Official Journals By StatPerson Publication
|
Table of Content - Volume 12 Issue 2 -November 2019
Ultrasound guided three in one block: A comparative study with spinal anaesthesia in lower limb surgeries
Ravi Kumar1, Moona Abdul Kadiru2*
1Professor, 2Assistant Professor, Department of Anaesthesia, MMCH, Modakkallur, Calicut, Kerala, INDIA. Email: moonakad@gmail.com
Abstract Background: Ultrasound guided 3in1 block is safe and easy procedure. It provides rapid and effective anaesthesia. Although several studies have been conducted most of them were focussed on analgesia purpose there are limited number of studies on the efficacy US guided 3 in 1 block used for conducting a surgery. The current study is aimed on whether ultrasound guided three in one block can be an alternative to spinal anaesthesia in lower limb surgeries. Methodology: Sixty patients posted for elective lower limb surgeries were taken divided into two equal groups based on randomised double blind fashion. In group I US guided 3in1 block was given and in group II spinal anaesthesia was given. Onset of action, duration of action, hemodynamic variability, side effects, quality of block, early ambulation were compared in both the groups. Sensory involvement of individual nerves and motor involvement of flexor, adductor and extensors of thigh are evaluated. Results: Demographic data and surgical characteristics were similar in almost both the group. The onset for spinal group, mean onset is 1.8 min. For 3in1 block group mean onset is 13.0 min(p value < 0.01). Mean duration of analgesia in spinal anaesthesia is 2.1 hours and in three in one block is 7.9 hours( p value < 0.01). Regarding heamodynamic variability (bradycardia, hypotension), in spinal anaestheisa 86.7% did not develop bradycardia and in 3in1 block no one developed bradycardia. In spinal anaesthesia group everyone had hypotension in 3in1 group no one had hypotension. No side effects in both the groups. The quality of block in 3 in 1 block is adequate in (51.7%) and inadequate or failed in (48.3%). In spinal anaesthesia it is (96.7%) and (3.3%) respectively.(p value <0.001). Early ambulation was another feature assessed it was possible in 43.3% of patients in spinal anaesthesia and 100% in 3in1 block.(p<0.01). Sensory block involvement was assessed femoral nerve (100%), obturator (65.4%), lateral cutaneous nerve (96%) p value is <0.01. Hence it is statistically significant. Motor involvement in 3in1 block group were assessed in flexor compartment(100%) involvement , adductors(64.0%) and extensor group (96%)..(p<0.001), which were found to be statistically significant. Conclusion: To conclude US guided 3in1 block is safe and easy procedure. It requires minimal US training it provides rapid and effective anaesthesia. Duration of analgesia is prolonged. As US guidance is used chances of failure and obturator nerve sparing are less compared to the conventional technique. Early ambulation is possible with 3in1 block and hemodynamic variability is minimal in 3in1 block and hence can be safely administered in cardiovascular compromised patients. Hence it may be used as alternative to subarachnoid block in lower limb surgeries. Key Words: US guided 3in 1block, spinal anaesthesia, anterior thigh and patella
INTRODUCTION In the current era most of the anterior thigh surgeries are performed either under subarachnoid block or sciatic femoral block but in either of these procedures they have their own fallacies, like subarachnoid block cannot be given with safety in cardiovascular compromised patients, while in sciatico femoral block a large volume of drug has to be administered. Ultrasound guided three in one block involves visual identification of the femoral nerve sheath and subsequent infiltration of anaesthetic. The block involves Femoral nerve, Obturator nerve, and the Lateral cutaneous nerve. The literature has found this nerve block to be simple, safe, and time efficient maneuver providing rapid and effective anaesthesia.1-6, The current study was designed to investigate whether three in block under ultrasound guidance for anterior thigh and patella surgeries will be an alternative to the conventional technique the Subarachanoid block.
MATERIALS AND METHODS Present study was a double blinded randomised prospective clinical study, 60 American Society of anaesthesiologists (ASA) physical status class I and II patients scheduled to undergo lower limb surgeries were randomly recruited for the study and divided into 2 equal groups of 30 patient each by block envelope randomization method. Calculation of sample size
[(Za + Zþ)2xo2x2] N =d2 Zα = 1.96 Z=0.84 σ = pooled variance d = difference in mean From the parent study conducted by Marhofer p et al, σ2 = 1.7 and d = 2.3. On applying these values to the sample size equation, a sample size of 5 was required in each group, but to improve the statistical value, a sample size of 30 was allocated in each group.
Inclusion Criteria
Undergoing elective surgeries for lower limb orthopaedic and soft tissue lesions and Split skin grafting Exclusion CriteriaPatients of ASA grade III and IV Age <18 years and >60 years Falling into risk classification beyond American society of anaesthesiology grade 3 History of allergy to amide local anaesthetics Patients on anticoagulants Haematological or bleeding disorder Known peripheral or central nervous system disorder Known malformation of vasculature of lower limb Distorted anatomy of pelvis and lower limb Those with difficulties in communication Cardiac arrhythmia Heart blocks Local infection Patient refusal Pre Operative Evaluation and Preparation
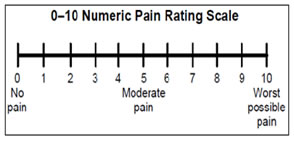
Anaesthetic Technique This study was conducted in 60 patients scheduled for elective lower limb surgeries involving the anterior thigh and patella. The procedure was explained to the patients in advance and attained a good rapport. As the patient arrived in the operation room, BP was recorded using non invasive blood pressure (NIBP) cuff and three lead ECG monitor is attached for continuous monitoring. Pulse oximeter probe was placed. Group A was given subarachnoid block under aseptic precaution with 25 gauge Quinkae needle 2 ml 0.5% bupivacaine heavy(8mg)is injected at lumbar 3-4 space using midline approach Group B was ultrasound guided three in one block under aseptic precaution under ultrasound guidance using a linear array probe 6-18 MHZ with sonosite ultrasound portable system using a 20 gauge IV canula 0.5% bupivacaine 30 ml given over the femoral nerve under the fascia iliaca 2cm lateral to the femoral artery. The anaesthetics spread in a cephalad direction and appears as expanding hypo echoic area within the fascial space surrounding the nerve sheath .Distal pressure is applied during and shortly after injection. Onset and duration of both the block were assessed. Onset of sensory blockade of each nerve was assessed with pin prick test and motor blockade of each group of muscle (flexor, extensor, adductor) assessed in group B were assessed with The Medical Research Council Scale for grading muscle function. Quality of block was assessed on basis requirements of supplementation of analgesia and sedation (ketamine in a dose of 2mg/kg given or fentanyl in a dose of 2mcg/kg given) or whether the patient had to be given general anesthesia. Fluid maintenance was done with Normal Saline and Ringer Lactate. Blood pressure, heart rate and respiratory rates were noted every 15 minutes in the intra operative period. Adverse events noted comprised of hypotension (a 20% decrease in relation to the base line value), bradycardia (HR <50 beats per min).Early ambulation of the patient was noted in both the group. Total analgesia time was noted from the point of absence of pin prick sensation to the first appearance of pain in the post operative period. The exact appearance of pain and discomfort was noted. Post operatively patients were given Inj. Diclofenac 2-3 mg/kg when the NRS score is >4. According to NRS score
Hemodynamic variability like hypotension, bradycardia, was closely watched in both groups. Side effects like Tachycardia, Hypertension, arrhythmia, accidental vascular puncture in three in one block group and urinary retention. Descriptive statistics such as percentage, mean, standard deviation and median were used to describe the variables used in study. Inferential statistics such as independent t test and chi square test were used to compare the outcomes and side effects between spinal and three in one block. SPSS 17.0 version was used to analyze data.
RESULTS 60 patients were studied. Ultrasound guided three in one block with0.5% bupivacaine 2.5 mg/kg given in group I and spinal anesthesia 0.5% bupivacaine (heavy) 8mg given in group II. The results were analyzed as follows.
Table 1: Comparison of onset of block
**: - Significant at 0.01 level
Mean onset of analgesia in Spinal anaesthesia is 1.8 minutes and in 3 in 1 block 13 minutes. P value is statistically insignificant Table 2: Comparison of duration of block
**: - Significant at 0.01 level Mean duration of analgesia in spinal anaesthesia is 2.1 hours and in three in one block is 7.9hours and p value is <0.01 which is statistically significant
Table 3: Comparison of Quality of Block
χ2 =15.709 df=1 p<0.001 The quality of block in 3 in 1 block is adequate in (51.7%) and inadequate or failed in (48.3%).in spinal anaesthesia it is (96.7%) and (3.3%) respectively
Table 4: Comparison of bradycardia based on group
In spinal anaestheisa 86.7% did not develop bradycardia and in 3in1 block no one developed bradycardia
Table 5: Comparison of hypotension based on group
**: - Significant at 0.01 level In spinal anaesthesia group everyone had hypotension in 3in1 group no one had hypotension. Table 6: Comparison of early ambulation in both groups
**: - Significant at 0.01 level Early ambulation was possible in 43.3% of patients in spinal anaesthesia and 100% in 3in1 block.(p<0.001) statistically significant Table 7: sensory involvement based on nerves
**: - Significant at 0.01 level Sensory block involvement was assessed femoral nerve (100%), obturator(65.4%) , lateral cutaneous nerve(96%) p value is <0.01hence it is statistically significant.
Table 8: motor involvement based on group of muscles
**: - Significant at 0.01 level Motor onset of analgesia in spinal anaesthesia is 1.8 minutes and in 3 in 1 block it is 13 minutes. P value is statistically insignificant
DISCUSSION One of the most common peripheral nerve blocks to facilitate postoperative analgesia is the3-in-1 nerve block, which uses a single injection to block the Femoral, Lateral femoral cutaneous (LFC), and Obturator nerves. These 3 nerves provide the major sensation to the lower extremity, and the ability to inhibit the individual distributions allows for successful analgesia and anaesthesia during, and following, knee and anterior thigh surgery. Anaesthesia practitioners have used the 3-in-1 block for many years to provide anaesthesia and analgesia to patients undergoing lower- extremity surgical procedures. However, the 3-in-1 block can be difficult to place and can result in anaesthesia sparing to the Obturator nerve, thereby leading to increased dissatisfaction among anesthesia providers and patients.7 It has also been noted that the 3-in1 block is often performed using the assistance of peripheral nerve stimulation and/or ultrasound guidance for placement, thereby necessitating the development of special skills and experience to consistently provide effective peripheral nerve analgesia. The potential for side effects is also a consideration when using a 3-in-1 block because of the proximity of the block to the femoral vasculature and increased risk of systemic absorption and toxicity.7,8 The present study is a prospective and double blinded randomized manner. Thirty patients each of either sex as per ASA physical status Grade I and Grade II,between 18-60 years of age , scheduled to undergo lower limb surgery, allocated to two groups randomly, were included in the study. In the present study an attempt has been made to evaluate the efficacy of 3in1 block can it be an alternative for the conventional subarachnoid block in lower limb surgeries, to enhance the precision of block ultrasound guidance was also used. The analysis was based on demographic parameters like age distribution, sex, weight, onset and duration of analgesia, the quality of block, hemodynamic variability, side effects. Among 60 patients studied. In spinal group 15 (50%) were males and 15 (50%) were females. In 3in1 block group 16(53.3%) were males and 14(46.7%) were females .Mean age of patient in 3in1 block group is 36.2 ± 10.8 and mean age of patient in spinal group is 35.6 ± 11.0 . Mean weight of patient in 3in1block group is 64 ± 7.2 kg and in spinal group is 62.9 ±5.4 ( p value = 0.905).So in this study all the demographic parameters (age , sex and weight ) are found comparable in both 3in1 block group and spinal anesthesia group (p value > 0.05). In this study it was observed that, for spinal group, mean onset is 1.8 min, For 3in1 block group mean onset is 13.0 min(p value < 0.01). The difference in onset of analgesia is statistically significant. Mean duration of analgesia in spinal anaesthesia is 2.1 hours and in three in one block is 7.9 hours( p value < 0.01). The difference in duration of analgesia is also statistically significant. Oberndorfer et al. found the duration of analgesia was longer and the volume of local anesthetic was significantly reduced with US compared with nerve stimulator (NS) guidance9. The quality of block in 3 in 1 block is adequate in (51.7%) and inadequate or failed in (48.3%).in spinal anaesthesia it is (96.7%) and (3.3%) respectively.(p value<0.001).hence the quality of block is statistically significant. In a study conducted by L T jerrol B Wallace et al There were no failures of the 3-in-1 block in this study, which may be due to the application of the ultrasound guided technique, which allows visualization of the femoral nerve and artery. In addition, infiltration of the local anesthetic into the femoral sheath further increases success of localizing the Obturator and LFC nerves. This is important because previous studies have suggested that the failure rate of the 3-in-1 block is directly related to the inability to consistently block all 3 nerves, thereby increasing postoperative analgesia requirements.10 To alleviate this potential problem, the addition of ultrasound is recommended when using the 3-in-1 block technique. This method decreases the level of difficulty, which allows the inexperienced provider or trainee to be successful in block placement. To obtain this success level, the anesthesia provider or trainee must be familiar with the anatomical landmarks seen under ultrasound. The lack of experience with ultrasound guidance may have contributed to the lower success rate noted in previous studies. The hemodynamic variability were assessed (bradycardia, hypotension). In spinal anaestheisa 86.7% did not develop bradycardia and in 3in1 block no one developed bradycardia. In spinal anaesthesia group everyone had hypotension in 3in1 group no one had hypotension Early ambulation was another feature assessed it was possible in 43.3% of patients in spinal anaesthesia and 100% in 3in1 block.(p<0.01)statistically significant. Sensory block involvement was assessed femoral nerve (100%), Obturator(65.4%), lateral cutaneous nerve(96%) p value is <0.01 hence it is statistically significant. Motor involvement in 3 in1 block group were assessed in flexor compartment (100%) involvement, adductors(64.0%) and extensor group(96%)..(p<0.001)statistically significant which signifies that chances of Obturator sparing is less when ultrasound guidance is used for giving the block. There were no side effects in both group in 3in 1 block there were no accidental arterial punctures neither any signs of increased systemic absorption(perioral numbness ,tachycardia, hypotension, arrhythmia) and in spinal anaesthesia no urinary retention .Hence although there is a chance of Obturator sparing in 3 in1 block but with ultrasound guidance it can be rectified to a certain extent and hence this block could be used as an alternative procedure where spinal anesthesia is highly contraindicated.
CONCLUSION To conclude US guided 3in1 block is safe and easy procedure. it requires minimal US training .it provides rapid and effective anaesthesia. Duration of analgesia is prolonged as US guidance is used chances of failure and obturator sparing are less compared to the conventional technique. Early ambulation is possible with 3in1 block and hemodynamic variability is minimal in 3in1 block an hence can be safely administered in cardiovascularily compromised patients. Hence it may be used an alternative to subarachnoid block in lower limb surgeries.
REFERENCES
.
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home