Official Journals By StatPerson Publication
|
Table of Content - Volume 12 Issue 2 -November 2019
Balakrishnan A*, Ashwini B**
*Professor, **Junior Resident, Department of Anaesthesia, Sree Mookambika Institute of Medical Sciences, Kulasekharam, Tamil Nadu. Email: balki09@gmail.com
Abstract Background: Pain following surgery is a universal phenomenon. Yet, it is often underestimated and under treated being purely subjective pain and its intensity vary widely among patients. The identification of opiate receptors in the early 70's gave a new meaning to the pain relief. Spinal administration of opioids has become common in recent years and is effective in treating the same. Buprenorphine, a thebaine derivative, an Opioid agonist-antagonist provides good post-operative analgesia when used as an ajuvant in Subarachanoid block. Aim of study: To evaluate the efficacy of spinally administered Buprenorphine hydrochloride in providing post-operative pain relief in caesarean section with two different doses of 60mcg and 120mcg. Materials and methods: A total of 100 pregnant females in the age group 18-35 years were randomly selected for this study. All patients belonged to ASA physical status 2 were divided in two groups 50 each. The patients were given 60mcg and 120mcg of Buprenorphine as adjuvant with Bupivacaine hydrochloride in sub arachanoid block. The duration of postoperative analgesia and side effects were noted. Informed consent was obtained. Descriptive and analytical statistics were performed by student “t” test. A P value of less than 0.05 was considered statistical significant. Result: It has been found in this study that 120 mcg of spinal buprenorphine provides pain relief for 37±7.238hours.Pain relief provided by 120mcg spinal buprenorphine is more constant, reliable and predictable than 60 mcg spinal buprenorphine. Conclusion: The highly lipophilic thebaine derivative opioid partial agonist Buprenorphine is a promising agent in relieving acute post-operative pain in caesarean delivery by single shot spinal route with good margin of safety. Key Word: Subarachanoid block, Buprenorphine, Bupivacaine hydrochloride
INTRODUCTION As international Association for the study of pain defines, PAIN is "an unpleasant sensory and emotional experience associated with actual or potential tissue damage or described in terms of such damage".1 The identification of opiate receptors in the early 70's gave a new meaning to the pain relief. Spinal administration of opioids has become common in recent years and is effective. First spinal analgesia was given by J. Leonard Corning, a neurologist in 1885. He accidentally pierced the duramater while experimenting with cocaine on the spinal nerves of a dog. Later he deliberately repeated the intradural injection in humans.2 First planned spinal analgesia for surgery in man was performed by AugustBier on 16 August 1898.3The procedure was actually first attempted on Bier by his assistant Hildebrandt.
AIMS AND OBJECTIVES To evaluate the efficacy of spinally administered Buprenorphine hydrochloride in
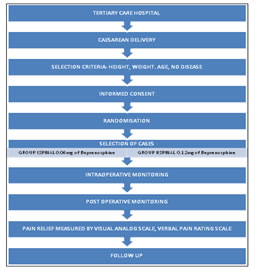
METHODOLOGY A total of 100 pregnant females in the age group 18-35 years, weighing 41-75kgs, of the height 140-165 cms were randomly selected for this study. All patients belonged to ASA physical status 2. All diseases like respiratory, cardio vascular, neurological or any other systemic disorders were excluded. Informed consent was obtained from all the 100 patients after a detailed explanation of the procedure to be done. Basic data like pulse rate, blood pressure, respiratory rate, haemoglobin estimations, urine analysis for albumin and sugar, blood urea and sugar, and serum creatinine were recorded. X-ray chest and Electro cardiogram were taken if required. All the patients were taught to assess the intensity of pain using the Visual analogue pain scale. Pre-medication: Patients were not pre medicated to avoid any possible interference with the outcome of study. Inside the operation theatre, once again the pulse rate, blood pressure and respiratory rate were recorded. The patients were cannulated with 18G IV cannula and Ringer lactate started. The patients were randomly divided into two groups of 50 each. The Lumbar puncture was performed in right lateral position with 22G spinal needle, through the L3-L4 inter space under strict aseptic precautions. Group I: Patients received 60mcg of Buprenorphine hydrochloride along with 1.8ml of Bupivacaine hydrochloride intrathecally. Group II: Patients received 120mcg of Buprenorphine hydrochloride along with 1.8ml of Bupivacaine hydrochloride intrathecally. After the subarachnoid injection, patients were put in supine position and with left lateral tilt. Oxygen 4L/minute was administered through face mask. When the sensory blockade reached T6 level surgery was started. Pulse, B.P and respiratory rate were monitored and recorded in the proforma chart every 2 min for first 10 min and 15 min intervals thereafter. If there was any fall in BP Intravenous fluids were rushed and if fall was more than 30mm of Hg or 25% below the baseline value, intravenous Ephedrine given in titrated doses. If bradycardia (pulse rate below 60/minute) occurred, injection Atropine sulphate 0.6mg Intravenous was given. All the patients were infused with injections oxytocin 10 units in Ringer lactate after the delivery of the baby. No narcotics or analgesics were administered intra-operatively. If patients were anxious, they were given Inj. Midazolam 1mg intravenously to allay their anxiety. The APGAR score of neonate was calculated at 1 and 5 min. The occurrence of side effects during the procedure like, hypotension, bradycardia, nausea, vomiting, itching, shivering, difficulty in breathing were noted. Level of sensory block was assessed by pin-prick and once it reached T10 level, this duration was considered as onset of analgesia. Level of maximal sensory block was later noted and it was repeated after sixty minutes Motor block was assessed 10 min after injection by using Bromage Epidural scale, which states. After the completion of surgery, the patients were observed in the recovery room, till they recovered their motor power adequately and were then transfered to the post operative ward. Post operative follow up: Vital signs were monitored for 12 hours. The patients were instructed before leaving the operation theatre, to inform about the pain and once again, they were taught about the visual analogue scale. No narcotics or analgesics were given and the nursing staff and surgeons were informed about this. Any untoward side effects like, nausea, vomiting, urinary retention, respiratory depression, pruritis, drowsiness, headache, back ache, shivering etc., were noted for The duration of analgesia was considered as the period when the visual analogue score reaches 5 or when patients complain of moderate pain (verbal pain rating scale) whichever is earlier. These data were then compiled to study the efficacy of the two given doses of Buprenorphine.
Flow chart of methodology
OBSERVATION AND RESULTS Of the 100 patients, 50 patients belonged to group I (60mcg subarachanoid buprenorphine) and other 50 patients belongs to group II (120mcg of subarachanoid buprenorphine) Duration of Analgesia: The range of analgesia was variable in both groups with 16 to 39 Hours in group I and 24.50 to 50.75 Hours in group II. The mean duration of analgesia was 27.686 ± 4.819 Hours in groups and 37.097±7.238 Hours in group II
Absolute Analgesic Period: By verbal pain rating scale, the time taken for mild pain was assessed and it was 4.495 hours in group I and 6.496 hour in group II and this was again statistically significant.
Adverse effect: The adverse effects noted in both the groups are mentioned below by the number of patients having those complaints.
The duration of Analgesia was higher with 120mcg of Buprenorphine compared to 60mcg intrathecally. DISCUSSION This study was a randomised controlled trial, Variables like age, weight, height were all standardised in both the groups as confirmed by the statistical data. Anaesthetic Variables: The Maximal sensory block (Between T6 andT4) and the onset of analgesia, though numerically had variations, statistically both the groups were comparable. Similarly the motor block quality of anaesthesia and two segment regression time were similar in both the groups. Duration of analgesia: Theduration of analgesia was higher with 120mcg spinal buprenorphine (37.097±7. 238 Hours) than with 60mcg spinal buprenorphine(27.686±4.819Hours). This was proved to be statistically significant. But the range of values varied in both the groups. The minimum duration of analgesia is 16 Hours in 60mcg of spinal buprenorphine and 24.30 Hours in 120mcg of spinal buprenorphine. The Duration of analgesia is stratified in the table below. It shows thatvariations are high in group I. In group I 30 patients have duration of analgesia between 24 to 30 hours. In Groups I duration of analgesia varies between 18 Hours to 42 Hours In group II duration of analgesia varies between 24 Hours to more than 48NHours. In Group II 28 patients have duration of analgesia between 30 to 42 Hours.
So the duration of analgesia is more in group II than group I Mild pain: By verbal pain rating scale, mild pain occurred first within mean of 4 Hours38 Minutes in Group I and 6 Hours 38 Min in group II. So the absolute analgesia period in group II is more when compared to group I The neonatal outcome were comparable in both groups. U.D Interval: U.D Interval is of great significance and after 90 seconds, fetal asphyxia and acidosis begin to become apparent, probably as a result of partial placental separations, impaired placental blood flow and premature fetal respiratory efforts causing aspiration of liquor. In group I, U.D Interval is 36.78 seconds and in group II it is 36.58 seconds. Side Effects: The incidence of nausea, vomiting and urinary retention were all numerically bit higher in group II, but statistically it was not significant. Urinary retention occurred in 7 patients in group I whereas in 11 patients in group II. The frequency of other side effects were comparable in both the groups. All these side effects were managed without any need for specific treatmentor intervention. Hypotension occurred in 14 patients in group I and 13 patients in group II. This may lead to nausea, vomiting, feeling unwell and even maternal death. The uterine blood flow and intervillous perfusion decreases, this inducing fetalbradycardia, acidosis abnormal APGAR and neuronal behavioural scores when maternal systolic blood pressure drops more than 30 % of base line or stays less than 80 mm of Hg for more than 4 minutes. The occurrence of hypotension may be due to aortocaval compression also. Respiratory depression did not occur in any of the cases in the study probably due to better counselling, vigilant monitoring, use of the lipophilic drug at a lower(lumbar) level, position of the patient, proper selection of the patient and avoidance of other narcotics. Vital parameters like pulse, blood pressure and respiratory rate remained normal throughout the study showing the cardio respiratory stability of the drug. Pain relief is the most gratifying service that can be offered to any patient. Postoperative analgesia after cesarean section poses unique clinical challenges to anesthesiologist as it should allow early ambulation of the mother to prevent thromboembolic episodes and ensure bonding with the baby. It should have no undesirable effects on the mother or newborn. SAB with LA alone provides limited postoperative analgesia. Opioid adjuvants can subjugate this limitation. Buprenorphine is a highly potent and lipophilic agonist-antagonist opioid with long duration of action which makes it an excellent choice for postoperative analgesia.7,8 High lipid solubility and high-molecular weight limit rostral spread of buprenorphine reducing the incidence of adverse effects compared to morphine. Different doses of buprenorphine ranging from 30 μg to 150 μg have been used as adjuvant to LA in SAB.9,10,11No ideal dose has been described that can produce postoperative analgesia with minimum side effects. Postoperative analgesia: A similar study was conducted by Dixit, in cesarean section with 60 patients in two groups. In the control group he used 1.7 ml of 0.5% hyperbaric bupivacaine and in the study group he used 1.7ml bupivacaine with 60 μg buprenorphine.12 In the study group he had a mean duration of analgesia of 8.2 h. In the study by Capogna et al., patients who received 45 μg buprenorphine had a mean duration of analgesia of 7.1 h.10 Fifty percent patients had analgesia at 6 h which declined to 16% at 20 h in the study conducted by Ipe et al. using 150 μg buprenorphine.13 Results in the present study are comparable with the above studies. This shows that addition of buprenorphine to intrathecal bupivacaine produces prolonged duration of analgesia which is dose-dependent. This is due to its great affinity for mu receptors and its slow dissociation from the receptors. Patients were evaluated for efficacy of postoperative analgesia by analyzing the maximum pain score attained using VAS during the 24 h period. Maximum pain scores were significantly lower in 0.12mg buprenorphine group compared to 0.06mg Buprenorphine group. Quality of analgesia as assessed by VAS score was significantly better with an increase in dose of buprenorphine. In the study by Dixit, onset of analgesia in the study group was faster than control.12 The peak sensory level of block was comparable among the two groups. Samal et al. reported elevated sensory levels with the addition of 150 μg buprenorphine intrathecally.9 Side Effects: In the study by Ipe et al. in cesarean section, respiratory depression was not observed even with 150 μg intrathecal buprenorphine.13 Being more lipophilic than morphine, rostral spread of intrathecal buprenorphine and therefore the risk of respiratory depression is much less.14,15,16 Addition of 120mcg buprenorphine produced increased incidence of minor side effects when compared to 60mcg . Pruritus, though more likely in obstetric patients receiving neuraxial opioids, was observed only in 2 patients in the study group.13
CONCLUSION The highly lipophilic thebaine derivative opioid partial agonist Buprenorphine is a promising agent in relieving acute post operative pain in caesarean delivery by single shot spinal route with good margin of safety.
REFERENCES
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home