Official Journals By StatPerson Publication
|
Table of Content - Volume 11 Issue 3 -September 2019
Effect of combination of scalp block and transversus abdominis plane block on postoperative quality of recovery after cranioplasty surgery: A prospective observational study
Sarasa K Sahoo1*, Debasis Kuanar2, Panigrahi Souvagya3
1Assistant Professor, Department of Anaesthesiology, Andaman and Nicobar Islands Institute of Medical Sciences and GB Pant Hospital, Port Blair, INDIA. 2Consultant, Department of Anaesthesiology, CARE Hospital, Bhubaneswar, INDIA. 3Associate Professor, Department of Neurosurgery, IMS and SUM Hospital, Bhubaneswar, INDIA. Email:drsarasa@yahoo.co.in
Abstract Background: Scalp block and transversus abdominis plane (TAP) block has been used successfully in patient undergoing craniotomy and various abdominal surgeries, respectively. Cranioplasty re-establishes the normal architecture of cranium and may play a role in normalising cerebrospinal fluid dynamics in patients who had undergone decompressive craniectomy in the past. The aim of our study was to compare the combined effect of scalp block and TAP block on postoperative quality of recovery and analgesia in patients undergoing cranioplasty surgery. Methods: Thirty-seven patients were included in this study, out of which eighteen patients in ‘Block Group’ received combination of scalp and TAP block before start of surgery, the rest nineteen patients in ‘NO Block Group’ did not receive any block. The primary outcome measure was the quality of recovery at 24 hr, measured using the 40-item quality of recovery questionnaire (QoR-40). In addition, comparisons between groups were also made for intra- and postoperative opioid consumption. Groups were compared using Student’s t test, Mann-Whitney U test or Chi-square test for different type of data. A p-value of <0.05 was considered statistically significant. Results: The median [interquartile range] aggregated global QoR-40 scores at 24 hr were significantly greater in the Block group, indicating good quality of recovery compared with the No Block group (186 [181-187] vs 156 [149-156] respectively; median difference, 30; P = 0.001). Intra- and postoperative opioid consumption was significantly higher in No Block group. No major block related complications were noticed during the study. Conclusion: We showed that the combination of scalp and TAP block in patients undergoing cranioplasty, produce superior analgesia resulting in improved quality of recovery in the postoperative period. Key Words: Cranioplasty, Scalp block, TAP block, QoR-40.
INTRODUCTION Decompressive craniectomy (DC) is a potentially lifesaving procedure for cases of refractory intracranial hypertension and commonly performed following post-traumatic brain swelling, intracranial haemorrhage and intraoperative brain swelling.1 Patients who survive DC undergo reconstructive cranial surgery in future. Cranioplasty is a surgical repair of defect of deformity of skull with the use of synthetic materials or more commonly with autologous bone flap, which was previously kept in the subcutaneous plane of anterior abdominal wall.2 Cranioplasty can protect the brain, and provide better cosmetic results but most importantly, improves the neurological functions by a decrease in local intracranial pressure and correction of CSF dynamics.3,4 Postoperative pain has been reported as moderate in this group of patients, requiring a combination of opioid and non-steroidal anti-inflammatory drugs as analgesics but opioids can interfere with neurological monitoring and associated with adverse effects.5 Peripheral nerve block, as a part of a multimodal analgesic technique, provide site-specific pain relief with few side effects and have been shown to be effective for improving the quality of recovery.6 Scalp block is a regional anaesthetic technique that involves blockade of the nerves that innervate the scalp, thereby providing analgesia for a considerable period of time with the potential of opioid sparing effect.7 Transversus abdominis plane (TAP) block is a peripheral nerve block designed to anaesthetise the nerves of supplying anterior abdominal wall (T6 to L1). It has been used successfully for variety of abdominal surgeries, such as caesarean section, hysterectomy, cholecystectomy, colectomy and hernia repair.8 Postoperative pain is an important component of quality of recovery after surgery; however, assessment of only pain outcomes after surgery does not completely describe the full dimensions of the quality of recovery. Among the multiple tools available to access the quality of recovery after anaesthesia and surgery, the 40-item quality of recovery questionnaire (QoR-40) is one of the validated multidimensional tools that has been shown to be suitable to assess the effect of interventions in anaesthesia that are aimed at improving the quality of recovery and improving patient satisfaction.9 The questionnaire measures various dimensions of recovery, including pain, nausea and vomiting, physical independence, physical comfort, emotional state, and psychological support.10 The QoR-40 scoring system is validated for many surgical facilities, including neurosurgery.11
AIM The main objective of this study was to determine the effect of scalp block along with TAP block on postoperative quality of recovery and analgesia in patients undergoing cranioplasty surgery. We hypothesised that the combined effect of both blocks would reduce postoperative pain and discomfort and thus improve the quality of recovery at 24 h as measured by the QoR-40 questionnaire. MATERIALS AND METHODS This prospective, observational, comparative study was carried out in a tertiary care centre from August 2015 to July 2016. After approval from the Institutional Ethics Committee of our hospital, written informed consent was obtained from all eligible patients. Patients of American Society of Anaesthesiologists (ASA) Grade I and II, aged 18-60 years of either sex, scheduled for cranioplasty, who had previously undergone unilateral frontotemporoparietal DC with the bone flap in the abdominal subcutaneous pocket, were considered for entry into the study. Exclusion criteria included patients with history of allergy to local anaesthetics, pregnancy and patients with known psychiatric or neurological condition that would affect the completion of the QoR-40 questionnaire. Patients who remained intubated at the time of first postoperative interview were also excluded. Patients were alternatively divided into two groups: Block group and No Block group. In the Block group, following administration of general anaesthesia, both scalp block and TAP block was performed on the ipsilateral side and in the No block group; none of the blocks were performed. Routine preparation of the patients was carried out as per our institutional standards for all patients undergoing cranioplasty surgery. Patients received standardized monitoring and an anaesthetic regimen consisting of intravenous fentanyl 2-3 µg/kg and thiopentone sodium 4-5 mg/kg, with vecuronium 0.1 mg/kg to facilitate endotracheal intubation. Anaesthesia was maintained with oxygen, air, and sevoflurane. Scalp Block: Six individual nerves; supraorbital nerve, supratrochlear nerve, auriculotemporal nerve, postauricular branches of great auricular nerve, greater occipital nerve and lesser occipital nerve, were blocked using a technique described by Pinoskyet al.12 The volume of local anaesthetic injected at each site was 2 ml of 0.25% bupivacaine. TAP Block: A linear, high frequency transducer was placed in a transverse plane, above the iliac crest and in the region of the anterior axillary line. The TAP was identified between internal oblique and transverse abdominis muscle and using in plane technique, a 22 gauge, short bevel, 100 mm Stimuplex® needle was advanced into this plane and 20 ml of 0.25% bupivaine deposited. Intraoperatively, all patient received ondansetron 0.15 mg/kg (maximum dose of 8 mg) IV towards end of surgery for postoperative nausea and vomiting (PONV) prophylaxis. A 20% increase in heart rate and/or blood pressure from the preoperative baseline was treated with fentanyl boluses of 25 µg at 2.5- minute intervals until vital signs returned to baseline.13 At the end of the surgery, sevoflurane was turned off and the neuromuscular blockade was reversed with neostigmine (50 µg/kg) and glycopyrrolate (10 µg/kg). Patients were monitored for the first 24 h postoperatively in a high dependency unit with standard monitoring facility including continuous oxygen saturation monitoring. Postoperative pain was assessed using an 11-point numeric rating scale (NRS; 0 = no pain, 10 = worst possible pain). All patients received IV paracetamol 1 gm every 6 h for 24 h as postoperative analgesia. Breakthrough pain was treated with bolus dose of Tramadol 50 mg IV and repeated every thirty minutes (maximum dose of 300 mg/24 h) to maintain NRS of < 4. Degree of sedation was measured by Ramsay sedation score; if awake, 1 ‑ anxious, agitated, restless, 2 ‑ cooperative, oriented, tranquil, and 3 ‑ responsive to commands only; if asleep ‑ 4 ‑ brisk response to light glabellar tap or loud auditory stimulus, 5 ‑ sluggish response to light glabellar tap or loud auditory stimulus, and 6 ‑ no response to light glabellar tap or loud auditory stimulus. PONV and was managed with additional dose of IV ondansetron 0.15 mg/kg and /or dexamethasone 8 mg.Patients were subjected to the QoR-40 questionnaire at 24 h after surgery by an independent investigator who was unaware of the group allocation. The questionnaire consists of 40 questions that examine five domains of patient recovery using a five-point Likert scale as follows: none of the time, some of the time, usually, most of the time, and all the time. The five domains assessed included emotional state, physical comfort, psychological support, pain and physical independence. Global QoR-40 scores range from 40-200 representing very poor to outstanding quality of recovery.10 We also recorded any block-related complications, such as intravascular injection of local anaesthetic, local anaesthetic toxicity. Other data recorded includes patient demographics, intraoperative fentanyl consumption, surgical data, postoperative pain score, sedation score, incidence of PONV, and the total tramadol consumption in the first 24 hr.The primary outcome measure was the global QoR-40 aggregate score at 24 hr after surgery. The secondary outcome measures were total opioid consumption during the intra- and post-operative period, side effects and complications.
Statistical analysis Groups were compared using Student’s t test for continuous data, Mann-Whitney U test for continuous non-parametric data and Pearson’s Chi-square test for categorical data. Continuous data are presented as mean (SD, Standard deviation), while non-continuous data are presented as median [IQR, Interquartile range]. Categorical data are reported as numbers. A p-value of <0.05 was considered statistically significant. SPSS® version 18 (Chicago, IL, USA) was used for all analyses.
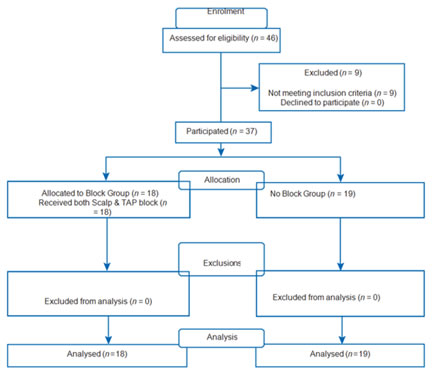
RESULTS Forty-six cases of cranioplasty were done during the study period, out of which nine patients were excluded in view of poor Glasgow Coma Scale because they could not follow the QoR-40 questionnaire. Eighteen patients received both the block (Block group) and nineteen patients did not receive any block (No Block group). The details of the conduct of the study are shown in Figure 1. There were no differences between the groups with regard to demographic and surgical duration but the total fentanyl use [225 (35) µgm vs 312 (65) µgm] during the intraoperative period was significantly less in Block group (Table 1). Median [IQR] aggregated global QoR-40 score at 24 h were significantly more in Block group, indicating better quality of recovery compared to No Block group (186 [181-187] vs 156 [149-158], respectively; median difference, 30; P = 0.001) and the patients in the Block group had significantly better median scores in all five domains (Table 2). The postoperative pain scores of were significantly lower in Block group at all points of time over first postoperative 24 h (Table 3). Cumulative tramadol consumption during the postoperative period was significantly more in No Block group at 24 h (Table 4). The incidence of nausea and vomiting were significantly less in patients who received both blocks, at 24 h after surgery, whereas the mean sedation score was comparable between the two groups at all points of times over the 24 h postoperative period and none of the patients had score <2 or >4 at any occasion (Table 4). There were no adverse events or serious complications reported in either group. Table 1: Patient characteristic and intraoperative data
*Calculated using Chi-square test or Student’s t-test as appropriate, ASA: American Society of Anaesthesiologists, SD: Standard deviation
Figure 1: CONSORT flow diagram Table 2: Quality of recovery score (QoR-40) at 24 h after surgery
Data are shown as median [interquartile range]
Table 3:NRS for postoperative pain up to 24 h after surgery
Data are shown as median [interquartile range]
Table 4: Postoperative data
*Calculated using Chi-square test or Student’s t-test as appropriate, SD: Standard deviation
DISCUSSION In our study the postoperative quality of recovery after cranioplasty was better in patients who received a combination of scalp and TAP block. The QoR-40 score was 30 points higher in the Block group compared to No Block group. There was improvement in all dimensions of QoR-40 scoring system in Block group (P<0.05). Intraoperative fentanyl and postoperative tramadol consumption was significantly more in No Block group. Patients in Block group had a better pain score in the first 24 h after surgery (p = 0.001). Fewer number of patients complained of PONV in Block group, probably due to overall decrease in opioid use in this group. All these factors contributed to a superior QoR-40 score in the group that received the combination of scalp and TAP block. Now days the focus of healthcare is more on improving the quality of recovery in patients undergoing various surgeries. The QoR-40 scoring system was developed by Myles et al. which is a valid, reliable and responsive tool for assessment of the quality of recovery after surgery and anaesthesia.10 It was further validated by Gornall et al. in their systemic review and meta-analysis.9 This scoring system has been used successfully for many different surgeries, including craniotomies.11 Scalp block was originally described by Girvin14 and modified by Pinoskyet al12, has been used successfully for awake craniotomies or along with general anaesthesia. Compared to scalp infiltration with local anaesthesia technique, it not only provides better postoperative analgesia but also reduces the total opioid intake during craniotomies.15,16 Rafi17 described the landmark bases technique for TAP block in 2001 and now days it is commonly performed, ultrasound guided with better localisation and deposition of the local anaesthetic with improved accuracy.18 We combined both the techniques in the Block group, resulting in significantly better analgesia during the intra- and postoperative period and improved QoR-40 score, compared to No Block group. There was no block related complications observed in our study which confirms the safety profile of scalp block and TAP block, even when used together. To the best of our knowledge, for the first time, combination of scalp block and ultrasound guided TAP block were used in patients undergoing cranioplasty and the superior analgesic and safety profile of these two regional techniques were demonstrated. There were certain limitations to our study. This was a prospective observational, non-randomised, single centre study and numbers of participants were limited. Patients in altered conscious state had to be excluded from this study as a reliable response to QoR-40 questionnaire was not possible from these patients.
CONCLUSION Pre-incisional, combination of scalp block and ultrasound guided TAP block, significantly improves the quality of recovery after cranioplasty. Both the block technique are relatively easy and safe to perform, and provides postoperative analgesia up to 24 h. However randomised controlled trials are necessary to validate these results.
REFERENCES
|
|
 Home
Home