Role of timing of fentanyl administration in attenuating cardiovascular response to laryngoscopy and endotracheal intubation
N Chiranjeevi1, Sai Suraj2*
1Assistant Professor, 2Senior Resident, Department of Anaesthesiology and Critical Care, Sri Venkateswara Medical College, Tirupati, Andhra Pradesh, INDIA.
Email: drchiranjeevinellore@gmail.com
Abstract Background: The laryngotracheal stimulation is known to cause reflex sympathoadrenal response with a marked increase in heart rate and blood pressure. Arrhythmias can be precipitated. One of the immediate and dramatic responses is that of the cardiovascular system – manifested by tachycardia, hypertension and dysrhythmias which may be catastrophic in patients with limited coronary / myocardial reserve. High dose were opiods were tried but with many complications so the present study was undertaken to evaluate small dose fentanyl and its optimal time of administration. Materials and Methods: This was double-blinded randomized controlled study, study wherein each patient was randomly assigned to one of 5 study groups by picking one sealed envelope containing the group name. Group NS - Normal Saline 5 ml (control group) group F1/5- Fentanyl 1.0 µg/kg 5 min, group F1/3- Fentanyl 1.0 µg/kg 3 min, group F 1.5/5- Fentanyl 1.5 µg/kg 5 min, group F 1.5/3 - Fentanyl 1.5 µg/kg 3 min before laryngoscopy and intubation. Heart rate, systolic blood pressure, diastolic blood pressure, and mean arterial blood pressure were recorded preinduction, postinduction after intubation were recorded and immediately at 1 min intervals thereafter, for 4 min i.e till t = 9 min. Results: Descriptive data presented as mean ± standard deviation .Statistical Analysis of the data was done using the Computer software package SPSS version 11. Hemodynamic data were analysed by One-way ANOVA (Analysis of Variance). “P” <0.05 was considered for statistical significance. The heart rate in group F 1.5/5 was significantly lower at all time intervals compared to all other groups. The rise in systolic, diastolic and mean BP was maximal in group F1/3 and minimal in group F 1.5/5, when compared to all groups. Conclusion: Fentanyl 1.5 ug / kg administered 5 min before laryngoscopy provides the best attenuation (not abolition) of this response. Dose lower than 1.5 ug / kg when given 3 min before laryngoscopy is Inadequate for effective attenuation of the pressor response. Fentanyl 1.5 ug / kg administered as a bolus IV dose, does not result in any serious cardio-respiratory complications.
Key Words: Fentanyl, Intubation, Laryngoscopy, Pressor Response.
INTRODUCTION
Laryngoscopy and endotracheal intubation are the most stressful conditions. It is a very powerful stimulus evoking a plethora of sympatho-adrenal stress responses. One of the immediate and dramatic responses is that of the cardiovascular system – manifested by tachycardia, hypertension and dysrhythmias. These changes occur approximately 30-45 seconds after laryngoscopy 1.This sudden stress may be catastrophic in patients with limited coronary / myocardial reserve. Several agents, were tried to reduce stress response like Deeper plane of anaesthesia with inhaled anaesthetics, Beta blockers, Local anaesthetics, Alpha agonists. High dose Opioids were found to completely abolish this stress response. High doses of 50 to 100 µg / kg (Lunn et al)2, which inevitably resulted in hypotension, bradycardia, respiratory depression and chest wall rigidity. These doses proved to be effective in Cardiac surgical patients who were anyway candidates for elective post operative ventilation. The advent of ambulatory surgery, fast-tracking in Cardiac surgery and the increasing geriatric population presenting for minor surgery posed a scenario of a higher likelihood of a fragile hemodynamic status in these patients. It therefore necessitated the search for lower doses of Fentanyl which could provide good protection against the intubation response and effective anti-nociception with minimal complications. Fentanyl, by virtue of its high lipophilicity, was found to have a fast peak clinical action, reducing gradually thereafter by redistribution (Scott et al)3. The strategy of using small dose Fentanyl coupled with accurate timing for optimum action was then explored so as to create a peak analgesic window within which if the Laryngoscopic stress were to be applied, effective attenuation of the stress response is possible (Ko et al)4. The small dose would then redistribute and not cause significant adverse effects thereafter. Different low doses of Fentanyl - 2 to 5 µg / kg had been compared, however hypotension, apnoea and bradycardia seemed to be inescapable complications. Hence, this study was undertaken to evaluate the optimal time of administration of a dose of Fentanyl effective enough to attenuate the cardiovascular stress response to laryngoscopy, such that the complications are kept within a safe clinical magnitude or totally avoided.
MATERIALS AND METHODS
The study population comprised of all patients aged between 20 and 30 years, admitted to Government General Hospital, tirupati for any elective non-cardiac surgery under General Anaesthesia. Only ASA I and II patients were included in the study. Patients with concurrent diseases like Hypertension, Diabetes mellitus, Ischaemic heart disease, Bronchial asthma, severe anaemia, those on anti-hypertensive / antidepressant medications and so on, are likely to have pre-existing hemodynamic compromise and are unlikely to respond normally to acute stress responses imposed on the cardiovascular system. Hence, hemodynamic parameters measured in such set of patients would be difficult to correlate and extrapolate to normal individuals. These patients were thus excluded from the study. On airway assessment, those patients in whom ventilation or intubation was expected to be difficult were also excluded. During Laryngoscopy, patients requiring more than two attempts or a total duration of more than 30 seconds at laryngoscopy were also to be excluded from the study. A total of 100 patients were studied; in 5 groups of 20 patients each. All patients were assessed in the ward the evening prior to surgery for fitness and Informed written consent was taken after explaining the procedure to them. All patients were premedicated with Tab. Diazepam O.2 mg / kg previous night and on the morning of surgery (7 am).In the Operation Theatre a peripheral intravenous cannula was placed and the patient was connected to monitors. Non-invasive Blood Pressure and Heart Rate were recorded on standard NIBP monitor. Continuous ECG was monitored on standard ECG monitor. Sp02 was monitored with standard Pulse Oximeter.
Statistical Analysis: Statistical Analysis of the data was done using the Computer software package SPSS version 11. Hemodynamic data were analysed by One-way ANOVA (Analysis of Variance) and subjected to Multiple Comparisons with significance of 0.05 for within and across group comparisons.
OBSERVATIONS AND RESULTS
A total of 100 patients were studied; in 5 groups of 20 patients each. No patient was excluded from the study due to either difficulty in ventilation or prolonged laryngoscopy. The mean age of the patients (Table-1) across the groups were comparable (p=0.056). Mean body weights of the patients (Table-1) were also comparable across the groups. Sex distribution among the groups are shown and in Table-1.
Table 1: Demographic Data
Group |
AGE (yrs)
(Mean ± 1 S.D) |
WEIGHT (kg)
(Mean ± 1 S.D) |
SEX DISTRIBUTION
Male Female |
NS |
34.2 ± 12.7 |
50.9 ±7.7 |
10 |
10 |
F 1/5 |
32.7 ± 10.1 |
48.0 ±6.8 |
8 |
12 |
F 1/3 |
33.8 ± 11.7 |
47.8 ± 5.7 |
6 |
14 |
F 1.5/5 |
29.5 ± 8.5 |
48.3 ±7.9 |
10 |
10 |
F1.5/3 |
38.6 ±11.1 |
48.1 ±8.3 |
6 |
14 |
HEART RATE (HR)
Comparing the mean heart rates at all time intervals across groups, group F 1.5/5 was found to be significantly different ( p=0.001) from Control group and all other groups. Comparing the heart rates at different time intervals in each group to their respective baseline values, at Induction there was no significant rise from baseline in any of the groups. At Laryngoscopy there was a significant rise in heart rate from baseline in all the groups except in groups F 1/3 (p= 0.078) (Fig-2a) and F 1.5/5 (p=0.070) (Fig-2b). At 1 minute post Laryngoscopy the rise in heart rate from baseline was significant only in the Control (p=0.004)At 2 min and 3 min post Laryngoscopy, mean heart rates were comparable to baseline values in all groups. At 4 min post laryngoscopy the mean heart rate in Group F1.5/3 was significantly lower than baseline value (Fig-2a 2b) Comparing the heart rates at a given time in any group to the respective Control group value; baseline and induction values in all groups were comparable to Control group. At Laryngoscopy, the heart rate in group F 1.5/5 was significantly lower than control (p=0.001), all others being comparable (Table-2). For each of the next 4 min post laryngoscopy the heart rates in all groups were comparable to control group value.
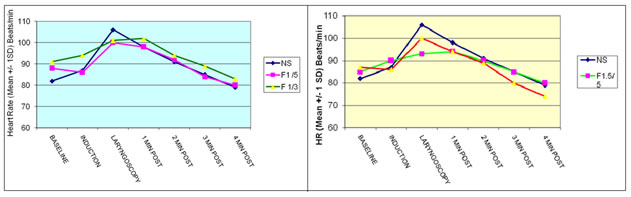
Figure 1a: Heart rate- fentanyl 1.0 ug/kg Groups Vs Figure 1b: Heart rate- fentanyl 1.5 ug/kg Groups Vs
Control Groups Control Groups
SYSTOLIC BLOOD PRESSURE (SBP)
Comparing the mean Systolic BP at all time intervals across groups, group F 1.5/5 was found to be significantly different from all other groups (p=0.000). Comparing the Systolic BP at different time intervals in each group to their respective baseline values, at Induction there was no significant rise from baseline. At Laryngoscopy the rise in SBP was significantly higher than baseline in all the groups except in group F1.5/5(p=0.066). At 1 min post laryngoscopy the SBP had returned to values comparable to baseline in all groups except in group F1/5 (p=0.011) and F1.5/3 (p=0.003) in which it was still significantly higher than baseline. (Fig-4). At 2 min post laryngoscopy the SBP in all the groups had returned to values comparable to baseline. At 3 min post Laryngoscopy, SBP was significantly lower than baseline in groups F1/ 5, F 1/3, F1.5/5 and F1.5/3. At 4 min post Laryngoscopy, except Control group all other groups had a significantly lower SBP compared to baseline. Comparing the Systolic BP at a given time in any group to the respective Control group value; baseline and induction values in all groups were comparable to Control group. At Laryngoscopy, 1 min, 2 min, 3min and 4 min post laryngoscopy the SBP in group F 1.5/5 was significantly lower than control group.
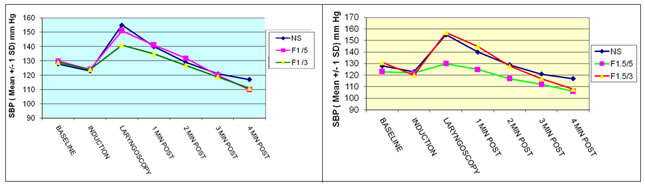
Figure 2a: SYSTOLIC BP-FENTANYL 1.0ug/kg Groups Vs Figure 2b: SYSTOLIC BP-FENTANYL 1.5ug/kg Groups Vs
Control Groups Control Groups
DIASTOLIC BLOOD PRESSURE (DBP)
Comparing the mean Diastolic BP at all time intervals across groups, group 1.5/5 was found to be significantly different from all other groups (p=0.000). Comparing the Diastolic BP at different time intervals In each group to their respective baseline values, at Induction there was no significant rise from baseline in any of the groups. At Laryngoscopy the rise in DBP was significantly higher than baseline in all the groups (p=0.000), however it was least in group F1.5/5. At 1min post laryngoscopy the DBP was still higher than baseline in all groups except F1.5/5 (Fig-6a, 6b). At 2 min post Laryngoscopy mean DBP in all groups were comparable to baseline. At 3 min post laryngoscopy the mean DBP in F1.5/5 is significantly lower than the baseline DBP. At 4 min post laryngoscopy, mean DBP in F1/5, F1/3, F1.5/5 and F1.5/3 were significantly lower than baseline DBP (Fig 6 a,b ).Comparing the Diastolic BP at a given time in any group to the respective control group value; baseline and induction values in all groups were comparable to Control group except in group F1.5/5 (p=0.021). At Laryngoscopy, 1 min, 2 min, 3min and 4 min post laryngoscopy the DBP in group F 1.5/5 was significantly lower than control group. At 3 min post laryngoscopy DBP in F 1/3 and F1.5/3 was also significantly lower than Control group.
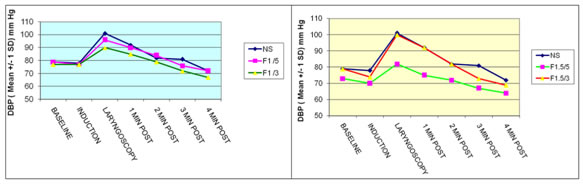
Figure 3a:DIASTOLIC BP-FENTANYL 1.0ug/kg Groups Vs Figure 3b: DIASTOLIC BP-FENTANYL 1.5ug/kg Groups Vs
Control Groups Control Groups
MEAN ARTERIAL PRESSURE (MAP)
Comparing the Mean Arterial Pressure at all time intervals across groups, group F 1.5/5 was found to be significantly different from all other groups (p=0.000).Comparing the MAP at different time intervals in each group to their respective baseline values, at Induction there was no significant rise from baseline in any of the groups. At Laryngoscopy the rise in MAP was significantly higher than baseline in all the groups, however it was least in group F1.5/5 compared to all other groups (Fig-8b). At 1 min post laryngoscopy the MAP was higher than baseline in Control .At 2 min and 3 post Laryngoscopy, MAP in all groups had returned to values comparable to baseline. At 4 min post Laryngoscopy, MAP in all groups was significantly lower than baseline except in Control group and F1/5.Comparing the MAP at a given time in any group to the respective Control group value; baseline and induction values in all groups were comparable to Control group. At Laryngoscopy and subsequent 4 mins post laryngoscopy the MAP in group F 1.5/5 was significantly lower than control group.
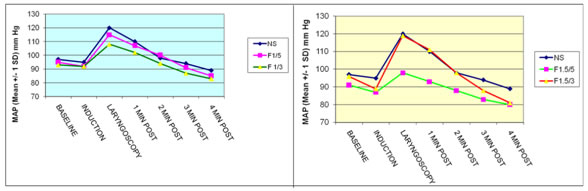
Figure 4a: Mean BP-FENTANYL 1.0ug/kg GROUPS Vs Figure 4b: Mean BP-FENTANYL 1.5ug/kg GROUPS Vs
Control Groups Control Groups
Table 2
Group |
Control |
F 1 / 5 |
Fl/ 3 |
F 1.5/ 5 |
F1.5/ 3 |
BRADYCARDIA (HR<60) |
0 |
0 |
0 |
2 |
0 |
TACHYCARDIA (HR> 20% BASELINE) |
17 |
9 |
12 |
5 |
10 |
HYPERTENSION (SBP> 20% BASELINE) |
8 |
8 |
7 |
1 |
11 |
HYPOTENSION (SBP < 70 % BASELINE) |
0 |
0 |
0 |
0 |
2 |
APNOEA |
0 |
o |
0 |
0 |
1 |
DYSRHYTHMIA |
0 |
0 |
0 |
0 |
0 |
Occurrence of a complication at any point in the study in a given case (excluding the baseline value) was done to assess effect of the given drug. Bradycardia was seen in 10 % cases in group F 1.5/5. Tachycardia was observed in 85 % cases in control group compared to 25 % in F 1.5/5 group. Hypertension was seen 40 % in Control group and 5 % in F 1.5/5. Hypotension was seen in 2 cases in group F 1.5/3. One patient who had apnoea, ceased breathing immediately after drug administration and resumed spontaneous respiration after ventilation was assisted once.
DISCUSSION
Laryngoscopy and Endotracheal intubation are associated with a host of sympathoadrenal stress responses manifested as sudden hemodynamic disturbances characterized by tachycardia, hypertension and dysrhythmias. Though normal healthy individuals can withstand this hemodynamic stress, in patients with diminished coronary reserve and occult cerebral aneurysms catastrophic complications are possible5,6.Even though lower doses of Fentanyl were able to attenuate the pressor response the most important factor seems to be the timing of administration of this bolus dose so that the laryngoscopic stimulus coincides with the peak anti-nociceptive action of the drug and so in our study we attempted to assess the efficacy of two low doses of Fentanyl viz. 1.5 µg / kg and 1.0 µg / kg administered at two different time intervals before laryngoscopy viz. 3 and 5 min prior. Kautto et al7 had demonstrated a similar pattern of response with Fentanyl 2 µg / kg, with the hemodynamic response peaking by 30-60 sec after laryngoscopy and reaching baseline values by 3 min. Chung et al8 had observed persistence of the pressor response for 1 min post intubation and then on a reducing trend thereafter to close to baseline values. Baseline heart rates were comparable among all groups, ranging from 82 ± 16 beats / min in the control group to 91 ± 17 beats / min in group F 1/3. The post induction parameters were lower than baseline values in most of the groups ranging from a 7% increase in control group to a 2.2% decrease from baseline in group F1/5, neither of which were clinically or statistically significant. Baseline SBP ranged from 123 ± 9.8 in group F 1.5/5 to 131±15 in group F1.5/3, being comparable among all groups. Post induction SBP was 1 - 8.7% lower than the baseline values. Post induction there was a lowering of DBP by 2 % in the control group and by 0.2 to 6.3 % in the groups receiving Fentanyl. MAP is reduced by 2.2 % in control group and by 1.4 to 7.8 % in the Fentanyl groups; maximum reduction is seen in group F1.5/3. This was however neither clinically nor statistically significant. Even though post induction parameters may not be attributable to fentanyl alone since it was also observed in control group ,However Iyer et al 42 had observed a 22% reduction of MAP with a 2 µg / kg and 30% reduction with doses higher than 5 µg / kg given 4 min prior to laryngoscopy. With laryngoscopy there was a rise in HR by 32 % in Control group. In group F1.5/5 there was an 9.7 % increase from baseline which was not statistically significant and with a mean of 93.7 ± 12 beats / min which was only 4 % more than induction value, the rise was only marginally significant clinically. Also, the mean HR in this group was significantly lower than the control group (p=0.001) thus demonstrating attenuation of HR. In all other groups receiving Fentanyl there was an increase from induction values, reaching mean values >100 beats / min which were clinically significant. However group F1/3 was an exception too, the rise from baseline not being statistically significant (p=0.078), even though the mean HR (101.8 ± 18 beats / min) being comparable to control group values. The significant attenuation of HR rise was more pronounced with the higher dose i.e F1.5/5 which was clearly different from all other groups. Hence it appears that attenuation of the tachycardiac response to laryngoscopy is best when small dose of Fentanyl is administered 5 min prior to laryngoscopy. The attenuation of the response was more effective in group F1.5/5 when compared to control group and to other groups. Hence, comparing the groups 1.5 µg / kg Fentanyl administered 5 min before laryngoscopy seems to be most effective. Systolic BP showed a significant rise from baseline during laryngoscopy. This was most pronounced in the Control group (21%) and in group F1.5/3 (20%). In all groups mean SBP rose to more than 150 mm Hg except group F1.5/5 where it was 130 ± 13.9 mm Hg, which was 5.8% higher than mean baseline values and this was statistically not significant. However this was significantly lower than control group value (p=0.000), thus proving that this group had better attenuation of the pressor response. With the 1 µg / kg dose given 5 min prior, the rise was by 16.8%. At either doses administered 3 min (F 1/3, F1.5/3) before laryngoscopy, rise in SBP is 9.3 % and 19.4 % from the baseline values respectively which is statistically significant. A similar pattern was seen with diastolic BP where a rise from baseline by 27.1% was seen in the control group. All groups receiving Fentanyl showed a significant rise from baseline, which was however least in group F1.5/5 i.e 11.1 %; the mean value again being significantly lower than the control group (p=0.000). This rise was around 16.6 - 26.5 % in the all other groups. Mean arterial pressure values mirrored the above changes with a 23 % increase from the baseline in the control group to a minimum 8.5 % increase in group F 1.5/5 during laryngoscopy. In the study by Ko et al4 in the group which Fentanyl 2 µg / kg 5 min before laryngoscopy, there was a 15% increase in HR and 11 % increase in MAP from baseline. The rise was higher in other groups ( 24-40 %) where the timing was 1, 3 and 10 min before laryngoscopy. This is consistent with our finding that peak clinical efficacy of Fentanyl is at around 5 min after administration. Splinter et al9 also had demonstrated that the rise in SBP in patients receiving Fentanyl 4.5 min before laryngoscopy was 20 % with 1.5 µg / kg and 8 % with 3 µg / kg compared to 40 % increase in control group. At 2 min post laryngoscopy, The HR further dropped in the Fentanyl groups to 1.9-8.7 % and 5.5-15 % below the baseline values in the next 2 min respectively. The additive effect of maintenance inhalational anaesthesia with lack of any further stimulation after cessation of laryngoscopy could have also contributed. At 3 min post laryngoscopy all hemodynamic variables in the control group had settled to values close to baseline values, while at 4 min post laryngoscopy, they were below baseline in the groups which received Fentanyl prior to laryngoscopy Hypotension defined by systolic BP lesser than 70 % of baseline was observed in 2 patients who belong to group F1.5/3, in the 4 min post laryngoscopy period.
Hypertension, defined by Systolic BP 20 % greater than the baseline value at any time during the study was seen in 40 % of Controls and 40-50 % patients receiving Fentanyl 3 min prior to laryngoscopy. There were no ECG changes suggestive of myocardial stress in any patient. Since the effect was only transient and all the patients were normal and healthy, no clinically detrimental effects were observed
CONCLUSIONS
The following conclusions can be drawn from our study comparing two different doses of Fentanyl given at three different time intervals prior to laryngosopy, to assess their efficacy in attenuating the ensuing hemodynamic stress response.
- Fentanyl 1.5 ug / kg administered 5 min before laryngoscopy provides the best attenuation (not abolition) of this response.
- Dose lower than 1.5 ug / kg when given 3 min before laryngoscopy is Inadequate for effective attenuation of the pressor response.
- Fentanyl 1.5 ug / kg administered as a bolus IV dose, does not result in any serious cardio-respiratory complications.
REFERENCES
- Wycoffc Endotracheal intubation, effects on blood pressure and pulse rate Anaesthesia 1960:21;153-57
- Lunn JK, Stanley TH, Eisele J, Webster L, Woodward A: High dose Fentanyl anaesthesia for coronary artery surgery. Plasma fentanyl concentrations and influence of Nitrous oxide on cardiovascular responses. Anesth Analg 1979; 58: 390-5
- Scott JC, Ponganis KV, Stanski DR: EEG quantitation of Narcotic effect. The comparative pharmacodynamics of Fentanyl and Alfentanil. Anesthesiology 1985; 62: 234-41
- Ko SH, Kim DC, HanYJ, Song HS: Small dose fentanyl; optimal time of administration for blunting the circulatory responses to tracheal intubation. Anesth Analg1998;86:658-61
- AL Kovac. Controlling the hemodynamic response to laryngoscopy and endotracheal intubation. J Clin Anesth. 1996;8(1):63–79.
- JD Helman, JM Leung, WH Bellows, N Pineda, et al. The risk of myocardial ischemia in patients receiving desflurane versus sufentanil anesthesia for coronary artery bypass graft surgery. . Anesthesiology. 1992;77(1):47–62.
- Kautto UM: Effect of Combinations of Topical Anaesthesia . Fentanyl , halothane or Nitrous oxide on circulatory Intubation response in Normotensive and Hypertensive patients. Acta anaesth. scand.1983; 27: 245-51
- Chung KS, Sinatra RS, Halevy JD, Paige D, Silverman DG: A comparison of fentanyl, esmolol and their combination for blunting the hemodynamic responses during rapid-sequence induction. Can J Anaesth 1992;39:774-9
- Splinter WM, Cervenko F: Haemodynamic responses to laryngoscopy and tracheal intubation in geriatric patients: effects of fentanyl, lidocaine and thiopentone. Can J Anaesth 1989; 36: 370-6.