Official Journals By StatPerson Publication
|
Table of Content - Volume 12 Issue 2 -November 2019
. Comparison of clonidine and tramadol in supraclavicular block as adjuvant in upper limb surgery
Bhavna H Sojitra1*, Malti J Pandya2, Ronak Nagoria3
1Assistant Professor, 2Additional Professor, 3Post Graduate, Department of Anaesthesiology, SMIMER, Surat, INDIA. Email: bhsojitra2002@gmail.com
Abstract Objective: Comparing the effect of clonidine and tramadol as adjuvant in supraclavicular block in upper limb surgery was primary objective. Methods: In this randomized, prospective study, patients aged 18-65 years with American Society of Anaesthesiologists grade I- III were included and randomized onto three groups [Control, Clonidine(150µg) and Tramadol(100mg)]. Lignocaine and Bupivacaine were given in control group (Group A). Clonidine 150µg (Group C) and Tramadol 100mg (Group B) was given as adjuvant in respected group with local anaesthetic. Onset and duration of sensory and motor blockade with level of sedation and post-operative analgesia were noted. Results: These patients in all groups were comparable with respect to demographic characteristics Age, sex, weight and ASA grading. The mean onset of sensory blockade was 21.75±2.94 minutes in Group A, 13.50±2.35 minutes in Group B and 14±2.05 minutes in Group C. Total duration of sensory block was significantly (P<0.05) prolonged in clonidine group (242±30.37 minutes) and tramadol group (218±20.42 minutes) as compared to control group (170±13.6 minutes). The mean time of onset of motor block was 27.75±2.55 minutes in Group A, 19±5.25 minutes in Group B and 17.5±3.44 minutes in Group C. Total duration of motor block was significantly (p<0.05) prolonged in clonidine group (212.75±22.91 minutes) and tramadol group (198.5±16.31 minutes) as compared to control group (135.75±8.47 minutes). The mean of total duration of analgesia was 206.5±8.45 minutes in Group A, 426.5±32.16 minutes in Group B and 632.45±89.9 minutes in Group C. Sedation score was higher in clonidine group (score 3) and tramadol group (score 3) as compared to control group (score 2). Key Words: Analgesia, clonidine, supraclavicular block, tramadol.
INTRODUCTION Pain is a common human experience, a symptom frequently encountered in clinical practice. It is a consistent and predominant complaint of most individuals following most surgical interventions.32 Peripheral nerve blocks have wide applicability in the management of acute post-operative pain. A single bolus injection of local anaesthetic around a peripheral nerve trunk can give many hours of analgesia, but may also only serve to delay the onset of pain.32 Brachial plexus block is among the most commonly performed peripheral neural blocks for upper extremity. Supraclavicular approach is the most popular and widely employed, because of its ease, reliability and high success rate. This approach is attractive due to its effectiveness in terms of cost and performance, margin of safety, along with good postoperative analgesia. Although supraclavicular brachial plexus block is an excellent technique in experienced hands, a relatively high incidence of pneumothorax (1-6%) may occur. Nowadays different drugs have been used as adjuvant with local anaesthetics in brachial plexus block to achieve quick, dense and prolonged block. Drugs like morphine, pethidine, clonidine, dexmeditomidine, butorphenol, midazolam are commonly used along with local anaesthetics for this purpose. 2 Adjuvants to local anaesthetics for peripheral plexus blockade have been proposed to enhance the quality and duration of anaesthesia and post-operative analgesia. 21 Since 1980, clonidine has been used as an adjuvant to local anaesthetics in various regional techniques to extend the duration of block. 7 Clonidine is an α2- adrenergic agonist that has shown great analgesic potential, especially when given with local anaesthetics for peripheral nerve block. it reduces the onset time, improves the quality of nerve block and prolongs post-operative analgesia. 10 Opioids are synergistic with concomitantly administered local anaesthetics. This synergy is best seen at low dose of both opiates and local anaesthetics, thus improving quality of intra-operative analgesia by reducing side effects associated with high doses of local anaesthetics as well as providing post-operative pain relief for longer time. 32 peripheral opioids would allow analgesia without central side effects and without side effects of non-steroidal anti-inflammatory drugs. 23 Tramadol has peripheral local anaesthetic properties and has a small potential for serious adverse effects. Perimedullary tramadol enhances the duration and quality of local anaesthetics or is comparable to morphine and bupivacaine when administered as the sole drug. Tramadol also exhibits a non- central analgesic effect that has lead to is use as an adjunct to local anaesthetics in the peripheral nervous system. 21 The present study was undertaken to evaluate and compare the efficacy and side effects of clonidine and tramadol as adjuvant to local anaesthetics in supraclavicular brachial plexus block for upper extremity surgeries.
MATERIAL AND METHODS After approval from institutional ethical committee, present study was conducted in sixty patients of either sex between age group of 18 to 65 years undergoing upper limb orthopedic surgeries under supraclavicular brachial plexus block. In this prospective randomized and controlled study, patients were randomly divided into three groups of 20 each. Exclusion criteria: History of cardiac, respiratory, hepatic or renal disease, leprosy or convulsion, contra-indication for brachial plexus block such as bleeding disorders, cutaneous local infection, anomalies of neck and shoulder, fracture clavicle and patients known to be sensitive or allergic to any drug. Routine investigation like hemoglobin, urine albumin and sugar, blood sugar, urea, serum creatinine, x-ray chest PA view and ECG were advised. All patients were kept nil by mouth for ten hours prior to anesthesia. Informed and written consent was obtained from all sixty patients after detailed the intensity of pain using thee visual analogue scale (VAS). The patients were randomly and equally divided into 3 groups and total volume of drugs injected was thirty-five ml. All the study drugs were used preservative free. Group-A: Inj. Bupivacaine 0.5% Plain 20 ml + Inj. xylocaine 2% plain 10 ml + (Control) Normal saline 5 ml. Group-B: Inj. Bupivacaine 0.5% Plain 20 ml + Inj. xylocaine 2% plain 10 ml + Inj. (Tramadol) Tramadol 2 ml (100 mg) + Normal saline 3 ml. Group-C: Inj. Bupivacaine 0.5% Plain 20 ml + Inj. xylocaine 2% plain 10 ml + Inj. (Clonidine) Clonidine 1ml (150µg) + Normal saline 4 ml. On arrival in the recovery room, pre-operative baseline pulse rate, and blood pressure were noted. Intravenous line was secured and pre-loading was done with 10-15 ml/kg crystalloid solution. All patients were pre-medicated with injection glycopyrrolate 0.004 mg/kg body weight and injection midazolam 0.04 mg/kg body weight intramuscularly thirty minutes before surgery. In the operation theatre, after baseline recording of vital parameters, supraclavicular block was performed in supine position. A bolster of adequate size was placed between the shoulders; arm kept adducted and head was turned to opposite side. A 23G 1.5inch short beveled needle was introduced about 1.5 cm above the midclavicular point and directed caudal, backward and medially just lateral to subclavian artery pulsation. After hitting first rib, paresthesia was elicited over the hand by walking the needle along the first rib. Keeping the needle in same position and solution was injected slowly. Accidental intravascular injection was checked by frequent aspiration through the syringe. Intra operative, pulse, blood pressure, sensory and motor blockade as well as level of sedation were monitored. every 5 minutes for first 30 minutes, every 15 minutes up to the surgery, then 1 hourly up to 6 hours and then 2 hourly up to 12 hours and 15,18 and 24 hours interval. Oxygen saturation was also observed at above time interval up to 3 hours. The patients were also monitored for any intra-operative complication like hypotension, bradycardia, nausea, vomiting, dizziness, pruritus and respiratory depression. Sensory blockade was assessed by a 3 point sensory score.
Onset of sensory blockade was taken as the time between injection and the complete ablation of pinprick test (sensory score 2). Duration of sensory block was defined as the time from complete block to the return of the parasthesia (sensory score 1). If a sensory score of 2 was not achieved even after 45 minutes or if there was a sparing in any segment, the sensory analgesia was deemed to be not satisfactory and general anesthesia was supplemented and these patients were excluded from the study. Motor blockade was assessed by a 3 point motor score described by Bromage.
Onset of motor blockade was considered as the time from performance of block to the time when a complete inability to move fingers (score 2) was achieved. Duration of motor blockade was considered as time from complete motor block to the restoration of full flexion and extension of elbow wrist and fingers (score 0). Sedation was assessed by Ramsay Scale.
Postoperative analgesia was assessed by the 10 point visual analogue scale. The total duration of analgesia was considered as time from onset of sensory block to requirement of rescue analgesic.
Visual Analogue Scale (VAS)
10- Worst pain Injection Diclofenac Sodium 75 mg intramuscularly was given when VAS ≥3. Total analgesic requirements in 24 hours were recorded. The statistical analysis was done by ANOVA – Multiple Comparison test (Post hoc- turkey, Dunnet).
OBSERVATION AND RESULTS The presents study has been carried out in 60 patients in the age group of 18 to 65 years belonging to ASA Grade I or II scheduled for upper extremity surgery under supraclavicular nerve SMIMER, Surat. The Distribution of patients with respect to age was comparable in all three groups (p>0.05). Mean age in Group A was 34.90±11.69 years, Group B was 38.75±11.77 years and Groups C was 37.50±13.77 years. In Group A, 70 % of patients were male and 30 % of patients were female. In groups B, 85 % of patients were male and 15% patients were female. In groups C, 60 % of patients were male and 40 % of patients were female. The distribution of patients with respect to weight was comparable in all three groups (p>0.05). Mean weight of patients in Group A was 55.30 ± 7.24 kg. Group B was 53.50±4.97 kg and Group C was 58.85±4.54 kg. The average mean duration of surgery was 112.50± 16.50 minutes in Group A, 112.50±16.50 minutes in Group B, and 124.50±28 minutes in Group C. The mean duration of surgery in three groups was comparable (p>0.05)
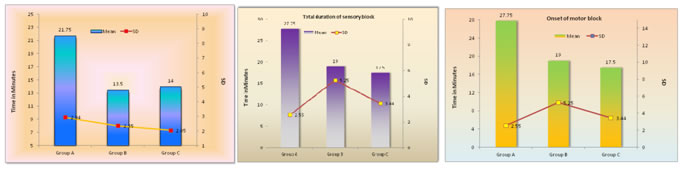
Figure 1: Onset of sensory blockade Figure 2 Figure 3
In figure 3, The mean onset of sensory blockade was 21.75 ± 2.94 minutes in Groups A, 13.50 ± 2.35 minutes in Groups B and 14 ± 2.05 minutes in Group C. There was no statistically significant difference in onset of sensory block between Group B and Group C, but onset of sensory blockade was significantly longer in Group A as compared to Group B and Group C (p<0.05). Total duration of sensory block was significantly (p<0.05), prolonged in clonidine group (242 ± 30.37 minutes) and tramadol group (218 ± 20.42 minutes) as compared to control Group (170 ± 13.6 minutes).
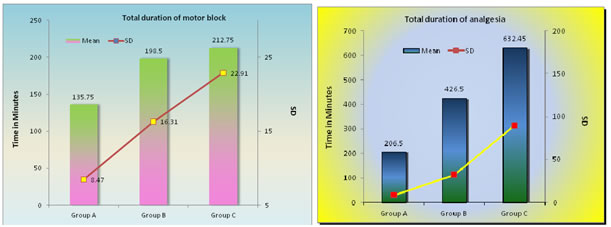
Figure 4 Figure 5
In figure 4, The mean time of onset of motor blockade was 27.75±2.55 minutes in Group A, 19±5.25 minutes in Group B and 17.5±3.44 minutes in Group C. There was no statistically significant difference in onset of motor block between clonidine and tramadol group, but onset of motor blockade was significantly longer in control group as compared to clonidine and tramadol group (p<0.05). Total duration of motor block was significantly (p<0.05) prolonged in clonidine group (212.75±22.91 minutes) and tramadol group (198.5±16.31 minutes) as compared to control group (135.75±8.47 minutes). However there was no statistically significantly (p<0.05) difference in duration of motor blockade between clonidine and tramadol group. There was statistically significant difference seen in sedation score from 30 minutes after performing the block to 4 hrs. At 45minutes sedation score 3 was attained in 16 patients in clonidine group, 12 patients in tramadol group and 4 patients in control group. None of the patient in study developed high level of sedation (score 5) intra-operatively. Post-operative analgesia was assessed by VAS. Total duration of analgesia considered as time from onset of sensory block to requirement of rescue analgesic. The difference in VAS between the groups were statistically significant from 4 hours to 6 hours after performing the block (p<0.05) In figure 5, The mean of total duration of analgesia was 206.5±8.45 minutes in Group A, 426.5±32.16 minutes in Group B and 632.45±89.9 minutes in Group C. The difference between three groups was statistically highly significant (p<0.001). thus post-operative analgesia was significantly prolonged in both clonidine and tramadol treated groups as compared to control group. Among three groups clonidine further prolonged the duration of post operative analgesia as compared to tramadol and control group and difference was highly significant (p<0.001). In Group A, 5% of patients required 2 injections, 75% of the patients required 3 injections and 20% of the patients required 4 injections. In Group B, 5% of patient required only 1 injection, 50% of patients required 2 injections, 25% of the patients required 3 injections, 20% of patients required 4 injections. In Groups C, 5% of patients required 1 injection, 90% of patients required 2 injections, and 5% of patient required 3 injections. Every patients required rescuer analgesics was 3.15±0.45 injections in Group C. Thus consumption of analgesics were significantly decreased in both clonidine and tramadol treated group as compared to control group (p<0.001). There was also statistically significant difference between clonidine and tramadol groups (p<0.001). Patients were observed for side effects like, hypotension, bradycardia, respiratory depression, nausea, vomiting and dizziness. The incidence of nausea and vomiting was 10% in tramadol group and 5% in control group and nil in clonidine group.
DISCUSSION A randomized prospective study was conducted in 60 patients of ASA I and II either sex and age group of 18-65 years, undergoing orthopedic surgery. Effect of clonidine (150 µg) or tramadol (100 mg) added to local anesthetics in supraclavicular brachial plexus block was compared. All patients were randomly and equally divided into 3 groups of 20 each were given supraclavicular block and total volume of drug given was thirty-five ml. Group-A (Control) : Inj. Bupivacaine 0.5% Plain 20 ml + inj xylocaine 2% plain 10 ml +Normal saline 5 ml. Group-B (Tramadol): Inj. Bupivacaine 0.5% Plain 20 ml + Inj. xylocaine 2% plain 10 ml + inj Tramadol 2 ml (100 mg) + Normal saline 3 ml. Group-C (Clonidine) : Inj Bupivacaine 0.5% Plain 20 ml + inj xylocaine 2% plain 10 ml + Inj. Clonidine 1ml (150 µg)+ Normal saline 4 ml. Thorough pre-anaesthetic check up was carried out. All the patients were explained about the procedure. Written and informed consent was taken and intravenous line was secured. Vitals parameters were noted in pre-anaesthetic room. Patients were preload with inj. ringer lactate solution 10-15 ml/kg body weight and premeditated with injection Glycopyrrolate. 0.004 mg/kg body weight and injection Midazolam 0.04 mg/kg body weight intramuscularly 30 minutes before the surgery. In the operation theatre, after baseline recording of vital parameters, supraclavicular block was performed in supine position. A bolster of adequate size was placed between the shoulders, arm kept adducted and head was turned to opposite side. A 23 G 4 cm short beveled needle was introduced about 1.5 cm above the mid-clavicular point and directed caudad, backward and medially just lateral to subclavian artery pulsation. After hitting first rib, parasthesia was elicited over the hand by walking the needle along the first rib, Keeping the needle in same position, solution was injected slowly, Accidental intravascular injection was checked by frequent aspiration through syringe. Just after giving supraclavicular block, pulse rate, blood pressure, sensory and motor block as well as level of sedation were monitored at every 5 minutes up to 30 minutes, at 45 minutes, at 1 hours and then at 1 hourly intervals up to 6 hours, then 2 hourly up to 12 hours, then at 15, 18 and 24 hours. In the present study mean age and weight of patient as well as duration of surgery and ASA status of patients were comparable among three groups. The mean onset of sensory blockade was 21.75±2.94 minutes in Gruop A, 13.50±2.35 minutes in Group B and 14±2.05 minutes in Group C. Among three group onset of sensory blockade was significantly longer in Group A as compared to Group B and Group C (P<0.05). Total duration of sensory block was significantly (P<0.05) prolonged in clonidine group (242±30.37 minutes) and tramadol gruop (218±20.42 minutes) as compared to control group (170±13.6 minutes). There was no statistically significant difference in onset and total duration of sensory block between clonidine and tramadol group (p>0.05) The mean time of onset of motor block was 27.75±2.55 minutes in Group A, 19±5.25 minutes in Group B and 17.5±3.44 minutes in Group C. Onset of motor block was significantly delayed in control group as compared to clonidine and tramadol group (p<0.05). Total duration of motor block was significantly (p<0.05) prolonged in clonidine group (212.75±22.91 minutes) and tramadol group (198.5±16.31 minutes) as compared to control group (135.75±8.47 minutes). However there was no statistically significant difference in onset and duration of motor blockade between clonidine and tramadol group. Pain was assessed by Visual Analogue Score. The total duration of analgesia was considered as time from onset of seensory block to requirdment of rescus analgesia. Inj Diclofenac Sodium 75 mg in was given at VAS ≥ 3. The mean of total duration of analgesia was 206.5±8.45 minutes in Group A, 426.5±32.16 minutes in Group B and 632.45±89.9 minutes in Group C. The difference among three groups was statistically highly significant (p<0.001). Thus post-operative analgesia was significantly prolonged in both clonidine and tramadol treated groups as compared to control group. Clonidine also prolonged the duration of post-operative analgesia as compared to tramadol and difference was highly significant (p<0.001). There was no statistically significant change in pulse rate, blood pressure and oxygen saturation among all three group (p>0.05). Sedation score was higher in clonidine group (score 3) and tramadol group (score 3) as compared to control group (score 2), though the patients were easily arousable on verbal stimulus in clonidine group and group and tramadol group. Patients were observed for side effects like; hypotension, bradycardia, respiratory depression, nausea, vomiting and dizziness. The incidence of nausea and vomiting was 10% in tramadol group and 5% in control group and nil clonidine groups. From the above results we concluded that:
Thus, Tramadol or clonidine can be used as an adjuvant to local anaesthetic for early onset and prolong duration of analgesia in supraclavicular brachial block. Clonidine proved to be a good alternative than Tramadol for providing longer duration of analgesia without side effects.
REFERENCES
|
|
 Home
Home