Official Journals By StatPerson Publication
|
Table of Content - Volume 12 Issue 2 -November 2019
Clinical study on effect of Dexmeditomedine on attenuation of haemodynamic response to laryngoscopy and intubation
M Ganesh Moorthy1, N Saranya Devi2*
1,2Assistant Professor, Department of Anaesthesiology, Institute of Social Obstetrics and Government Kasturba Gandhi Hospital for Women and Children, Madras Medical College, Chennai, INDIA. Email: n.saranyadevi@gmail.com
Abstract Background and Aims: The induction of anaesthesia, laryngoscopy, tracheal intubation and surgical stimulation often evoke cardiovascular responses characterised by alteration in systemic arterial blood pressure, heart rate and cardiac rhythm. This study was done to compare the efficacy of intravenous dexmeditomedine with placebo in attenuating the hemodynamic stress responses to laryngoscopy and intubation. Materials and Methods: we conducted a prospective, double-blind randomized controlled study. After Institutional Ethical Committee clearance, sixty patients of American Society of Anesthesiologists Physical Status 1 or 2 undergoing elective surgical procedure under general anaesthesia with endotracheal intubation were enrolled in the study and divided into two equal group. Group D received intravenous dexmeditomedine 0.6 μg/kg (diluted to 20ml) intravenously 10 minutes before induction and Group C received normal saline 20ml intravenously 10 minutes before induction. The general anaesthesia technique was standardised for both groups. Haemodynamic response during laryngoscopy intubation and at 1, 3 and 5 minutes after intubation were measured. Results: Groups were well matched for their demographic data. The data was analysed using SPSS version15.0. There was a statistically significant difference (P<0.05) between dexmedetomidine (0.6 μg/kg) and normal saline in heart rate, systolic, diastolic and mean arterial pressures during and at 1,3,5 minutes after tracheal intubation, stating dexmeditomidine being more effective in attenuating stress response to laryngoscopy and intubation. Conclusion: The haemodynamic changes associated with laryngoscopy and endotracheal intubation can be effectively attenuated by intravenous dexmeditomedine 0.6 µg/kg prior to induction of anaesthesia. Key Words: Dexmedetomidine, Intubation, Laryngoscopy, Haemodynamic response
INTRODUCTION The haemodynamic responses to laryngoscopy and endotracheal intubation have been recognised since 1950. The induction of anaesthesia, laryngoscopy, tracheal intubation and surgical stimulation often evokes cardiovascular responses characterised by alteration in systemic arterial blood pressure, heart rate and cardiac rhythm1. The response following laryngoscopy and intubation peaks at 1.2 minutes and return to baseline within 5 to 10 minutes2. Increase in Blood pressure and heart rate occurs most commonly from reflex sympathetic discharge in response to laryngo tracheal stimulation, which in turn causes increased plasma norepinephrine concentration3. These changes may be fatal in patients with ischemic heart disease and Hypertension. Tachycardia, Hypertension and dysarrythymias all occur during laryngoscopy and intubations. The consequent rise in rate/pressure product may result in myocardial oxygen demand which exceeds the oxygen supply resulting in myocardial ischeamia4. This response is sympathetically mediated and can be attenuated by beta-adrenergic blocking drugs. The haemodynamic changes brought about by laryngoscopy and intubation was first described by Reid and Brace5. Studies have documented myocardial ischemic changes due to reflex sympathoadrenal response immediately following laryngoscopy and intubation with a mean increase in systemic pressure of 40mm of Hg even in normotensive patients. An increase in heart rate is more likely to produce signs of myocardial ischeamia than hypertension on the ECG. Indeed, in anaesthetized patients, the incidence of myocardial ischemia on the ECG sharply increases in patients who experience a heart rate greater than 110 bpm (ischemic threshold). A frequent recommendation is to maintain heart rate and blood pressure within 20% of normal awake value for that patient. Many attempts have been made to attenuate the pressor response to laryngoscopy and intubation in neurosurgical patients. Deep plane of Anaesthesia, Use of ganglionic blockers, intravenous local anaesthetics, nitroglycerine infusion, Magnesium sulphate, Fentanyl, Beta-blockers, Αlpha 2 agonists – Clonidine, Dexmeditomedine6-12. Dexmeditomedine is a newer α2 which has been found to be effective in attenuating the cardiovascular stress response to laryngoscopy and intubation. Our objective is to evaluate the efficacy of Dexmeditomedine by comparing with control (placebo). This study was done in the Department of Anaesthesiology, Govt Kasturba Gandhi Hospital, Madras Medical College, Chennai after getting approval from the hospital ethics
AIM OF THE STUDY For the safe conduct of anaesthesia, the haemodynamic responses to laryngoscopy and intubation should be abolished or at least attenuated to balance the myocardial oxygen supply and demand. This study was done to compare the efficacy of intravenous dexmeditomedine and placebo in attenuating the hemodynamic stress responses to laryngoscopy and intubation.
MATERIALS AND METHODS This prospective, double blinded randomized controlled study was conducted in our medical college hospital after getting approval by our institution ethical committee and after obtaining written, informed consent from the patient. Sixty patients of age 18-50 years assessed under ASA physical status 1 or 2 undergoing elective surgical procedure under general anaesthesia with endotracheal intubation were included in this study. Patients who were having difficult airway, hypertension, diabetes, bronchial asthma, ischemic heart disease, cerebrovascular disease, history of drug or alcohol abuse, history of allergy to clonidine or dexmeditomide were excluded from the study. Patients were divided into two groups of 30 patients each randomly by lots method. The double-blinding procedure was followed, in which the person administering the drug and the patients both were unaware as to which group the patient belonged to. One consultant anaesthesiologist prepared the intravenous (IV) infusions and coded them. The infusions were handed over to the resident anaesthetist to be administered to the patients. The resident anaesthetist was unaware of the contents of the syringe. The resident anaesthetist who administered the infusions recorded the parameters. The patients were unaware as to which group they belonged to. The results of the study were analysed at the end of the study and then the decoding procedure was done. Group C received 20ml of normal saline itravenously 10 minutes before induction and Group D received dexmeditomedine 0.6 mcg/kg diluted to 20ml with normal saline intravenously 10 minutes before induction. Anaesthetic protocol: Pre-operative visit was done to allay anxiety and good rapport was established with the patients. All the patients were given pre-operative night sedation with tab.diazepam 10mg orally. Induction of anasesthesia was standardised for all patients. All patients had NIBP, ECG, Et co2 and pulse oximetry monitoring. Patients are shifted to the operating table,their baseline pulse rate, blood pressure and SpO2 were recorded. They were premedicated with injection glycopyrollate 4 mcg/kg body weight intravenously and injection fentanyl 2mcg/kg body weight intravenously. Then, their heart rate, blood pressure and SpO2 were recorded. The study drug was given intravenously 10 minutes before induction. Then vital signs were recorded. Preoxygenation done with 100% oxygen for 3 minutes .patient was induced with injection thiopentone 2.5% 5mg/kg body weight intravenously and injection succinycholine 1.5mg/kg body weight was given. Intubation was performed by the same person for all the cases with appropriate sized endotracheal tubes orotracheally. Anaesthesia was maintained with controlled ventilation with N2O/O2 mixture 2:1, sevoflurane 1-2% and injection atracurium 0.5mg/kg given as initial dose with top ups with 0.1mg/kg . No surgical stimulation was permitted for 5 minutes after intubation. Haemodynamic variables heart rate, blood pressure noted during intubation, at 1,3,5 minutes after intubation. Patients were monitored throughout the period from entering into operation theatre till recovery and in the immediate post operative period by means of automated NIBP, pulse oximetry and ECG in a multichannel monitor. ECG was monitored with particular importance to any alteration in rhythm. All patients were extubated after neuromuscular reversal with injection neostigmine 0.05mg/kg and injection glycopyrrolate 0.01mg/kg and were shifted to post anaesthetic care unit for a follow up for 24 hours. Descriptive and inferential statistical analyses were carried out using statistical package for social sciences (SPSS) version 15.
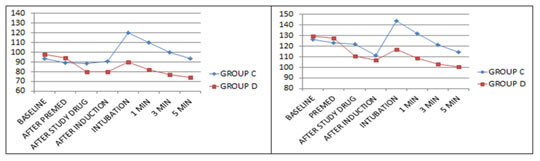
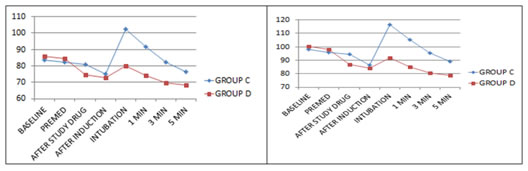
OBSERVATION AND RESULTS Sixty patients under this study were categorised into two groups, group C and group D, 30 in each group. They comprised both sexes in the age group 15-50 yrs. Demographic data of both groups (C and D) were comparable and differences were statistically insignificant. (TABLE: 1) HAEMODYNAMIC VARIABLES The data was analysed using SPSS 15.0 for windows. Haemodynamic variables were represented by mean ± SD. P value of < .05 was considered as statistically significant. The baseline heart rate, systolic, diastolic and mean arterial blood pressure were comparable in both groups. The heart rate, systolic, diastolic and mean arterial blood pressure after premedication, after study drug and induction were also comparatively similar and there is no statistically significant difference among the groups. There is statistically significant difference in haemodynamic response during intubation, at1,3,5 minutes after intubation among the groups. Haemodynamic response were high in group C(normal saline) compared to group D (dexmeditomidine) proven by significant P value <0.001. The statistical data given in tables 2,3,4,5 and charts 1,2,3,4 clearly states that haemodynamic response to laryngoscopy and intubation is effectively attenuated by dexmeditomidine(0.6 µg/kg) when compared to control group. None of the patients had bradycardia, hypotension or fall in saturation in both groups.
Table 1: Demographic variables
Table 2: Comparison of heart rate
Table 3: Comparison of systolic blood pressure (mmHg)
Table 4: Comparison of diastolic blood pressure (mmHg)
Table 5: Comparison of mean arterial pressure(mmHg)
Chart 1: Comparison of Heart Rate Chart 2: Comparison of Systolic blood pressure Chart 3: Comparison of Diastolic bold pressure Chart 4: Comparison of Mean arterial pressure
DISCUSSION Laryngoscopy and endotracheal intubation produces hemodynamic stress responses characterized by hypertension and tachycardia. The haemodynamic response is initiated within seconds of direct laryngoscopy and further increases with the passage of the endotracheal tube. The response is initiated within 5 s of laryngoscopy, peaks in 1–2 min and returns to normal levels by 5 min2. This neuroendocrine response can cause a variety of complications in patients with cardiac disease due to imbalance of myocardial oxygen supply and demand like ischemic changes, ventricular arrythmias and cardiac failure13.This is also hazardous in patients with vascular pathologies due to weakening of lining of major arteries in particular cerebral and aortic aneurysms. In patients with hydrocephalus or intracranial mass lesions the increase in CSF pressure may produce transient impairment of cerebral perfusion leading to cerebral ischemia13. These reflex responses may be diminished or modified locally or centrally and attempts have been made to accomplish this with varying success by different techniques and agents. Many drugs have been reported to have beneficial effects in partially attenuating sympathoadrenal responses to laryngoscopy and endotracheal intubation. Injection lidocaine, esmolol, fentanyl, calcium channel blockers have been extensively studied by many authors6-10. Alpha 2 agonist Dexmeditomedine, though not extensively studied like other drugs, there are many reports stating its beneficial effects in attenuation of circulatory responses to laryngoscopy and endotracheal intubation. α-2 receptor agonists mediate their action through α-2A receptors located in locus caeruleus, the predominant noradrenergic nuclei of upper brainstem. The presynaptic activation of α-2A receptors in the locus caeruleus inhibits the noradrenaline release and brings about sedation and hypnosis. Post-synaptic activation of α-2 receptors in central nervous system brings about decreased sympathetic activity leading to bradycardia and Hypotension14. Dexmedetomidine is more potent α-2receptor agonist than clonidine. The action of dexmedetomidine is short lived with an elimination half-time of 2 h. These factors make dexmedetomidine superior to clonidine15.SCHENIN , LINDGREN et al.,16 ( 1992 ) studied the effect of single dose of intravenous Dexmeditomedine 0.6 µg/kg 10 mins before induction and concluded that Dexmeditomedine attenuated the pressor response to laryngoscopy and intubation . JAAKOLA , ALI – MELKKILA et al.,17 ( 1992 ) studied the effects of single dose of intravenous Dexmeditomedine 0.6µg/kg 10 mins before induction in patients undergoing cataract surgery and concluded that Dexmeditomedine attenuated the pressor response to laryngoscopy and intubation .In our study , comparison of intravenous dexmeditomedine (0.6 µg/kg ) and placebo was done in attenuating circulatory responses to laryngoscopy and endotracheal intubation. HEART RATE CHANGES: The baseline mean heart rate of both the control and dexmeditomedine was not statistaically significant. After laryngoscopy and tracheal intubation there was a increase in heart rate in both the control and study groups . the increase in heart rate in the dexmeditomedine group is significantly less compared to control group during intubation and at 1,3,5minutes after intubation as evident by p value<0.001(table 2). Our study results matches with Jaakola et al17 ., Ferdi Menda et al 18., and Takayuki Kunisawa et al19 ., which proved the efficacy of dexmeditomedine in blunting the haemodynamic response to laryngoscopy and intubation . In our study , the heart rate remained significantly lower in the dexmeditomedine group than the control group at all times after intubation . BLOOD PRESSURE CHANGES: The baseline systolic, diastolic and meanarterial blood pressure in the control group and dexmeditomedine group was not statistically significant(table 3,4,5). After the administration of study drug the systolic ,diastolic and mean arterial blood pressure in the dexmeditomedine group decreased significantly when compared to control group which was statistically significant evident by P value <0.05 (table 3,4,5). After induction , there was no significant difference in the mean systolic,diastolic and mean arterial blood pressure in both the control and dexmeditomedine groups. After laryngoscopy and intubation , there was an increase in systolic ,diastolic and mean arterial blood pressure in both the control and dexmeditomedine groups . The rise in systolic,diastolic and mean arterial blood pressure was less in the dexmeditomedine group when compared with the control group which was statistically significant ( p value < 0.001** )table 3,4,5 . Our study result matches with Scheinin et al16., Ferdi Menta et al18., Jaakola et al17., and Hulya Basar et al20., which proved that dexmeditomedine was effective in attenuating the pressor response to laryngoscopy and intubation . Episodes of perioperative hypertension and tachycardia with its consequent ill effects on the vital organs can be a significant problem in some patients despite adequate depth of anaesthesia and analgesia. This study shows the effectiveness of dexmeditomedine in attenuating the increase in heart rate and blood pressure following laryngoscopy and endotracheal intubation . None of the patients had bradycardia , hypotension or fall in oxygen saturation in both groups. We have not used intra-arterial blood pressure monitoring due to cost constraints and we have not monitored sedation scoring after drug administration.
CONCLUSION Dexmeditomidine at a dose of 0.6 µg/kg intravenous infusion given 10 minutes prior to induction attenuates the haemodynamic response to laryngoscopy and intubation significantly wnen compared to control group. No significant adverse effects noted in patients of both groups.
REFERENCES
|
|
 Home
Home