs commonly between 5 months to 3 years of age. In our study 69% children were below the age of 3 years. Similar to our study Lone SA.et al8 and Kalyanappagol KT. et al9 found that majority of the children presenting with foreign body aspiration were under the age of 3-4 years. Most common site from which foreign body was removed was right main bronchus followed by left bronchus. In our study majority of them presented within 24-48 hrs of duration of history. Eroglu A.et al 10 studied Eighty two percent of the patients were symptomatic for less than 24 hours before admission and in 5% of cases, symptoms were present for more than one week. In our study history of foreign body ingestion was present in 63.3% of patients. The diagnosis is made by history of foreign body ingestion from parents and symptoms like cough, breathlessness, wheezing supported with chestxray and CT scan. Vegetable type foreign body absorb fluid and swell, oils from nuts cause localised inflammation and is more troublesome while sharp object can pierce the airway. In present study types of foreign body were vegetable type (peanuts, groundnut, other seeds or food particle)and non-vegetable type (plastic, metal and tobacco particles)in 36(60%) and 24(40%)patients respectively.11 Kavishvar N et al12 showed that vegetable foreign body was found in 87% patients where as 10% patient had non vegetable foreign body. Mukherjee M. et al13 also found Vegetable type foreign bodies were in 26/ 94 patients with suspected foreign body aspiration (FBA). In vegetable types peanut was the commonest foreign body found in 52% cases similar to other studies.14,15,16,17 ronchoscopy was positive in 54 (90%) and negative in 6(10%) cases. Two patients require tracheostomy for removal of foreign body. Kalyanappagol KT. et al9 found positive results of bronchoscopy in 206of 316 bronchoscopies were performed accounting for 2/3 of all suspected cases. The commonest radiological feature was obstructive Emphysema in 34 cases. Dhupar P.18 et al found the similar results that Obstructive emphysema was the most common radiological finding and normal X-ray chest does not rule out the possibilities of foreign body. It is difficult to have a single anaesthetic technique that can satisfy all these requirements. One should have an idea about probable location and type of foreign body before inducing anaesthesia. The review of the latest chest radiograph is helpful in determining the location of the foreign body and for evidence of secondary pathologic changes. Goals of anaesthesia 1) Adequate oxygenation 2) Controlled cardiorespiratory reflexes during bronchoscopy so there is no coughing laryngospasm or bronchospasm iii) Rapid return of upper airway reflexes. 3) Prevention of pulmonary aspiration. 4) Rapid return of upper airway reflexes after the procedure. Out of various ventilatory techniques oxygen can be delivered by insufflation at high flow rates (10-15 litre/min) by apnoeic oxygenation following hyperventilation with 100% oxygen to denitrogenate lung. Apnoea should not extend more than 3 minutes because carbon dioxide accumulation. Various intravenous induction agents (thiopentone sodium, ketamine or propofol) were used. Ketamine is preferred in paediatric patients in emergency were they may be with inadequate nill by mouth. It leaves the cough reflex intact, provides cardiovascular stability and prevents bronchospasm19.Maintenance done by repeated injections of intravenous anaesthetics, inhalational agent sevoflurane or halothane, intermittent positive pressure ventilation with 100%oxygen. In our study 20(33.3%) patients were maintained on Intravenous and inhalational agents with proximal foreign body. Chen HL et al20 showed that a total Intravenous technique with spontaneous ventilation was associated with a higher incidence of body movement, breath holding, and laryngospasm. Muscle relaxation, if desired can be achieved by succinylcholine or bolus or intermittent doses of non-depolarising relaxants (atracurium) to avoid excessive neuromuscular blockade at the end of a bronchoscopy. The disadvantage of this technique used in study that intermittent positive pressure ventilation may push foreign body further deep making its removal difficult which can be reduced by gentle ventilation with hand at lower pressure. The advantage of this technique is that muscle relaxation necessitate controlled ventilation, but also allows less inhalation agents requirement, prevents coughing, trauma and facilitates removal of foreign bodies through the vocal cords.21 In our study succinyl choline was used in 34(56.6%) patients and non-depolarising muscle relaxant was required in 6(10%) cases in which duration of procedure lasted more than 1 hour and subsequent endotracheal intubation needed. Method of ventilation at the end of procedure depends on respiratory gas exchange and the severity of airway edema. Instrumentation of the airway may produce mucosal swelling which can cause difficulty in breathing in postoperative period. Prophylactic use of humidified oxygen, nebulization with epinephrine and steroids are used to minimize postoperative mucosal swelling and oedema due to instrumentation of airway. Spontaneous ventilation with assisted mask ventilation was sufficient for uncomplicated cases. Intubation during emergence may be indicated for a marginal airway, pulmonary compromise, or residual neuromuscular blockade. Potential complications of rigid bronchoscopy include laryngeal edema, laryngotracheal lacerations, bronchial rupture, and bleeding. Detail clinical history, examination by signs and symptoms, X-ray chest with proper anaesthetic and surgical management are essential to ensure a high degree of success rate. All the cases observed till 48 hours post procedure and showed no mortality.
CONCLUSION Detail clinical history, examination by signs and symptoms, X-ray chest with proper anaesthetic and surgical management are essential for high degree of success rate.Various methods of ventilation are available and the best option should be selected based on the need of the procedure, the equipment available, and patient factors and expertise of the bronchoscopist. Limitations of our study was small number of patients and non-availability of flexible bronchoscopy and jet ventilation.
ACKNOWLEDGEMENT We wish to thank the department of Otorhinolaryngology of our hospital.
REFERENCES
|
|
 Home
Home