Official Journals By StatPerson Publication
|
Table of Content - Volume 12 Issue 2 -November 2019
.
Krishna Prasad T1, Gnanasekar N2*, Dilip Kumar G3
1Assistant Professor, 2,3Associate Professor, Department of Anaesthesiology, Shri Sathya Sai Medical College and Research Institute, (Sri Balaji Vidyapeeth, Deemed to be University), Thiruporur Guduvanchery Main Road, Ammapettai, Nellikuppam Post, Chengalpet Taluk, Kancheepuram - 603108, Tamil Nadu, INDIA. Email: drkrishna86@gmail.com
Abstract Background: Laryngoscopy and intubation are done to initiate general anesthesia which are associated with cardiovascular changes such as hypertension, tachycardia, dysrhythmia, increased catechola-minesand even myocardial ischemia. These responses are well tolerated in healthy patients, but may be dangerous in diabetic patients with elevated risk for coronary artery disease and other vascular insufficiencies. Materials and methods: This prospective, randomized, double blinded study was done with diabetic patients posted for elective surgeries under general anaesthesia. Before induction, a single dose of dexmede-tomidine 1µg/kg body weight (in 100ml NS) was administered intravenously over 15 min. The same amount of saline was administered to patients in the control group. The hemody-namic variables were recorded after 5 min of drug infusion, immediately before intubation and at the 1st, 3rd, 5th and 10th min after intubation. Results: Heart rate increased in both groups after intubation compared to pre intubation value and was significantly more in saline group compared to dexmedetomidine group (p =0.031) which was statistically significant. The blood pressure (both systolic and diastolic) response was significantly less in the dexmedetomidine group compared to the saline group. Conclusion: Pre-treatment with dexmedetomidine at a dose of 1µ/kg body weight in diabetic patients blunts the hemodynamic responses to laryngoscopy and tracheal intubation. Key Word: laryngoscopy, intubation, dexmedetomidine, tachycardia, diabetic
INTRODUCTION Diabetes mellitus is associated with macrovascular and microvascular complications like coronary artery and cerebrovascular diseases. India being the diabetic capital of the world, the chances of every alternate patient anaesthetized being diabetic is very high. It is also not possible to evaluate every patient for vascular complications of diabetes. There is a high possibility that tachycardia and hypertension would be poorly tolerated by these patients during laryngoscopy and intubation for general anaesthesia. Any noxious airway manipulation in supraglottic region and trachea elicits a cardiovascular response which is initiated by proprioceptors consisting of mechanoceptors with myelinated fibres of small diameter located in close proximity to the airway mucosa. The glossopharyngeal and vagal afferent nerves transmit these impulses to the brain stem, which, in turn, causes widespread autonomic activation through both the sympathetic and para sympathetic nervous systems.1,2 Several techniques have been proposed to prevent or attenuate these hemodynamic responses such as deepening the plane of anaesthesia, pretreatment with nitroglycerine, β blockers, calcium channel blockers, opioids etc. Hemodynamic changes start within seconds of direct laryngoscopy, and there is a further increase in heart rate and BP with passage of the tracheal tube. These hemodynamic changes might result in myocardial ischemia without causing much harm to majority of the patient population. These changes would be of greater risk and poorly tolerated by diabetic patients. The magnitude of the response is greater with increasing force and duration of laryngoscopy. As a premedicant, dexmedetomidine, at i.v. dose of 0.33 to0.67 µg/kg given 15 minutes before surgery, seems efficacious, while minimizing the cardiovascular side effects of hypotension and bradycardia. Within this dosage range, it reduces general anaesthetic requirements and effectively attenuates the hemodynamic response to laryngoscopy and tracheal intubation. The α2-adrenergic agonists provide sedation, anxiolysis, hypnosis, and sympatholysis by acting on α2 receptors in the locus caeruleus and analgesic action at α2 receptors within the locus caeruleus and the spinal cord. Dexmedetomidine is a more selective α2 agonist with a 1600 greater selectivity for the α2 receptor compared with the α1 receptor. The quality of sedation produced by dexmedetomidine is different compared with that produced by other sedatives acting through the GABA systems. The sedation has been described as being very easy to wake up and having the ability to follow commands and cooperate while being tracheally intubated and there is limited respiratory depression, providing wide safety margins.3,4 Many drugs were tried and tested for obtunding the hemodynamic response to laryngoscopy and intubation. Many studies conducted with dexmedetomidine were done on healthy volunteers and patients, who generally tolerate this noxious stimulus without any untoward complications. Only limited data is available on dexmedetomidine attenuating these responses in diabetic patients posted for elective surgeries under general anaesthesia. Hence, we conducted this study on diabetic patients to compare the hemodynamic changes associated with laryngoscopy and endotracheal intubation with dexmedetomidine.
MATERIALS and METHODS This was a prospective, randomized, single centered, double blinded study conducted over a period of 6 months after obtaining approval from the Institutional Ethics Committee. The trial was done with diabetic patients posted for elective surgeries under general anaesthesia. Diabetic patients between 25 to 60 years of age of physical status American society of Anaesthesiology (ASA) class II with HbA1C between 6-8% were included in the study. Patients with physical status ASA III and above, emergency surgeries, pregnant patients and patients not willing to participate in the study were excluded from the study. Patients were randomly allocated into 2 groups (Group A and Group B) using computer generated randomization to receive either dexmedetomidine (Group A, n=33) or 0.9% saline (Group B, n=33). All patients were evaluated a day before surgery. The study protocol was explained to the patients in their own language and written informed consent taken before posting for surgery. Patients were pre-medicated with Tab. Alprazolam 0.5mg orally and were fasted for 8 hours from night before surgery. 100 ml saline bottles containing aqueous solutions of either dexmedetomidine 1µ/kg or plain saline were prepared in a double-blinded fashion by a team member who was not involved in data recording. Electrocardiogram (ECG), pulse oximetry, systolic blood pressure, diastolic blood pressure, mean arterial blood pressure were monitored. After 5 min of stable cardiovascular variables, baseline hemodynamic variables were noted. Before induction of anesthesia, a single dose of dexmedetomidine 1µg/kg body weight was administered intravenously over 15 min. The same amount of saline was administered to the patients in the control group. After 5 min of infusion of the study drug, the hemodynamic variables were once again recorded. General anesthesia was induced with fentanyl 2µg/kg and Propofol 2mg/kg. Tracheal intubation was facilitated by administering 0.1mg/kg Vecuronium bromide and after ventilating with mask for 3 min with 100% oxygen. Direct laryngoscopy and intubation was performed by the same experienced anaesthesiologist. The duration of laryngoscopy and intubation limited to minimum possible time and was less than 15 seconds for all patients. Hemodynamic variables were recorded again, immediately before intubation that is 2 min after administering vecuronium and at the 1st, 3rd, 5th and 10th min after intubation. Inhalation agents were given only after the study period and the surgery commenced. Any hemodynamic deteriorations were noted. The primary outcome of the study was to compare the attenuation of hemodynamic response to laryngoscopy and intubation in patients receiving single dose of dexmedetomidine versus placebo. The safety of the drug in terms of any hemodynamic instability throughout the surgery and any other post-operative complications were also noted. All the measured parameters were compared between the two groups. Statistical analysis: The Statistical analysis was performed by STATA 11.1(Stata Corp College station TX USA). Student’s t-test (Paired) was used to find the statistical significance of pulse rate, blood pressure and mean arterial pressure (MAP). The above three parameters compared baseline with 5min after study drug infusion, 2 min after induction, 1st, 3rd, 5th and 10th min after intubation. The above three parameters were also compared 2min after induction (pre intubation) with 1st, 3rd, 5th and 10th min after intubation. Chi square test was used to compare gender between the groups. Independent sample t-test was used to find the significance of between the groups with the age. The continuous variables were described as mean ± SD. Categorical variables are described as frequency and percentage. P<0.05 was considered as statistically significant.
RESULTS All the 66 patients randomized were included and analysed for the study. The demographic data was comparable between the two groups in terms of age, sex, BMI and ASA physical status. HbA1C levels were comparable between the two groups (Table 1). Table 1: Demographic profile between the 2 groups
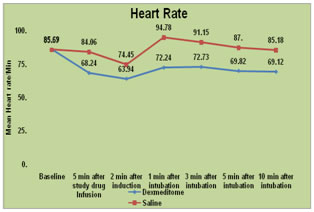
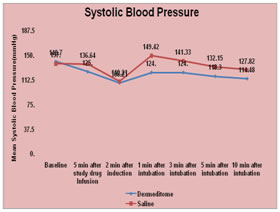
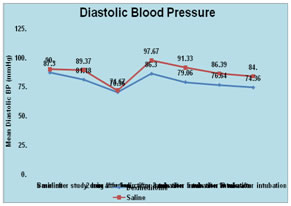
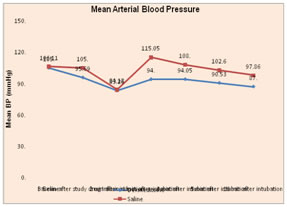
A]: Hemodynamic changes before intubation after drug infusion in both the groups Heart rate significantly decreased from baseline level in group A (-26%) compare to group B (-2%) (p=0.005) which was statistically significant. Systolic, diastolic and MAP decreased more in group A (11%, 7% and 9%) compared to group B (2%, 1% and 2%) but all were statistically insignificant. B]: Hemodynamic changes after intubation compared to pre intubation values (2 min after induction) in both the groups Heart rate increased in both the groups after intubation compared to pre intubation value (2min after induction) and was significantly more in group B (33%) compared to group A (11%) (p =0.031). Systolic blood pressure raised significantly less (8%) after intubation in group A compared to pre intubation values than in group B (27%) (p= 0.042) and return to pre intubation values early in group A compared to group B. Diastolic BP raised significantly less in group A (7%) after intubation compared to pre intubation values than in group B (27%) (p= 0.031) and return to pre intubation values early in group A compared to group B. MAP raised significantly less (8%) after intubation in group A compared group B (27%) (p=0.042). Graph 1: Heart rate variation during the study period; Graph 2: Systolic pressure variation during the study period
Figure 3: Diastolic blood pressure variation during the study period; Figure 4: Mean arterial blood pressure variation during study period
DISCUSSION The results of our study have demonstrated that adding dexmedetomidine as a pre-medicant in diabetic patients effectively attenuates the hemodynamic stress response to laryngoscopy and intubation as evidenced by the significantly lesser raise in heart rate and blood pressure in these patients. Diabetes mellitus is considered to be a fore runner of micro vascular and macro vascular diseases. Hemodynamic instability in the form of end organ involvement and vascular complications may be encountered during anaesthesia and surgery. Attenuation of pressor response during laryngoscopy has been one of the most researched topics in anaesthesia. Increased sympatho-adrenal activity may result in hypertension, tachycardia and dysrhythmias which is usually unpredictable, transient and variable. This response is probably of no consequence in healthy individuals, but either or both may be precarious to those with coexisting conditions like diabetes, hypertension, myocardial insufficiency and cerebrovascular diseases. Diabetic patients have shown variable sensitivity patterns to the catecholamines and their reuptake process. Diabetic autonomic neuropathy (DAN) and atherosclerotic vascular changes are well documented phenomenon in these patients with predominant effect on the cardiovascular system. Many randomized trials have been conducted evaluating the hemodynamic blunting response of dexmedetomidine comparing with various drugs and their combination but were done only on healthy patients. Burgo et al and Khan et al have shown a lesser heart rate response following intubation in diabetic patients in whom 20% of the patients had DAN. Vohra et al have shown a raised hemodynamic response in diabetic patients compared to the non-diabetics.5-7 Following the contradictory responses in the previous studies, we enrolled diabetic patients who may not tolerate the response well.Stoelting et alstudied that the best way to prevent laryngoscopic response was to minimize the duration of laryngoscopy and intubation. He noted that if laryngoscopy and intubation were performed within 15 seconds, the hemodynamic changes seemed to be minimal8 Hence, we restricted our duration of laryngoscopy and intubation to less than 15 seconds. Yildiz et al studied the effects of dexmedetomidine on hemodynamic response to laryngoscopy and intubation in elective minor surgeries and found that preoperative administration of a single dose of dexmedetomidine resulted in progressive increases in sedation, blunted the hemodynamic responses during laryngoscopy, and reduced opioid and anaesthetic requirements. Furthermore, dexmedetomidine decreased both blood pressure and heart rate as well as post operative recovery time.9 Our study findings correlated with the above results with the same single dose of dexmedetomidine of 1 mcg/kg though our target included diabetic patients. Sulaiman et al studied the effects of dexmedetomidine on attenuation of stress response to endotracheal intubation in patients undergoing elective off-pump coronary artery bypass grafting. They concluded that pretreatment with dexmedetomidine is a safe and effective method to attenuate the hemodynamic response to laryngoscopy and intubation. In patients undergoing myocardial revascularization, even if the patients are receiving beta blockers, dexmedetomidine can be considered before induction of general anaesthesia.10 We too noticed no significant hemodynamic instability or any other side effects in our study. There were some drawbacks of the study. First, we excluded patients with anticipated difficult airway in order to stick on to 15 seconds of intubation time. The effectiveness of the study drug would have been better established in these patients since the hemodynamic response correlates directly with the force and duration of laryngoscopy. Second, establishing an arterial cannula would have accurately delineated the blood pressure response which we didn’t perform due to limitation of resources. Third, we did not delineate insulin dependent from non-insulin dependent diabetic patients where the autonomic neuropathy incidence is high. Further research and meta-analysis are required in diabetic patients undergoing general anaesthesia to understand the drug-receptor interaction and identifying the risk diabetics to optimize the hemodynamic responses during surgery.
CONCLUSION We concluded that pretreatment with dexmedetomidine at a dose of 1µ/kg body weight as 15 min infusion prior to induction of anaesthesia is a safe and an effective method to attenuate the hemodynamic responses to laryngoscopy and intubation in diabetic patients receiving endotracheal anaesthesia.
REFERENCES
|
|
 Home
Home