Official Journals By StatPerson Publication
|
Table of Content - Volume 12 Issue 1 -October 2019
Efficacy of paracetamol when added as an adjunct to lignocaine in intravenous regional anaesthesia- A prospective randomised double blinded study
S Sulekha1, M S Prasanth Kumar2*
1.Senior Resident, Department of Anesthesiology, ESIC Medical College and PGIMSR, K.K. Nagar, Chennai, Tamil Nadu, INDIA. Email: jabarali2009@gmail.com
Abstract Background: Intravenous regional anaesthesia (IVRA) using Lignocaine is a safe, reliable, and cost-effective technique for providing anaesthesia as well as a bloodless field during upper limb surgery. It has been postulated that the site of action in IVRA is probably by blockade of small nerves or possibly nerve endings and not the major nerve trunks. Aim: In this study we evaluated the effects of Paracetamol on the onset of sensory and motor block time, sensory and motor recovery time and the requirement of postoperative analgesia. Methods: Sixty patients undergoing upper limb extremity surgeries were randomized into two groups .IVRA was achieved by injecting 10 ml of 2% Lignocaine with 30 ml of Paracetamol to a total of 40 ml in Group 1(n=30) and 10 ml of 2% Lignocaine with 30 ml of Normal saline to a total of 40 ml in Group 2(n=30). Results: Onset of sensory and motor block was shorter and sensory recovery time was longer in Group 1 (p < 0.001). Intraoperative VAS scores were significantly lower in Group 1 (p< 0.05). Intraoperative Fentanyl consumption was 8.33 ± 21.82 mcg in Group 1 and 38 ± 37.82 mcg in Group 2, the number of patients requiring Fentanyl was 4 and 17 respectively ( p< 0.001). The postoperative analgesic requirement was lower in Group 1 with 9 patients and was 25 patients in Group 2 (p< 0.001). Conclusion: The administration of Paracetamol as an adjunct to Lignocaine in IVRA was found to be efficacious and it provided significant shortening in the onset of sensory block, a decrease in the intraoperative analgesic requirement and an improvement in the postoperative analgesia with a reduced need for analgesics in the postoperative period. Key Words: Intravenous regional anesthesia, Lignocaine, Paracetamol, Postoperative Pain
INTRODUCTION Intra Venous Regional Anaesthesia (IVRA) is a regional anaesthetic technique commonly used in forearm surgeries. It was first introduced by a German surgeon August Gustav Bier in 1908 by injecting Procaine intravenously between twotourniquets1. He found that there was a rapid onset of anaesthesia between the tourniquets and a slower onset beyond the distal tourniquet. This technique gained more importance in the late 1960s after its reintroduction by Holmes2.
AIM To determine the efficacy of Paracetamol when added as an adjuvant to Lignocaine for IVRA.
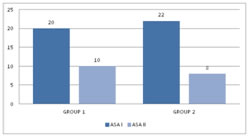
MATERIALS AND METHODS This randomized double-blinded study was conducted in the Department of Anaesthesiology, PSG Institute of Medical Sciences, Coimbatore in ASA I and II patients posted for upper limb surgeries from August 2013 – March 2015.The study group patients were assigned into two groups as Group 1 and Group2, comprising of 30 patients each. IVRA was performed using 10 ml of 2%Lignocaine with 30 ml of Paracetamol in Group 1 patients and 10 ml of 2%Lignocaine with 30 ml of Normal saline in Group 2. Inclusion Criteria: ASA I and II patients, aged between 20-60 yrs, Upper limb extremity surgeries of duration not exceeding 60 minutes. Exclusion Criteria: a history of allergy to local anaesthetics, expected duration of surgery more than 60 minutes, Raynaud’s disease, Sickle cell anaemia, Coagulation disorders. Simple randomization was done and assigned into two groups (with 30 patients in each group as Group -1 and Group - 2). According to ASA starvation guidelines patients were kept nil per oral status overnight and pre-medicated with Tablet Ranitidine 150 mg and Tablet Diazepam 5 mg the night prior to surgery and on the morning of surgery. Anaesthesia machine safety checklist including resuscitation equipment, emergency drugs and tourniquet equipment were kept ready before the patient arrived in the operating room (OR). Starvation status and surgical consent confirmed in the preoperative room before the patient was shifted inside the operating room. Preinduction monitors like ECG leads, Noninvasive blood pressure (NIBP)cuff and pulseoximeter were connected and baseline readings noted. All the patients were explained about the Visual Analogue Scale (VAS) prior to the start of the procedure. Vital signs like MAP, HR, and SpO2 were recorded before and after application of a tourniquet and monitored continuously during the procedure at 5, 10, 15, 20, 30,40, 50 minutes interval till the release of a tourniquet. The pain was assessed using a 10cm visual analogue scale. If the patient reported a VAS > 4, rescue analgesic of 1 mcg/kg Fentanyl was intravenously given and the requirement for analgesics was recorded.
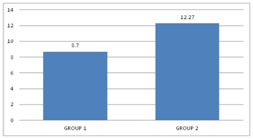
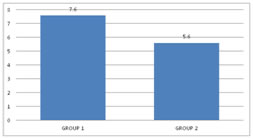
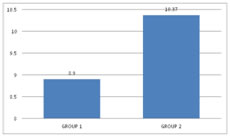
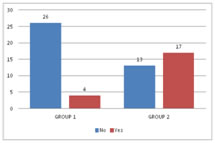
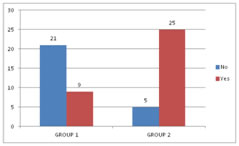
RESULTS In this study, 60 patients were selected after considering the inclusion and exclusion criteria. Consent was obtained from all the 60 patients and was divided into2 groups with 30 patients in each group. Group 1 received 30 ml of Paracetamol and 10 ml of 2% Lignocaine (preservative-free (PF)). Group 2 received 30 ml of Normal Saline and 10 ml of 2% Lignocaine (preservative-free (PF)). In our study, after reviewing the literature we selected the study group in the age between 20 – 60 years. The mean age distribution in our study was 42.87±11.57 in Group 1 and 39.37±13.04 in Group 2. Out of 60 patients in our study, the sex distribution was 18:12 (Male: Female)in Group 1 and 16:14 (Male: Female) in Group 2.In our study, we used a double pneumatic tourniquet placing the first tourniquet on the proximal portion of the extremity to be operated and the second tourniquet distal to the proximal one. Group 1 patients in our study had very negligible intraoperative pain / discomfort during the procedure, but Group 2 patients reported with pain intraoperatively, presumably tourniquet pain. In our study, the meantime of onset of sensory block was 5.60± 1.58 minutes in Group 1 and 7.13± 1.59 minutes in Group 2 patients. The p-value<0.001 shows there is a statistically highly significant difference between the two groups in terms of the time of onset of sensory block. In our study amongst patients in Group 1, the average onset of motor block time was 8.70± 2.52 minutes and in Group 2 it was 12.27± 2.79 minutes. The p-value<0.001 shows that there is a statistically significant difference among the two groups in terms of the time of onset of motor block. In our study, the sensory recovery time was 7.60± 1.102 minutes in Group 1and 5.60± 1.610 minutes in Group 2. The p-value<0.001 showed that there is a statistically highly significant difference with regard to the onset of the sensory recovery time between the two groups. In our study, the motor recovery time was 8.90± 2.13 minutes in Group 1 and10.37 ± 2.498 minutes in Group 2. The p-value 0.018 showed that there is a statistically significant difference between the two groups in terms of motor recovery time. In our study, 4 patients out of 30 required Fentanyl consumption intraoperatively in Group 1 and 17 patients out of 30 in Group 2 and proved to be statistically significant. In our study, the mean Fentanyl consumed was 8.33±21.82 micrograms in Group 1 and 38±37.820 micrograms in Group 2, p-value<0.001 showed that there is a statistically significant difference between the two groups in terms of Fentanyl consumption as rescue analgesic intraoperatively. The mean VAS pain score intraoperatively was 2.17±1.62 in Group 1 and3.80±2.36 in Group 2. The p-value 0.003 showed that there is a statistically significant difference in the intraoperative VAS score between the two groups. Out of 30 patients in each group in our study, 9 patients required analgesia following tourniquet deflation in Group 1 and 5 patients in Group 2; which was statistically significant between the two groups with p-value< 0.05.Out of 30 patients in each group in our study, surgeon satisfaction grade was excellent in 14 patients in Group 1 and 6 patients in Group 2. The grade was good in16 patients of Group 1 and 24 patients of Group 2. There was a statistically significant difference between the two groups as the p-value is 0.028 (which is < 0.05) with regard to surgeon satisfaction in our study. Out of 60 patients in our study, 7 patients from Group 1 and 2 patients from Group 2 gave excellent grading (Grade 1), 18 patients from Group 1 and 14 patients from Group 2 gave good grading (Grade 2) and 5 patients from Group 1 and 14patients from Group 2 gave moderate grade (Grade 3).There was a statistically significant difference between the two groups as p is0.023 (<0.05) with regard to patient satisfaction in our study.
Figure 1 Figure 2 Figure 3 Figure 4
Figure 5 Figure 6 Figure 7
Figure 1: ASA grading distribution Figure 2: Onset of the sensory block (mins) Figure 3: Onset of the Motor block (mins) Figure 4:Sensory recovery time Figure 5: Motor recovery time; Figure 6: Fentanyl Consumption; Figure 7: Postoperative analgesic requirement
Figure 1: ASA grading distribution Figure 2: Onset of the sensory block (mins) Figure 3: Onset of the Motor block (mins) Figure 4:Sensory recovery time Figure 5: Motor recovery time; Figure 6: Fentanyl Consumption; Figure 7: Postoperative analgesic requirement
DISCUSSION In our study, we investigated whether the addition of Paracetamol to IVRA solution decreased tourniquet pain, intraoperative use (Fentanyl) and enhanced the sensory and motor block duration by increasing the quality of IVRA. However, in our study we also demonstrated a decrease in postoperative pain score and analgesic requirement. Elhakim M and Sadek RA12 carried out IVRA on patients between 25 – 55years. Palecha S et al13 used IVRA on patients above 20 years of age. Sanjay Kherde et al14 used the age group of 15 – 55 years in his study. Tourniquets are used in IVRA to restrict the drugs from entering beyond the cuff into the systemic circulation causing untoward consequences. It is also used to provide analgesia and motor blockade distal to the tourniquet. Chandrashekara PM et al15 used single rubber latex bandage as a tourniquet above the site of surgery. He noted the tourniquet pain and discomfort in surgeries that prolonged for more than 40-50 minutes. Holmes C et al1, Sorbie C and Chancha P16 and Janardhan et al17 used double tourniquet with the second tourniquet placed on the anaesthetized portion of the extremity distal to the proximal one to prevent tourniquet pain and discomfort. Intravenous regional anaesthesia technique is successful when there are proper tourniquet placement and adequate exsanguination1.Holmes C et al1 and Chandrashekara PM et al15 achieved exsanguination either by simple gravity draining method or by using Esmarch bandage and combined both in some cases. Blond L et al18 showed there was a 69% reduction in blood volume in the limb after exsanguinations using Esmarch bandage. The observation of the present study is in accordance with regards to the meantime of onset of the sensory block by Myoung Jin Ko and Jeong Han Lee et al19. He reported a similar statistically significant difference in his IVRA study, in patients who received 40 ml of 0.5% Lignocaine in one group and 0.5% Lignocaine diluted with intravenous Acetaminophen 300 mg to a total volume of 40ml. The observation of the present study is in accordance with the observations of Sen H, Kulahci Y et al20 who stated the similar statistically significant difference in theirs tudy population with the meantime motor block onset, mean time of sensory block recovery time, mean time of motor block recovery time. This observation was in accordance with observation obtained in Sen H et al20where intraoperative VAS scores were seen at 20 and 30 minutes were significantly lower in Group 2 which was 10 ml 3mg/kg Lignocaine with 300mg Paracetamol similar to the present study. Post deflation analgesic requirement in a study done by Sen H et al20 and Myoung Jin Ko et al19 where they showed a statistically significant difference between the two groups with a p
CONCLUSION To conclude from our study, that the administration of Paracetamol as an adjunct to Lignocaine in IVRA, was found to be efficacious and it provided significant shortening in the onset of sensory block, a decrease in the intraoperative analgesic requirement and an improvement in the postoperative analgesia with a reduced needf or analgesics in the postoperative period. REFERENCES
|
|
 Home
Home