Official Journals By StatPerson Publication
|
Table of Content - Volume 12 Issue 2 -November 2019
A comparative study of different doses of ephedrine on intubating conditions and haemodynamics using propofol and low dose rocuronium
Manju Sharma1*, Anju Jamwal2, Anjali Mehta3, Ruchika Jyoti4
1,2,3,4Department of Anaesthesiology, Government Medical College, Jammu, J & K, INDIA. Email: sharmamanju30june@gmail.com
Abstract Background: Succinylcholine as muscle relaxant is a norm in emergency department even though it is associated with a multitude of adverse effects. We used low dose rocuronium with ephedrine so as to shorten the onset of rocuronium in accordance with rapid sequence intubation without prolonging the duration as seen with the usual dose for rapid sequence intubation. Increase in cardiac output caused by Ephedrine can reduce the onset time of Rocuronium. Hypotension associated with bolus dose of Propofol during induction can also hypothetically be prevented by the use of Ephedrine. Appropriate dose of Ephedrine is advised to achieve the aforementioned benefits without undue side effects such as hypertension and tachycardia. Because of variation in doses and side effects of Ephedrine in various studies, we compared the influence of Ephedrine 30, 70 and 110 mcg/kg on intubating conditions and haemodynamics using Propofol and low dose Rocuronium Method: 90 patients of either sex, ranging in age from 18-50 years belonging to ASA grade 1 and 2 undergoing elective surgeries under general anaesthesia were taken up for study. Patients were randomly allocated to one of the three groups of 30 patients each.Group1- Patient received Rocuronium 0.6 mg/kg and Ephedrine 30mcg/kg Group2- Patient received Rocuronium 0.6 mg/kg and Ephedrine 70mcg/kg Group3- Patient received Rocuronium 0.6 mg/kg and Ephedrine 110mcg/kg Result: It was found that intubating conditions were most favourable in group 2(Ephedrine 70 mcg/kg) followed by group 3(Ephedrine 110 mcg/kg) and least favourable in group 1(Ephedrine 30 mcg/kg). Group 3 was associated with adverse haemodynamic effects such as tachycardia and increased blood pressure. Such effects being least in group 1(Ephedrine 30 mcg/kg) and intermediate in group 2(Ephedrine 70 mcg/kg). Conclusion: Ephedrine pre-treatment in the dose of 70mcg/kg with similar doses of Rocuronium and Propofol provides ideal intubating conditions with acceptable haemodynamic changes. So, the combination of Propofol 2.5mg/kg, Rocuronium 0.6mg/kg and ephedrine 70mcg/kg may be of value when use of Succinylcholine is contraindicated for Rapid Sequence Induction. Key Points: ephedrine, haemodynamics.
INTRODUCTION Rapid sequence intubation is almost a norm in emergency departments where full stomach patients are commonly encountered. Succinylcholine is the most common neuromuscular blocking agent used owing to its short onset as well as duration. Though succinylcholine is the most favoured neuromuscular blocking agent for rapid sequence intubation, its use is not without several adverse reactions ranging from myalgia to hyperkalemia, masseter spasm and even death. To avoid these adverse reactions, non-depolarising muscle relaxants have come in favour. Rocuronium in appropriate doses has a speed of onset only marginally slower than that of Succinylcholine. It has an intermediate duration of action and depends on the kidney and liver for elimination. Rocuronium by the virtue of its low potency and thereby a rapid onset of action may be used in place of Succinylcholine. However, the onset of Rocuronium is dose dependent and duration of action is longer as compared to Succinylcholine which limits it’s use in Rapid Sequence Induction. Most of the general anaesthetic procedures require laryngoscopy and endotracheal intubation. Risk of hypoxia and pulmonary aspiration is highest in the period ranging from loss of consciousness to tracheal intubation. Therefore, it becomes important to use a neuromuscular blocking agent with short onset so as to prevent life threatening hypoxia or aspiration. The onset time of Rocuronium depends on the rate at which a pharmacologically effective concentration is achieved in the Biophase, that is the neuromuscular cleft. In turn, this rate is influenced by certain factors, such as the potency of the drug, the dose administered and the cardiovascular status namely cardiac output and muscle blood flow. Moreover, the onset time of drugs with rapid onset such as Rocuronium, chiefly depends on the circulation time to the muscle.1 It has been reported that Rocuronium is only comparable to Succinylcholine during Rapid Sequence Induction and Intubation in a dose of 0.9-1.2 mg/kg body weight, but a dose of 0.9-1.2 mg/kg lead to increased duration of action up to 50-60 minutes.2 Rocuronium in a dose of 0.6 mg/ kg produced moving vocal cords on direct laryngoscopy and diaphragmatic response to intubation in 20-25% of patients.3 Ephedrine is an indirect acting sympathomimetic agent that stimulates both alpha and beta receptors, and hence increases systolic blood pressure, diastolic blood pressure, heart rate, cardiac output and venous return. Intravenous Ephedrine is used for hypotension associated with regional anaesthesia in a dosage of 2.5-10 mg I/v stat. Ephedrine by increasing the cardiac output and tissue perfusion could reduce the onset time of Rocuronium and improve the intubating conditions.4 It can also prevent hypotension associated with bolus doses of Propofol during induction of general anaesthesia.5 The peak effect of Ephedrine on cardiac output is reached at about 2-3 minutes after the injection.6 It is advisable to use an appropriate dose of Ephedrine to achieve both these benefits without undue side effects such as hypertension or tachycardia. Because of variation in doses and side effects of Ephedrine in various studies, we compared the influence of Ephedrine 30, 70 and 110 mcg/kg on intubating conditions and haemodynamics using Propofol and low dose Rocuronium.
AIMS AND OBJECTIVES
MATERIAL AND METHODS The present randomised open labelled prospective study was conducted in the Post Graduate department of Anaesthesiology and critical care GMC, Jammu. This study was approved by the University's Institutional Ethics Committee (IEC/Thesis/Research/T5B/2016/294) dated 07-10-2016 and written informed consent was obtained from all subjects participating in the trial. 90 patients of either sex, ranging in age from 18-50 years belonging to ASA grade 1 and 2 undergoing elective surgeries under general anaesthesia were taken up for study. Patients were randomly allocated to one of the three groups of 30 patients each. Group1- Patient received Rocuronium 0.6 mg/kg and Ephedrine 30mcg/kg Group2- Patient received Rocuronium 0.6 mg/kg and Ephedrine 70mcg/kg Group3- Patient received Rocuronium 0.6 mg/kg and Ephedrine 110mcg/kg Exclusion Criteria • Patient refusal to participate in the study. • Hypersensitivity to study drugs. • Haemodynamically unstable patient. • Any cardiovascular or neuromuscular disease. • Intake of drugs known to interact with neuromuscular junction or Ephedrine such as Aminoglycosides, Tetracyclins, Bacitracin, Polymyxin B, Colistin, Sodium Colistimethate, MAO inhibitors and Tri Cyclic antidepressants. • Anticipated difficult airway (MPG grade 3 or 4). • Cormack Lehane grade 3 or 4 on direct laryngoscopy. • Patients on chronic preoperative Beta-Adrenergic Blocker treatment. • Pregnancy • Obesity(BMI>30Kg/m2) • History of long term Diuretic or vasoactive medication. • 30% or more increase in BP or HR above baseline during procedure were excluded from the study. Statistical Methods: The recorded data was compiled and entered in a spreadsheet (Microsoft Excel) and then exported to data editor of SPSS Version 20.0 (SPSS Inc., Chicago, Illinois, USA). Continuous variables were summarised in the form of means and standard deviations and categorical variables were expressed as frequencies and percentages. Graphically the data was presented by bar and lie diagrams. Analysis of variance (ANOVA) with least significant difference (LSD) test was employed for comparing continuous variables. Chi-square test or Fisher’s exact test, whichever appropriate, was applied for comparing categorical variables. A P-value of less than 0.05 was considered statistically significant.
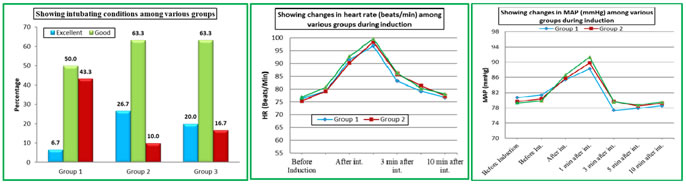
RESULTS The demographic parameters of the patients including age, weight, sex, ASA status and intubating time was statistically insignificant between the groups(p-value>0.05) (Table 1 and 2). Among the 90 patients enrolled in the study 4 patients were excluded from the study. Endotracheal intubation caused significant increase in systolic and diastolic blood pressure (systolic/diastolic blood pressure: >200/100) at 1 minute in 4 patients of group 3 (110mcg/kg) with no patients in other study group. This exaggerated response may be because lighter planes of anaesthesia, prolonged laryngoscopy or higher dose of Ephedrine (110mcg/kg). It was found that intubating conditions were most favourable in group 2(Ephedrine 70 mcg/kg) followed by group 3(Ephedrine 110 mcg/kg) and least favourable in group 1(Ephedrine 30 mcg/kg) (Table 3, Fig 1)). Group 3 was associated with adverse haemodynamic effects such as tachycardia and increased blood pressure. Such effects being least in group 1(Ephedrine 30 mcg/kg) and intermediate in group 2(Ephedrine 70 mcg/kg). However, group 2(Ephedrine 30 mcg/kg) had best patient profile in terms of favourable intubating conditions and haemodynamic conditions (Fig 2 and 3). Table 1: Showing mean age of study patients among various groups
Table 2: Comparison based on intubating time among various groups
Table 3: Comparison based on intubating conditions among various groups
*Statistically Significant Difference from Baseline (P-value<0.05)
Figure 1 Figure 2 Figure 3 Figure 1: Intubating conditions amongst various groups; Figure 2: Changes in heart rate (beats/ min) among various groups during induction; Figure 3: Changes in MAP (mm Hg) among various groups during inductionDISCUSSION In patients where Succinylcholine could be avoided because of conditions like recent burns, open globe injury, increased intracranial pressure etc., Rocuronium was successfully used in higher doses of 0.9-1.2 mg/kg to decrease the onset time of neuromuscular blockade. When a large dose of Rocuronium is used, its duration of action is prolonged, making it unsuitable for short procedures and difficult ventilation situations. Several anaesthesiologists used Rocuronium in the lower dose of 0.6 mg/kg for rapid tracheal intubation which lead to suboptimal intubating conditions in 20–25% of patients.8 Ephedrine as an adjuvant with Rocuronium and Propofol has various effects. A larger dose of Rocuronium 0.9±1.2 mg/kg can be avoided by administering ephedrine. Another advantage being that it’s theoretically safer for haemodynamically unstable patients. Induction with Propofol, Ephedrine and low dose Rocuronium produces good intubating conditions in a timescale appropriate for rapid sequence induction. The use of the Propofol-Ephedrine combination will also avoid the unwanted side-effects of Ketamine and Etomidate, which although shortens the onset of Rocuronium but produces hallucinations and adrenal suppression.9 The better intubating conditions in Group 2 and Group 3 are most likely due to the effects of Ephedrine resulting in an increased cardiac output and tissue perfusion and therefore a faster delivery of Rocuronium to the laryngeal and diaphragmatic muscles. The factors affecting the onset of neuromuscular blockers have been extensively reviewed by Donati, 19881 and includes access of the neuromuscular blocker to the muscle and its interaction with muscle nicotinic receptors. The speed of a drug's access to these receptors appears to be proportional to cardiac output, circulation time and muscle perfusion. Development of neuromuscular blockade was not monitored as there is a poor correlation between onset time of neuromuscular blockade measured at the adductor pollicis muscle and the quality of intubating conditions 10. Agoston, 199511 has declared that neuromuscular transmission monitoring is probably obsolete in this context. Furthermore, we considered it more important to adhere to a rapid sequence protocol rather than delay tracheal intubation during the calibration period of a neuromuscular transmission monitor. In present study, the difference in heart rate from the baseline was greatest in group 3 followed by group 2 and group 1 in that order. This can be explained by the fact that in group 1 we used lowest dose of Ephedrine and hence patients’ laryngeal and diaphragmatic musculature could not be completely paralysed during laryngoscopy and intubation. As lower dose of Ephedrine has minimal effect on cardiac output, therefore decreased amount of the muscle relaxant will be present in the biophase leading to poor relaxation of laryngeal musculature during intubation and hence the aforementioned effects. No statistically significant difference in Systolic blood pressure, diastolic blood pressure and mean arterial pressure was found amongst the groups on intergroup comparison (P value>0.05). On intragroup comparison, statistically significant increase in systolic blood pressure, diastolic blood pressure and mean arterial pressure from baseline was seen after intubation and 1 minute after intubation in all the three groups. The difference in blood pressure from the baseline was greatest in group 3 followed by group 2 and group 1 in that order. The increase in heart rate and blood pressure after Ephedrine is expected as it is a sympathomimetic drug which stimulates both alpha and beta receptors, and also releases Noradrenaline from the storage sites. This sympathomimetic action is responsible for the haemodynamic changes. However, the heart rate returned to baseline at 5 minutes after intubation and the systolic blood pressure, diastolic blood pressure and mean arterial pressure returned to baseline at 3 minutes after intubation. Finally, to sum up, ephedrine 70 mcg/kg given 60 seconds before Rocuronium improved intubating conditions and facilitated the onset of Rocuronium without adverse hemodynamic effects. It was found that intubating conditions were most favourable in group 2(Ephedrine 70 mcg/kg) followed by group 3(Ephedrine 110 mcg/kg) and least favourable in group 1(Ephedrine 30 mcg/kg). Group 3 was associated with adverse haemodynamic effects such as tachycardia and increased blood pressure. Such effects being least in group 1(Ephedrine 30 mcg/kg) and intermediate in group 2(Ephedrine 70 mcg/kg). However, group 2(Ephedrine 30 mcg/kg) had best patient profile in terms of favourable intubating conditions and haemodynamic conditions.
CONCLUSION We conclude that pre- treatment with ephedrine 30mcg/kg one minute before administration of low dose Rocuronium (0.6mg/kg) on induction with Propofol (2.5mg/kg) provides poor intubating conditions with stable haemodynamics, while pre- treatment with ephedrine 110mcg/kg with the same doses of Rocuronium and Propofol provides acceptable intubating conditions but with exaggerated and unacceptable haemodynamic response. Ephedrine pre-treatment in the dose of 70mcg/kg with similar doses of Rocuronium and Propofol provides ideal intubating conditions with acceptable haemodynamic changes. So, the combination of Propofol 2.5mg/kg, Rocuronium 0.6mg/kg and ephedrine 70mcg/kg may be of value when use of Succinylcholine is contraindicated for Rapid Sequence Induction. REFERENCES
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home