Official Journals By StatPerson Publication
|
Table of Content - Volume 11 Issue 3 -September 2019
Comparison of 0.25% bupivacaine and 0.375% ropivacaine in combination with fentanyl for modified radical mastectomy under cervical epidural Anaesthesia
Suganthi C1, Mangal Swathi V2*, Jayaraman3, Valli Sathyamoorthy4
1Assistant Professor, Department of Anaesthesiology, Tamil Nadu Government Multi Super specialty Hospital, Omandurar Estate, Chennai, Tamil Nadu, INDIA. 2Assistant Professor, Department of Anaesthesiology, Institute of Social Obstetrics and Government, Kasturba Gandhi Hospital for Women and Children, Chennai, Tamil Nadu, INDIA. 3Professor, Department of Anaesthesiology, Sri Ramachandra Medical College and Hospital, Chennai, Tamil Nadu, INDIA. 4Professor, Department of Anaesthesiology, Government Kilpauk Medical College and Hospital, Chennai, Tamil Nadu, INDIA. Email: drvmswathi@gmail.com
Abstract Background: Cervical epidural anaesthesia provides safe and reliable anaesthesia for head, neck and upper thoracic surgery. We used cervical epidural anaesthesia as sole anaesthetic technique to evaluate onset, extent, duration of analgesia and haemodynamic and respiratory status, reduction in blood loss and promotes early ambulation when used for neck, arm and upper thoracic surgery. Aim of The Study: To compare the effects of 0.25% bupivacaine and 0.375% ropivacaine in combination with fixed dose of fentanyl 50 μg for modified radical mastectomy under cervical epidural anaesthesia. To evaluate the time of onset of sensory blockade, time taken to achieve the maximum level of blockade upto T6,duration of sensory blockade, onset of motor blockade. Materials And Methods: Forty patients of ASA Grade I and II of female patients with the age group of 20-60 yrs, who were all posted for modified radical mastectomy were divided into two groups 20 in each, Group B received 0.25% Bupivacaine 10 ml with 25μg fentanyl and Group R received 0.375% Ropivacaine 10 ml with 25μg fentanyl as initial bolus and top up doses were given once the patient complained of pain. Results: The mean onset time of sensory blockade was found in group B 19±3.44 min and in group R 8.75 ±0.91 min. Mean duration of blockade in group B was 70±4.29min and in group R was 61 ± 5.75 min, Maximum level of blockade was obtained from C4-T6 dermatome level, haemodynamic parameters were within normal limits. Conclusion: When compared with epidural bupivacaine, epidural ropivacaine is better in terms of faster in onset of action, maximum level of blockade, reduced number of boluses and decreased requirement of rescue analgesia and adequate pain relief with stable haemodynamic parameters in the perioperative period. Key Words: Cervical epidural anaesthesia, Ropivacaine, Fentanyl, Modified Radical Mastectomy, Postoperative analgesia. INTRODUCTION Mastectomy for carcinoma breast is usually done under general anaesthesia. But nowadays there is growing interest to do this surgery under regional anaesthesia because of its more advantages when compared to general anaesthesia. Cervical epidural anaesthesia results in an effective sensory blockade of the superficial cervical plexus (C1 / C4) and brachial plexus (C5 / T1 – T2). It is used both intra operatively and in the treatment of postoperative pain. The approach to the epidural space at the C7-T1 interspace. The advantages are stable haemodynamic and respiratory status, control of pain extending into the postoperative period, early ambulation with reduction in stress response, blood loss and postoperative morbidity. Another main advantage is the avoidance of problems associated with the mechanical ventilation and also the avoidance of multiple drug exposure and its various side effects.
MATERIALS AND METHODOLOGY This study was a prospective randomized double blinded control trial. In this study, 40 female patients who were posted for modified radical mastectomy from the Department of General Surgery, Chengalpattu Medical College Hospital were analysed. The study was done over a period of one year (July 2013 – July2014). Institutional ethical Committee approval was obtained. Female patients who were posted for modified radical mastectomy in the age group of 20 – 60 years were counselled for Cervical Epidural Anaesthesia. The procedure was explained to the patient. Informed consent was obtained. Patients fulfilling the inclusion criteria and who gave consent were then randomly allocated to one of the study groups on the basis of computerized randomized list. In this study, who were all posted for modified radical mastectomy were divided into two groups 20 in each, Group B received 0.25% Bupivacaine 10 ml with 25μg fentanyl and Group R received 0.375% Ropivacaine 10 ml with 25μg fentanyl. To evaluate the time of onset of sensory blockade, time taken to achieve the maximum level of blockade upto T6 level, duration of sensory blockade, onset of motor blockade, changes in haemodynamic and respiratory parameters, effects in reducing blood loss, need of rescue analgesia and number of boluses needed during surgery, Intraoperative sedation scores and postoperative analgesia. EXCLUSION CRITERIA: • Patient refusal • Hypersensitivity to ropivacaine, bupivacaine • Hemodynamic instability • Local infection/inflammation • On anticoagulants • Bleeding disorders PARAMETERS MONITORED: Baseline Heart Rate, Non invasive Blood Pressure, Oxygen saturation, Respiratory Rate, Cardiorespiratory parameters were monitored continuously and recordings were made every 5 minutes until 30 min and at 15 min interval for the 1st and 2nd hour and thereafter every 30 minutes. Intra operatively the incidence of hypotension (systolic blood pressure falling more than 20% from the baseline value) was treated with injection ephedrine 6 mg IV. Time taken the onset of cutaneous analgesia at T6 level was evaluated using cold saline touch and midline bilateral pinprick every minute till complete loss of cutaneous sensation at T6 at which point surgery started. Maximum level of blockade obtained from C4- T6 and duration of blockade assessed by time interval between the administration of the agent till the regression of sensory level to C4. Duration of analgesia was recorded as the time interval from the completion of anaesthesia to the time when the patient complains of pain at the surgical incision site with VAS score >3. Motor block was assessed by modified bromage scale 0. Requirement of additional epidural top ups after the initial bolus were recorded for each agent and rescue analgesia along with epidural agent with intravenous sedatives also noted. Amount of blood loss was noted by weighing the gauze and pads used during the surgery and postoperative analgesia was given with Inj.Tramadol 100mg 12th hourly for next 48hours epidurally in the postoperative period. STATISTICAL ANALYSIS: The statistical analysis were done using SPSS-Statistical package for social sciences version 16 for windows. The profile of the cases were compared with the treatment allocation in order to check if there was any significant difference. Descriptive statistics are presented as mean± 1SD. Component bar and line diagrams were drawn as and when required. Chi square test for association was used to compare categorical variables between treatment allocations.
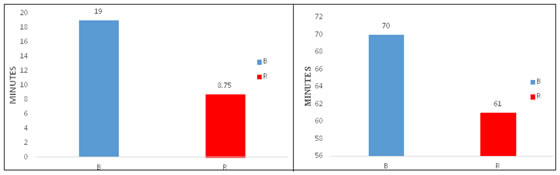
RESULTS AND OBSERVATIONS The initial patient characteristics such as age, weight, ASA grade, co-morbid conditions of the patients were noted. 1. DEMOGRAPHIC CHARACTERISTICS: The patient characteristics such as Age, Weight, ASA grade showed no significant statistical difference between the two groups. 2. SENSORY BLOCKADE ONSET TIME (student’s t test): The mean onset time of sensory blockade in group-B was 19 ± 3.44 minutes and in group-R was 8.75 ± 0.91 minutes. This variable showed that there was a statistically significant difference in onset time of sensory blockade between the groups (p=0.00)
Figure 1: Sensory blockade onset time Figure 2: Duration of sensory blockade
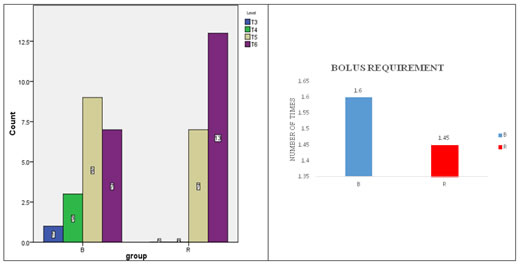
3. DURATION OF SENSORY BLOCKADE (student’s t test):The mean duration of sensory blockade in group-B was 70 ± 4.29 minutes and in group-R was 61 ± 5.75 minutes. This difference in duration of sensory anaesthesia in between both the groups was statistically significant (p=0.00) 4. SENSORY LEVEL (student’s t test): Out of 40 patients, 7 patients in group-B and 13 patients in group-R had T6 level. 9 patients in group-B and 7 patients in group-R had T5 level. 3 patients in group-B had T4 level. One patient in group-B had T3 level. The level of sensory blockade between the two groups was not statistically significant. Figure 3:Maximum Level Of Blockade Figure 4 5. MOTOR BLOCK (chi square test): Out of 40 patients, 20 patients in group-R had grade 0 and 19 patients in group-B had grade 0 and one patient had grade 1. This variable explained that development of motor blockade between the two groups had no statistically significant difference (p=0.5), chi square value was 1.03. Table 1
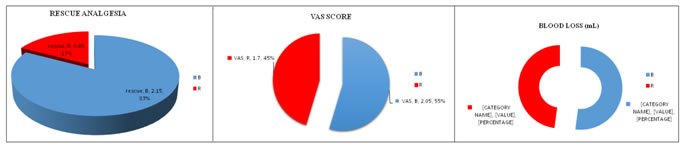
6. HAEMODYNAMICS: All the patients had their haemodynamics monitored continuously starting at baseline (before epidural), every 5 minutes for first 30 minutes, every 15 minutes for next 2 hours and thereafter every 30 minutes for next 1 hour. The minimum monitoring time was around 3 hours in both the groups. The following table will show the number of patients observed throughout the procedure. A) COMPARISON OF OXYGEN STAURAION (Student’s t test): The following table shows the changes in oxygen saturation in between both the groups. There was no significant statistical difference in both the groups (p>0.05) B) COMPARISON OF HEART RATE (Student’s t test): The following table shows the heart rate variations which showed no statistical difference in both groups (p>0.05) C) COMPARISON OF SYSTOLIC BLOOD PRESSURE (Student’s t test): The following table shows that the comparison of systolic blood pressure variations between the two groups showed no significant statistical difference (p>0.05) D) COMPARISON OF DIASTOLIC BLOOD PRESSURE (Student’s t test): The following table shows that the comparison of diastolic blood pressure changes between the two groups showed no significant statistical difference (p>0.05) 7. BOLUS REQUIREMENT (student’s t test):The number of epidural boluses given throughout the procedure in group-B was 1.6 ± 0.50 times and in group-R was 1.45 ± 0.68 times. No statistical difference was observed between the groups (p=0.43) 8. RESCUE ANALGESIA (student’s t test): Out of 40 patients, patients in group-B who had pain after giving epidural boluses required intravenous sedation was 2.15 ± 0.81times. In group-R patients, rescue analgesia given was 0.45 ± 0.51 times. This variable showed that there was a statistically significant difference in between both the groups (p=0.00) Figure 5 Figure 6 Figure 7 9. VAS (student’s t test): Out of 40 patients, 6 patients in group-B and 9 patients in group-R had VAS score of 1. 7 patients in group-B and 8 patients in group-R had VAS score of 2. 7 patients in group-B and 3 patients in group-R had VAS score of 3.There was noticeable decrease in the pain levels immediately after bolus. The pain levels did not go above visual analogue score of 3 in both the groups. The mean VAS score value in group-B was 2.05 ± 0.82 (55%) and in group-R was 1.7 ± 0.7 (45%). The pain score variation did not have any statistical significance (p=0.16). 10. BLOOD LOSS (student’s t test): The amount of blood loss observed in group-B was 102.25 ± 12.61 ml and in group-R was 94 ± 12.73 ml. This variable explained that there was no statistically significant difference in both the groups (p=0.04) 11. POST OPERATIVE ANALGESIA: The postoperative pain relief was given with tramadol for 48 hours with 12 hours interval. In both the groups it was given in 4 times. There was no statistically significant difference between the two groups.
DISCUSSION The sole use of cervical epidural anaesthesia for variety of surgeries involving neck and upper thorax carries many advantages like providing stable cardiopulmonary status and avoids the risk of airway manipulation, less blood loss thereby reducing postoperative morbidity and promotes early ambulation and less duration of hospital stay1,10,14. Neuraxial local anaesthetics and opioids act synergistically to provide neuraxial analgesia. This combination reduces the minimum local analgesic concentration (MLAC). Recently, ropivacaine has been studied for its efficacy in cervical epidural anaesthesia10,18. In our study, we used 0.25% bupivacaine of 10 ml and 0.375% ropivacaine of 10 ml combined with 25µg fentanyl to compare the effects of both the drugs in addition with opioids. The female patients are comparable with regards to age, weight in both groups. In this study we found that onset of sensory blockade was earlier in group R(8.75min)than in group B(19min),it was statistically significant(p=0.00) as correlated with the study conducted by Girdhari L Garg et al. Duration of sensory blockade also statistically significant (p=0.00) in group R(61min) than in group B(70min). Maximum level of blockade (upto T3-T6) between the two groups was not statistically significant. Development of Motor block between the two groups was not statistically significant (p=0.5) as correlated with the study conducted by Khanna et al. There was no significant rise in pulse rate or fall in mean arterial blood pressure in both group B and group R, found to be there was no statistically significant difference in haemodynamic parameters (p=0.05). The requirements of epidural top ups given throughout the procedure in group R (1.45min) and group B (1.6min), no statistical difference was observed between the two groups. The amount of blood loss observed in group R (94ml) and group B (102ml), there was no statistically significant difference in both the groups. Total number of Rescue analgesia given in group R (0.45times) was less than in group B (2.15 times), it showed that there was a statistically significant difference in between two groups. There was no statistically significant difference in VAS score and Postoperative analgesia in both groups. Addition of opioid with the local anaesthetic into cervical epidural space shown to provide high quality anaesthesia and analgesia as correlated by Libor et al. CONCLUSION This study shows that epidural ropivacaine is faster in onset, shorter in duration, maximum level of blockade and had decreased requirement of rescue analgesia and high quality anaesthesia and adequate analgesia in addition with fentanyl comparison with epidural bupivacaine. This study concluded that epidural ropivacaine is better than bupivacaine in the concentration used in our study. Ethical approval: The study was approved by the institutional ethics committee REFERENCES
|
|
||||||||||||||||||||
 Home
Home