Official Journals By StatPerson Publication
|
Table of Content - Volume 12 Issue 1 -October 2019
Sequential combined spinal epidural anesthesia (CSEA): A safe choice for elderly patients posted for major orthopedic surgery
Wasudeo S Barsagade1*, Vrishali R Ankalwar2, Yogesh R Harde3
1,2,3Department of Anaesthesiology, Government Medical College, Nagpur, Maharashtra, INDIA. Email: vriankalwar@yahoo.com
Abstract Aim and Objective: The present study was undertaken to compare the clinical effects of sequential combined spinal epidural anesthesia (CSEA) versus spinal anesthesia in elderly high risk patients undergoing major orthopedic surgery. Methods: Total 90 ASA grade II and III patients, posted for fracture hip surgeries were randomly divided in two groups of 45 in each. Group A received spinal anesthesia. Group B received sequential CSEA. Results: Both groups had minimum sensory level upto T10 with adequate muscle relaxation. Group B showed a significantly less incidence of hypotension of less severity. Also, requirement of vaso-pressor and incidence of bradycardia was less in group B(p< 0.05). Conclusion: Sequential CSEA is effective, safe and produces a comparatively stable haemodynamics with provision of prolonged analgesia compared to spinal anaesthesia in geriatric patients under-going major orthopaedic surgery. Keywords: Sequential combined spinal epidural anaesthesia, CSEA, Spinal anaesthesia, Fracture hip surgeries, Bupivacaine, Geriatric.
INTRODUCTION Spinal anaesthesia is widely used in orthopaedic surgery even for elderly patients. Because of many associated comorbidities specially enhanced atherosclerosis geriatric patients may not tolerate hypotension following spinal anaesthesia.1 Also, level of block obtained following a spinal anaesthesia is approximately 3-4 spinal segments higher in elderly compared with young adult patients.2,3Combined spinal epidural anesthesia i.e. single segment, needle though needle technique is gaining popularity in modern anaesthesia practice.1,4 CSEA offers rapid onset, efficacy and safety with potential for improving an inadequate block and prolonging duration of analgesia intraoperatively and post operatively.5This technique is now being used in elderly high risk patients for orthopaedic surgery with encouraging results and because of various claimed benefits, mainly stable hemodynamic status.6 So, we carried out this prospective, randomized, interventional study to evaluate clinical effects of sequential CSEA versusspinal anesthesia in elderly high risk patients undergoing major orthopedic surgery. . MATERIAL AND METHODS After obtaining Institutional Ethical Committee approval and patient’s written informed consent, the study was conducted in 90 adult patients of ASA grade II and III, aged between 60 to 75 years having weight and height 45-75 kg and 145-175 cm respectively, scheduled for elective fracture femur surgeries. They were randomly divided into two groups of 45 patients each, allotted to receive either spinal anesthesia or sequential combined CSEA. Patients having contraindications for central neuraxial block were excluded from the study. A thorough preanesthetic checkup and relevant investigations were done for all the patients. In the operation theatre, standard monitoring devices- NIBP, ECG, pulse oximeter and temperature probes were applied to all patients and baseline parameters like systolic blood pressure (SBP) diastolic blood pressure (DBP), mean arterial pressure (MAP), heart rate (HR), oxygen saturation (SPO2) along with respiratory rate and temperature were noted. Patients preloaded with 400 to 500 ml of Ringer Lactate solution in sitting position. Under all aseptic condition, intervertebral spaces at L3-L4 and L2-L3 were identified and prick point was infiltrated with 2 ml of 2% lignocaine. Then group A patients received spinal anesthesia with 3 to 3.5 ml of 0.5% hyperbaric bupivacaine depending upon height of the patients, like 3 ml of bupivacaine for patients with height ˂150 cm and 3.5 ml for patients with height ˃150cm. Group B received sequential CSEA with 1.5 ml (7.5 mg) of 0.5% hyperbaric bupivacaine through spinal needle of CSE set which was introduced through a 16 G tuohy’s needle in the epidural space. Spinal needle was withdrawn after injection of drug into CSF followed by insertion of 16 G epidural catheter through epidural needle in situ .After removal of epidural needle, catheter was secured and taped. Then patient gradually made supine. After 10 mins, to extend the level of block to T-10, 1.5 ml of 0.5% isobaric bupivacaine was given for every unblocked segment through epidural catheter after giving test dose with 2ml of 2% lignocaine with adrenaline. Epidural top up was repeated at 11/2 hrs – 2 hrs when sensory level receded up to T12 with 5 ml of isobaric bupivacine 0.5%. The sensory block was assessed by pin prick sensation while motor block was assessed by Bromage scale. Intraoperatively, all patients were closely monitored and hemodynamic variable SBP, DBP, HR, SPO2 were noted at regular interval. If SBP falls below 90mm of Hgor less than 30% of baseline reading, Inj.Mephentermine 7.5 mg was administered and if SBP did not improve after 2 doses of Inj.Mephenteramine, Inj. Dopamine drip (200 mg in 500 ml 5% dextrose) started. Bradycardia (HR> 56/ min) was treated with Inj. Glycopyrolate 0.1 mg in incremental doses. Any intraoperative and post-operative complications during first 48 hours were recorded. At the end of surger, for post-operative analgesia, group A received Inj.Diclofenac75 mg intramuscularly and group B received 0.125% of 6-10 ml of isobaric Bupivacaine with Bupremorphine 100 microgram through epidural catheter 8 hourly upto 48 hours. Statistical analysis Data was analyzed using statistical software STATA VERSION 10.0. Hemodynamic variables were compared at different time interval from base line by using paired t-test while mean changes in hemodynamics at different time interval between two groups were compared by Mann-Whitney test.
OBSERVATIONS AND RESULTS Table 1 showed the demographic profile of the patients in two groups. Both the groups were comparable with respect to age, sex, weight, height, ASA distribution, pre-operative hemodynamic characteristics and type of surgery. The mean duration of surgery was around 147±13.72 minutes in group A and 151.67±19.24 minutes in group B.
Table 1: Demographic data of the patients and type of surgery
In group A both sensory and motor onset time was faster as compared to group B (p.> 0.05).Minimum level of sensory block achieved in both groups was T-10.Boththe groups had adequate muscle relaxation. Three patients of spinal group required supplementation with general anesthesia due to wearing spinal block after 2hrs, (Table no.2). Table 2: Assessment of Quality of Anesthesia
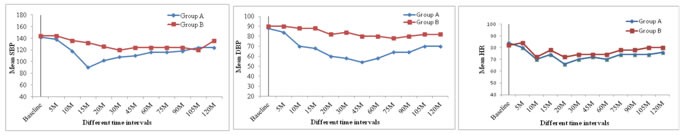
When mean values of SBP, DBP, HR at various time intervals were compared in both groups, it was observed that mean changes in SBP and DBP were more in group A as compared to group B, (P˂0.05). Also, in group A fall in SBP, DBP from its baseline values were statistically significant, (Figure 1, 2). Overall incidence of hypotension was higher in group A as compared to group B. Figure 1 Figure 2 Figure 3 Figure 1: Comparison of Systolic blood pressure (SBP) between two groups; Figure 2: Comparison of Diastolic blood pressure (DBP) between two groups; Figure 3: Comparison of Heart Rate (HR)between two groups Mean HR changes in both groups were statistically not significant (p>0.05), (Figure 3) but occurrence of bradycardia and requirement of Inj. Glycopyrolate was more frequent in group A than group B (< 0.05), (Table 3). Number complications like nausea, vomiting, headache were comparable in both groups.
Table 3: Hemodynamic changes in both groups
DISCUSSION Due to medical advances in recent years, the life expectancy of people has increased over the past century. 21% of people over the age of 60 years may undergo surgery. 85% of older patients have at least one chronic health condition and 60% may have presence of two chronic health conditions. Due to associated comorbid conditions, geriatric patients are more at risk of intraoperative and postoperative complications.7Similar to earlier studies8-10elderly patients of present study were also having comorbid conditions like hypertension, diabetes, ischemic heart disease, COPD. There exists number of studies which had observed significant arterial hypotension particularly in geriatric patients for lower limb orthopedic surgeries, who received higher doses of bupivacaine intrathecally. This inadverantly occurs in old age, as with the advanced age, the compensatory mechanisms were not as effective as in the younger age group, thus they develop hypotension even at T-6spinal level (Bhattcharya). This may occur despite use of prophylactic measures like preloading with crystalloid and or use of vassopressors. Low dose of intrathecal bupivacaine can minimize incidence and severity of hypotension but there is threat of inadequate degree and duration of spinal block which may expose these elderly patients to risk of general anesthesia who are already having compromised cardiopulmonary status. So, to overcome these problems long back in 90’s Bonnet et al11by Schnider et al12 used continuous spinal anesthesia technique but then there is risk of caudaequina syndrome. However, more improved technique, sequential CSEA where smaller doses of intrathecalbupivacine supplemented with epidural drug is observed to provide stable hemodynamics. This technique is also found to be superior to epidural block alone.13In modern obstetric practice, sequential CSEA is becoming popular because of multiple benefits, mainly stable hemodynamics.14,15 Similarly, technique of CSEA in patients of Cardiomyopathy or patients having any absolute and relative contraindication for spinal anesthesia observed to produce good sensory block and satisfactory hemodynamics and recovery score.16In our study, not only incidence but severity of hypotension was more in spinal group. Also, the requirement of vasopressors was more in spinal group than CSEA group. This is attributed to less dense spinal block in sequential CSEA. Epidural supplementation within 10 minutes of low dose of intrathecal injection of local anesthetic ensured these patients adequate level of analgesia needed for surgery. Many explanations are proposed to understand the manner by which epidural top up works after spinal anesthesia in sequential CSEA like leakage of epidural local anesthetic through the dural hole in subarachnoid space, change in epidural pressure or by enhancement of already existed subclinical analgesia at higher level.7,17No patient of sequential CSEA group required general anesthesia which again emphasizes benefits of epidural catheter.
CONCLUSION From the results of present study, we concluded that sequential CSEA technique is effective, safe, produces a stable haemodynamic with provision of prolonging surgical analgesia to any length of time depending upon the duration of surgery as compared to spinal anaesthesia in geriatric patients undergoing major orthopaedic surgery.
REFERENCES
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home