Official Journals By StatPerson Publication
|
Table of Content - Volume 11 Issue 3 -September 2019
Perioperative echocardiography in Ozaki’s procedure: An observational study - Single centre experience
Pushpa J1, Ananda Bhat2*, Parimala Prasanna Simha3, Prasanna Simha M4, Manjunatha N5
1Assistant Professor, 2Associate Professor, 3Professor & HOD, Department of Anaesthesia, SJICR, Bengaluru, Karnataka, INDIA. 4,5Professor, Department of Cardiothoracic and Vascular Surgery, SJICR, Bengaluru, Karnataka, INDIA. Email: anandadr@gmail.com
Abstract Objective: The aortic valve reconstruction using autologous pericardium described by Shigeyuki Ozaki et al is a novel surgical procedure. It can be applied to a wide spectrum of aortic valve pathology. We would like to report the peri operative echocardiographic data and intra operative transesophageal echocardiographic images of the patients who underwent Ozaki’s procedure in our center. Material and methods: This is a retrospective nonrandomized study involving twenty-two patients who underwent Ozaki’s procedure between January 2016 and October2017atSJICR, Bengaluru. The surgical procedure involves replacement of aortic valve by a valve reconstructed from autologous pericardium with three cusps. Preoperatively ten patients had aortic stenos is (AS) and twelve had aortic regurgitation. The aetiology of the aortic pathology was Rheumatic heart disease (RHD), Bicuspid aortic valve and senile calcific degeneration. Two of the patients were excluded because of incomplete echocardiographic data. Mean age of the study population was 29.4 years. Preoperative echocardiography showed an average peak gradient of 96.12 ± 22.7 mm of Hg and an average mean gradient of 62.75±14.3 mm of Hg in patients with AS. The average left ventricular ejection fraction was 52.8 ± 9%.Results: Postoperative echocardiography revealed an average peak gradient of 17.6 ± 9.75 mm of Hg and an average mean gradient of 8.85 ± 6.5 mm of Hg. After bypass, the leaflets opened and coapted well with no residual leak. No patient left the operating room with an aortic regurgitation of grade 2 or greater. Average postoperative left ventricular ejection fraction was 50.95 ± 9%. Conclusion: Our study cohort was very diverse as exemplified the by age range of patients and diverse etiology. We found that Ozaki’s procedure resulted in a neo tri-leaflet valve with elongated coaptation zone with minimal postoperative gradients and no significant aortic regurgitation in most of the cases. Key Word: Aortic valve replacement, Autologous pericardial reconstruction, Ozaki’s procedure
INTRODUCTION Aortic valve disease is commonly caused by degenerative atherosclerotic processes, congenital abnormalities or rheumatic disease. Open aortic valve replacement is the gold standard in the treatment of patients with severe aortic stenosis and aortic regurgitation. Mechanical prosthetic valves are used in younger patients because of their longer durability, whereas biological valves are preferred in elderly patients to avoid the need for oral anticoagulation1. On the flip side, there is limitation of durability with bio-prosthetic valves and disadvantage of anticoagulation with mechanical prostheses. Moreover, both prostheses cannot create good hemodynamics comparable with a native aortic valve. If a patient’s native aortic valve leaflets are reparable, standard valve repair may be the procedure of choice. But, this type of conservative repair is not always possible, especially for calcified Aortic stenosis in elderly patients2. Native aortic valve repair in children and adults with congenital valvular pathology is undergoing resurgence along with growing number of mechanical and biological substitutes. But there is no consensus over an optimal therapeutic solution. Furthermore, enthusiasm for the Ross pulmonary auto graft operation is undergoing reconsideration as longer follow-up has shown potential double semilunar valve disease; neoaortic insufficiency, future right ventricular outflow tract homograft reintervention, and risks of aortic root reoperation3. The Ozaki Aortic Valve reconstruction procedure using autologous pericardium is an innovative surgical procedure for any type of aortic valve disease, regardless of the age of the patient or the size of the annulus. The technique involves total resection of all three diseased cusps; hence the procedure can be applied to any type of aortic valve disease. By suturing three meticulously designed pericardial cusps onto the annulus; this surgery can address both adult and pediatric patients with aortic valve disease2. Ozaki et al postulate that independent replacement of cusps is more effective in preserving the natural motion of the aortic valve annulus and the coordination of the left ventricle, aortic annulus, and sinus of Valsalva and aorta which results in better hemodynamics2. The purpose of this study was to evaluate the hemodynamics of the newly reconstructed valve with perioperative transesophageal and transthoracic echocardiography
MATERIALS AND METHODS Study Design and Setting: The present study included all the Ozaki’s procedures performed over a period of one year ten months from January 2016 to October 2017, in Sri Jayadeva Institute of Cardiovascular Sciences and Research Center, Bengaluru. It was a retrospective nonrandomized study.A total of twenty-two patients underwent Ozaki’s procedure during the said period. There were ten patients with aortic stenosis and twelve patients with aortic regurgitation. Of the twenty-two patients, perioperative echocardiographic data was incomplete in two patients. They were excluded from the analysis. Data collection: This study reviewed hospital medical records, operative notes, echocardiograms and cardiac catheterization data in all patients undergoing Ozaki’s procedure. The data was checked for completeness. An echocardiographic examination was routinely performed prior to the patients’ discharge and resulting data were collected for each patient. The perioperative echocardiographic data include preoperative and postoperative transthoracic echocardiographic data along with intra operative transesophageal echocardiographic data and images when available. Surgery: All the surgeries were performed under general anesthesia. The patients were continuously monitored with five-lead electrocardiography, pulse-oximetry, and invasive measurement of arterial blood pressure and central venous pressure according to our routine protocol for patients undergoing open heart surgery. Transesophageal echocardiography (TEE) was performed throughout the procedure. After median sternotomy, the pericardium was dissected and treated for ten minutes with a 0.6% glutaraldehyde solution. In the meantime, the ascending aorta and the right atrium were cannulated, and cardiopulmonary bypass was established. After aortotomy, the diseased cusps were resected. The distance between each commissure was measured, using a special measuring device. The pericardium was subsequently cut according to a template that corresponded to the measured size. The cusps were then sewn along the annulus. The functionality of the substituted valve was assessed after coming off cardiopulmonary bypass by TEE. Postoperatively, the patients were routinely monitored in the intensive care unit. The surgery was performed by a single surgeon. The anesthetic protocol was comparable in all the patients. Cardiopulmonary bypass management protocol and postoperative patient management was standardized in all the patients. OBSERVATION AND RESULTS Demographic data: In the study population, fifteen were male patients and five were female patients. The patients belonged to all age groups. Highest number of patients was in the second decade of life. Table 1: Sex distribution of patients (Graphical representation of the same on right side)
Table 2: Age distribution of patients
Table 3: Aetiology of the Aortic Valve Disease
Eight patients had Aortic stenosis and twelve patients had Aortic regurgitation. The aetiology of the aortic pathology was Rheumatic heart disease (RHD), Bicuspid aortic valve andsenile calcific degeneration in eleven patients, eight patients and one patient respectively. Of the eight patients with Bicuspid Aortic valve, four patients had Aortic regurgitation and four had Aortic stenosis. Three of the four patients with Aortic regurgitation with Bicuspid Aortic valve had regurgitation following balloon aortic valvotomy. In eleven patients with RHD, three had isolated Aortic valve disease, among whom two patients had Aortic regurgitation and one had Aortic stenosis. One case with RHD had associated Moderate Mitral Stenosis. Seven cases with RHD had associated Severe Mitral Regurgitation. In cases with associated mitral valvular lesions, combined procedures were done. Nine out of the twenty procedures were combined procedures. One procedure was Ozaki’s procedure combined with CABG and one was Ozaki’s procedure combined with OMV. The rest were Ozaki’s procedure combined with Mitral valve repair. Perioperative Echocardiographic data: The average peak gradient in the cases with AS was 96.12 ± 22.7 mm of Hg. The average mean gradient in cases with AS was 62.75 ± 14.3 mm of Hg. The average preoperative left ventricular ejection fraction was 52.8 ± 9 %. Three patients had an LVEF of 40% or less. Table 4: Preoperative Aortic valve gradients in Aortic Stenosis
Table 5: Preoperative and Postoperative Left Ventricular Ejection Fraction Values
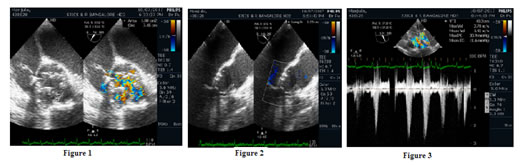
After coming off cardiopulmonary bypass the aortic valve coapted well and appeared like a standard tri-leaflet repair. After bypass, the leaflets opened and coapted well with no residual leak. Postoperative average peak gradient was 17.6 ± 9.75 mm of Hg. Postoperative average mean gradient was 8.85 ± 6.48mm of Hg. Two cases had gradients higher than mean and peak gradients of 15 and 30 mmHg (respectively). One case had a peak gradient of 30mm of Hg and mean gradient of 14mm of Hg. No patient left the operating room with an aortic regurgitation (AR) grade of 2 or greater. Postoperative average left ventricular ejection fraction was 50.95 ± 9%. Figure 1: ME Aortic valve short axis view of the reconstructed valve post Ozaki’s procedure –Planimetry of the valve area; Figure 2: ME Aortic valve long axis view of the reconstructed valve post Ozaki’s procedure- Coaptation Height measurement; Figure3: TG Aortic valve long axis view of the reconstructed valve post Ozaki’s procedure – Aortic valve gradient measurement. Table 6: Postoperative Aortic Valve Gradients
DISCUSSION Glutaraldehyde-fixed autologous pericardium is being used increasingly for aortic valve leaflet reconstruction in the presence of irreparable leaflet disease. In 1986, Love and colleagues first reported that scarring problem associated with the use of autologous pericardium can be eliminated by immersing it in 0.6% glutaraldehyde for ten minutes before use4. Based on recent models of aortic valve geometry, objective techniques have been developed to construct pericardial leaflets, making repair of more pathologies possible. Al-Halees et al published a series of autologous pericardial reconstruction for severe aortic valve disease in sixty-five young patients with good outcomes and average time to reoperation of sixteen years5. Duran reported his experience in fifty-one patients who underwent total aortic valve replacement with glutaraldehyde-treated autologous pericardium with a follow up of five years6. Ozaki et al reported a new technique of aortic valve reconstruction with glutaraldehyde treated autologous pericardium in 404 patients with a follow up of three and a half years. The technique can be applied to a wide spectrum of aortic valve diseases. The technique involves replacing all the three cusps of aortic valve by glutaraldehyde-treated autologous pericardium. Aortic valve normally, is a collection of different-sized cusps.As a result, pericardial cusps are created separately for each coronary cusp in Ozaki’s technique. The size of the new pericardial cusp as per Ozaki’s template is decided by three factors: the length of the cusp free edge, the intended larger coaptation zone and the margin for seams. Characteristics of Ozaki’s procedure are measurement of the distances between commissures as opposed to annular diameter, suturing the cusps directly onto the annulus and raising the contact point of the cusps to the commissural level2. In native aortic valve initially in the systole, native aortic annulus dilates, and then the valve cusps are fully opened by blood flow. The dilatation of aortic annulus at the beginning of systoleincreases the effective orifice area and decreases the stress tothe valve cusps. Suturing the cusps directly onto the annulus in Ozaki’s procedure enables the annulus to move naturally, replicating the natural mechanics which results inless mechanical stress. Reduced mechanical stress to the cusps lead to reduction in calcification and reduced postoperative pressure gradients. This operative method may also preserve the coordination of left ventricle, aortic annulus, sinus of Valsalva and aorta. As a result, Ozaki et al postulate that the post operative hemodynamics is excellent7. TEE helps in preoperative evaluation of the valve function, evaluating feasibility of repair and planning the aortic valvular reconstruction. A thorough echocardiographic assessment of the valve is necessary to assess the adequacy of the reconstruction, valvular structure, function, mechanics and presence of aortic regurgitation. It is helpful in coming off cardiopulmonary bypass and assessment of ventricular function. One of the primary roles of TEE in aortic valve reconstruction surgery is the immediate evaluation of the quality of valve function. The desired postoperative result is a flexible valve that opens well and is competent without any residual insufficiency. Mean and peak transvalvular gradients should be measured in the operating room to rule out significant stenosis. Mean and peak gradients more than 15 and 30 mmHg (respectively)are associated with an increased risk of developing aortic stenosis8. In Ozaki et al’s published study with 404 patients undergoing Ozaki’s procedure, postoperative echocardiography showed an average peak pressure gradient of19.8 ± 10.2 mm Hg one week after surgery and 13.8 ± 3.7 mm Hg three and a half years after surgery2. Ozaki et al published a series of aortic valve reconstruction for AS in 416 patients. On postoperative echocardiography, average peak pressure gradient was 21.2±10.7 mmHg at one week after surgery and 14.3±5.0 mmHg five and a half years after surgery7.Ozaki et al published a series of 108 patients aged less than sixty years with severe aortic valve disease with a follow up of four years. Of the 108 patients, fifty-one patients had aortic stenosis, seven patients had annulo-aortic ectasia, seven patients had infective endocarditis and forty-three patients had aortic regurgitation. Postoperative echocardiography showed an average peak pressure gradient of 14.8± 7.8 mm Hg one week after surgery and 12.8 ±3.1 mm Hg four years after surgery9.Komorov et al conducted a study to evaluate the effectiveness of Ozaki procedure and also to compare the hemodynamic efficiency with conventional prosthetic valve replacement. The study population consisted of three groups of patients with aortic valve surgeries. They compared patients who underwent Ozaki’s procedure with patients undergoing replacement with mechanical prosthesis and stented bio-prosthesis. Average mean valve gradient in the Ozaki group was 10.6 ± 3.2mm of Hgas compared to 13.7 ± 0.7 mm of Hg in the mechanical prosthesis group and 17.46 ± 0.8 mm of Hg in the bio-prosthesis group. They concluded that Ozaki’s procedure was associated with better hemodynamic parameters than aortic valve replacement by mechanical or stented biological prostheses10.Reuthebuch et al conducted a study to assess the results of Ozaki procedure in thirty patients. Average mean and peak postoperative gradients were 8 ± 3.55and 14.8 ± 6.21 mm of Hg respectively1. There was no significant change between the early and late postoperative grade of regurgitation and transvalvular gradients in these studies, which advocates for the stability of the technique at medium duration2,7,9.The absence of ischemic changes and the findings of echocardiographic valve competence and insignificant gradients are indicators of a reliable surgical technique6.On transesophageal echocardiographic evaluation, we found that two patients who underwent Ozaki’s procedure had more than mean and peak gradient of 15 and 30 mm of Hg respectively. One of the characteristics of Ozaki’s procedures is that contact point of the cusps is at the commissural level. By raising the contact point, the new cusps make the new coaptation zone longer than the native valve. The elongated coaptation zone minimizes postoperative aortic insufficiency2.We found this to be true in our cohort. Ozaki et al reported in their published data that most of the patients undergoing Ozaki’s procedure had less than mild aortic regurgitation postoperatively. The patients who developed significant aortic regurgitation had infective endocarditis with an incidence of 0.04%, 0.09% and 0.09%2,7,9. Reuthebuch et al reported in their study that at three monthspost-surgery, none of the patients in their cohort had aortic stenosis and regurgitation of the substituted valves was graded nil/trace in 85.71%, mild in 10.71%, and moderate in 3.57% of the patients1. In aortic valvular repair, the amount of residual AR by itself is not a satisfactory criterion for revision. The level at which coaptation occurs compared to the annulus and coaptation height are more predictive of presence of significant postoperative aortic regurgitation. The level of cusp coaptation should be above the aortic annulus. Ideally, the height of coaptation should be more than 9mm and reach the middle of the sinus of Valsalva8.If there is no residual AR and coaptation is above the aortic annulus, recurrent postoperative aortic regurgitation is highly unlikely8.Further studies are needed to define the threshold values for coaptation height and coaptation distance in case of aortic valvular reconstruction. Al Halees et al reported that seven patients out of sixty-five in the group which underwent autologous pericardial reconstruction developed endocarditis in his series which is asurprisingly high incidence5.Duranreported that two out of fifty onepatients had to undergo reoperation because of endocarditis which is nearly 5% prevalence6.In three of the studies published by Ozaki et al the incidence of infective endocarditis in patients who underwent Ozaki’s procedure is 0.04%, 0.09% and 0.09%2,7,9. Large scale studies with long term follow upare required to determine the incidence and to compare it with incidence of endocarditis in patients with prosthetic valve replacement. An additional factor is the cost of aortic valve reconstruction. The cost of Ozaki’s procedure is lesser than the cost of prosthetic valves. Apart from the higher initial costs, the cost associated with long-term anticoagulation, repeated monitoring of prothrombin time and repeated hospital visits can be avoided if autologous pericardial reconstruction procedures like Ozaki’s procedure are chosen11. Limitations of the study: The study is retrospective in nature and conducted at a single center. This study reports the early outcomes in a highly selected patient population. The follow-up period is short, and the study does not include comparison with patients undergoing alternative options for Aortic valve replacement. Because the study protocol was finalized at the end of the observation period, echocardiographic data was not complete in all patients. Further multi center randomized studies reporting outcomes in large number of patients will be required to demonstrate the superiority of this alternative technique.
CONCLUSION Ozaki’s procedure is feasible in a wide spectrum of aortic valve pathology including rheumatic disease. Our study cohort was very diverse as exemplified the by age range of patients and diverse etiology. We found that Ozaki’s procedure resulted in a tri-leaflet valve with elongated coaptation zone with minimal postoperative gradients and no significant aortic regurgitation in most of the cases. Adequate long-term follow-up will be required before this technique becomes main stream. Ozaki’s procedure could become a valuable management option in treatment of aortic valve disease.Intra operative TEE and perioperative echocardiography play a pivotal role in guiding case selection, surgical planning and in evaluating procedural success.
REFERENCES
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home