Official Journals By StatPerson Publication
|
Table of Content - Volume 12 Issue 2 -November 2019
. Efficacy of dexamethasone in reducing the severity of postoperative sorethroat after endotracheal intubation
K Chandra Mohan1, R Arun Kumar2*, A T Sathiya Vinotha3, D Dhatchinamoorthi4
1,4Consultant Anaesthesiologist, Department of Anaesthesiology, Kovai Medical Center and Hospital Limited, Coimbatore, INDIA. 2Associate Professor, Department of Anaesthesiology, PSG Institute of Medical Sciences and Research, Coimbatore, INDIA. 3Assistant Professor, Department of Pharmacology, KMCH Institute of Health Sciences, Coimbatore, INDIA. Email: shivaaniarun76@gmail.com
Abstract Background: Airway management with cuffed endotracheal intubation is an integral part of an anaesthesiologist’s responsibilities. Local irritation and inflammation caused by prolonged inflation of the cuff can result in minor sorethroat to more serious transglottic complications inherent to the usage of cuffed endotracheal tube. Many studies have been performed and published exploring the measures to minimize or eliminate post-intubation morbidities. Aim: The aim of our study was to evaluate the efficacy of intravenous administration of Dexamethasone in reducing the incidence and severity of postoperative sore throat in patients receiving general anaesthesia with cuffed endotracheal intubation. Materials and methodology: 100 patients of age group between 18 – 65 years belonging to ASA 1 and 2 of both the sexes posted for elective surgeries under general anaesthesia with endotracheal intubation participated in this study. Patients were randomly allocated to one of the two groups, 50 in each by using envelope method. Group C: Control group was given 2 ml Normal Saline Intravenously and Group D: Dexamethasone group was given 2 ml Dexamethasone 8mg Intravenously. Observation and Results: Statistical analysis was done using SPSS PC (11.5) version. Student’s t-test was used to compare the mean difference in quantitative variables and Chi-square test was used to study the association among qualitative variables. p value < 0.05 was considered statistically significant. Conclusion: The conclusion of our study is that single dose of 8 mg prophylactic Dexamethasone given intravenously reduces effectively the incidence and severity of sore throat after general anaesthesia with cuffed endotracheal intubation. Key Word: Dexamethasone, Post operative sorethroat, Endotracheal intubation
INTRODUCTION Airway management with cuffed endotracheal intubation is an integral part of an anaesthesiologist’s responsibilities ensuring adequate ventilation and preventing aspiration of secretions. In addition, the wastage of anaesthetic gases and pollution of the operation theatres are also reduced substantially. However, local irritation and inflammation caused by prolonged inflation of the cuff can result in minor sorethroat to more serious transglottic complications (like vocal cord problems and subglottic stenosis), inherent to the usage of cuffed endotracheal tube. The minor sequelae of sore throat from the use of cuffed endotracheal tube results in up to 90% incidence in the postoperative period. Several factors like trauma to laryngopharyngeal mucosa during laryngoscopy, contact of tracheal tube with the vocal cords and pharyngeal wall resulting in oedema, pressure affecting the tracheal mucosal capillary perfusion, cuff design, oral suctioning, placement of nasogastric tube, mobility of the tube inwards, outwards or sideways can contribute to sorethroat. After general anaesthetic one may develop a sore throat which can range between minor discomfort to a more severe continuous pain. One may also have a very dry throat or feel pain on speaking or swallowing and the symptoms may disappear after a few hours but may take a two days or more to settle down completely. Many studies have been performed and published exploring the measures to minimize or eliminate post-intubation morbidities, viz,
Dexamethasone is a potent corticosteroid with anti-inflammatory, analgesic and antiemetic properties and has been reported to reduce the postoperative pain and swelling following oral surgeries.2,3,13
AIM The aim of our study was to evaluate the efficacy of intravenous administration of Dexamethasone in reducing the incidence and severity of postoperative sore throat in patients receiving general anaesthesia with cuffed endotracheal intubation.
MATERIALS AND METHODS A study titled “Efficacy of Dexamethasone in reducing the severity of postoperative sore throat after endotracheal intubation” was done after obtaining ethical committee clearance from the institution and informed written consent were obtained from all the patients who participated in this prospective and randomised study. 100 patients of age group between 18 – 65 years belonging to ASA 1 and 2 of both the sexes posted for elective surgeries under general anaesthesia with endotracheal intubation participated in this study. Inclusion criteria
Exclusion criteria
Routine pre-operative assessment was done and the patients were kept nil per oral from 10 pm the day prior to surgery. Informed written consent was obtained. All the patients were pre-medicated with Tab. Pantoprazole 40 mg and Tab. Alprazolam 0.25mg at night the day prior to surgery and at 6 am on the day of surgery. Patients were randomly allocated to one of the two groups, 50 in each by using envelope method. Group C: Control group was given 2 ml Normal Saline iv Group D: Dexamethasone group was given 2 ml Dexamethasone 8mg iv Patients were connected to ASA standard monitors – ECG, Non invasive blood pressure (NIBP), pulse oximeter (SpO2) and baseline readings recorded. An 18 G Intravenous catheter was inserted and intravenous fluids started. Preoxygenation was done with 100 % Oxygen for 3 minutes and general anaesthesia was instituted with intravenous Fentanyl 2mcg/kg, Lignocaine (preservative free) 20mg and Propofol 2mg/kg intravenously for induction. Mask ventilation was done for 3 mins and Endotracheal intubation was facilitated with 0.5 mg/kg Atracurium besylate. High volume low pressure endotracheal tube from the same manufacturer (Rusch Inc.) were used for all patients from both groups. Male patients received 8 and 8.5 mm and female patients received 7 and 7.5 mm inner diameter endotracheal tubes respectively. Intubation was performed with a standard MacIntosh curved blade size 3 or 4. Application of external laryngeal pressure to aid endotracheal intubation and number of attempts at laryngoscopy were recorded. The cuff was inflated with air just to achieve an airtight seal in the presence of intermittent positive airway pressure ventilation. Intra cuff pressure was adjusted as required every 30 minutes to 25 – 40 cm H20 (18 – 30 mm Hg) using a cuff pressure monitor to limit nitrous oxide related intracuff pressure increase. Anaesthesia was maintained with oxygen and nitrous oxide in a ratio of 33:66 in isoflurane. Muscle relaxants and analgesia were repeated when required at regular intervals. Ventilation was adjusted to maintain normocarbia (35 – 40 mmHg). Oral or nasal airways were not placed in any patient. Coughing or bucking on the ETT if any, were recorded. At the end of the surgery, Ondansetron 0.1mg/kg i.v was administered and muscle relaxation was reversed with a combination of Neostigmine 0.05 mg/kg and Glycopyrrolate 0.01 mg/kg. Oropharyngeal suction before extubation was done under direct vision to avoid trauma to pharyngeal mucosal tissues as well as to confirm that secretions were completely removed. Presence of blood in oropharyngeal suction or on the endotracheal tube after extubation excluded these patients from the study. In the Post anaesthesia care unit, presence of soreness of throat was evaluated by a trained observer who, along with the patient, was blinded to the study group assignment. The assessment was done using visual analogue scale (linear 10 cm, starting from 0 = no pain to 10 = worst imaginable pain) at rest and with effort (swallowing movement) at one hour, three hour, six hour, 12 hour and 24 hour periods. Statistical analysis: Our randomized double blind placebo controlled prospective study comprised of 100 patients, 50 in each group. Group C-Control Group (n=50) Group D- Dexamethasone (n=50) Statistical analysis was done using SPSS PC (11.5) version. Student’s t-test was used to compare the mean difference in quantitative variables and Chi-square test was used to study the association among qualitative variables. p value < 0.05was considered statistically significant. OBSERVATION AND RESULTS Table 1: Demographic details - Group C and Group D
Table 2: Intra Cuff pressure (cm of H20) at various periods
Table 3: Incidence of sorethroat between two groups
Table 4: VAS scores at rest
Table 5: VAS scores at effort
Table 6 :Parameters observed intraoperatively
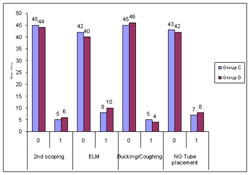
Figure 1: Incidence of 2nd attempt, External laryngeal pressure, Bucking/Coughing on ETT between groups
DISCUSSION Sorethroat though a minor complaint following endotracheal intubation, is one of the most common and irritating complaints similar to Post operative nausea and vomiting (PONV); and if associated with cough, it increases the pain and oozing when there is abdominal or thoracic wounds. Postoperative sore throat is a symptom caused by many factors, such as the intubation procedure, cuffed endotracheal tube, intracuff pressure and the use of stylets or lubricants. Stenqvist O et al16in his studies showed the incidence of postoperative sore throat does not necessarily reflect damage caused by the endotracheal cuff only. In our study, Dexamethasone group had a statistically significant reduction in the incidence (18% Vs 54%) and severity of sore throat after general anaesthesia with endotracheal intubation compared to the placebo group. Contrarily the occurrence of sore throat was similar between the two groups, in respect to the duration of surgery, the number of laryngoscopic attempts and intracuff pressure. In our study, patients from both groups had their intracuff pressure checked every half hourly and maintained within acceptable limits. Jenson PJ et al6, El Hakim et al4 and Mc Hardy FC et al9 in three different studies concluded that the incidence of sorethroat ranges from 6.6 – 90%, a wide spectrum. 54% with sorethroat in our study is indicating that every alternative patient had postoperative sore throat. Stout DM et al17 showed a higher incidence of sore throat caused by larger size endotracheal tube compared with smaller size tube. The size of the endotracheal tube in both age groups was similar in both groups, not letting the size affect the incidence of sore throat. The duration of surgery did not alter the incidence of sore throat in our study, in contrast Jensen PJ et al6 where they found a direct relation with the length of cuff – tracheal contact. In respect to the cuff design and lubrication, Loeser EA et al7 in their study demonstrated high volume low pressure cuffs were associated with higher incidence of sore throat due to the larger area of contact with the tracheal mucosa but we did not have any such increase in the incidence of sore throat in spite of using high volume low pressure cuffs ( Rusch AVT Ind. Ltd.,) in our study, which is possibly explained by the improvement in the endotracheal tubes and cuff designs over the last three decades.Stanley TH et al15showed a significant increase in cuff volume and cuff pressure after use of nitrous oxide intraoperatively and this has been blamed for increase in the incidence of sorethroat. But in our study, though the cuff pressure and cuff volume increased due to the use of nitrous oxide, it was monitored every 30 minutes by a cuff pressure monitor and brought back to acceptable limits, thus not allowing it to affect the incidence of sore throat. 64.5% of postoperative sore throat was reported by Monroe MC et al11 in patients with blood tinge of airway instruments like endotracheal tube tip, compared to those 30.9% without blood tinge, due to improper suctioning which was wrongly attributed to the increased sore throat incidence. None of our patients from either group had any blood staining. Sang-Hyan Park et al12concluded prophylactic administration of 0.2 mg/kg body weight Dexamethasone significantly decreased the incidence and severity of sore throat and hoarseness 1 hour and 24 hours after tracheal extubation of a double lumen tube. We have used Dexamethasone 8 mg IV, as the exact dose is not known and the results of our study agree with the above study. Hamelberg W et al5 found insignificant decrease in the incidence of sore throat when 1% hydrocortisone ointment was applied to the endotracheal tube. Stride18 used the same method together with standardized anaesthesia and direct questioning technique and concluded that hydrocortisone ointment was ineffective in the prevention of postoperative sore throat due to the presence of additive substances which are irritating to the tracheal mucosa. Dexamethasone being better anti-inflammatory agent compared to hydrocortisone probably explains better results in reducing sorethroat.Dexamethasone being a steroid may produce complications like gastritis, avascular necrosis, delayed wound healing, glucose intolerance and susceptibility to infection, but a single bolus dose of intravenous dexamethasone does not produce these complicationsas evidenced by Melby JC et al.10 The results of our study very well correlates with the findings of Wang et al19 which primarily studied the effect of dexamethasone on postoperative nausea and vomiting (PONV) and these results were consistent with the study by Siji Thomas et al.14 Postoperative sore throat is a symptom caused by many factors, such as the intubation procedure, cuffed endotracheal tube, intracuff pressure and the use of stylets or lubricants. Methods to minimize sore throat will bring patient satisfaction, less pain and less oozing, thereby promoting early discharge from the recovery room and hospital. One such method is using intravenous Dexamethasone. Draw backs of this study
CONCLUSION The conclusion of our study is that single dose of 8 mg prophylactic Dexamethasone given intravenously reduces effectively the incidence and severity of sore throat after general anaesthesia with cuffed endotracheal intubation. Dexamethasone minimizes two of the minor, but irritating postoperative problems of general anaesthesia with endotracheal intubation i.e. PONV and postoperative sore throat and hence it may be recommended in patients undergoing surgery under general anesthesia.
REFERENCES
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home