Official Journals By StatPerson Publication
|
Table of Content - Volume 12 Issue 2 -November 2019
Effects of intrathecal tramadol on low-dose bupivacaine spinal anesthesia in elderly patients undergoing transurethral resection of prostate
N Vijayarahavan1*, P P Mahilamani2, A Thavamani3
1Postgradute, 2Associate Professor, 3Professor and HOD, Department of Anaesthesiology, SreeMookambika Institute of Medical Sciences Email: visinila@gmail.com
Abstract Background: Spinal anaesthesia is preferred over general anaesthesia in TURP. Low-dose Bupivacaine can limit the spinal block level with minimal hemodynamic effects and yield a rapid recovery, but causes inadequate anesthesia for TURP. Tramadol has antinociceptive action when given intrathecally. Aim of the study: To evaluate the adjuvant effects of Intrathecal Tramadol in elderly patients undergoing transurethral prostate surgery with low-dose bupivacaine spinal anesthesia. Materials and methods: Fifty- patients undergoing transurethral prostate surgery were randomized into two groups receiving either Tramadol 20mg (n=25) or normal saline (n=25) intrathecally with 7 mg of 0.5% hyperbaric bupivacaine. The characteristics of the spinal block was evaluated. Results: The Tramadol group demonstrated a longer duration of spinal block than the saline group (p<0.01). The motor block scales at the time of peak sensory block and regression of 2-sensory dermatomes were higher in the Tramadol group (<0.001). There was less analgesic request and the time to the first analgesic request was longer in the Tramadol group (each 487, 345 min, p<0.05). Conclusion: Tramadol 20mg when added to intrathecal bupivacaine 7 mg produced a prolonged duration of sensory block and postoperative analgesia in elderly patients for transurethral resection of prostate Key words; Spinal anaesthesia, Bupivacaine, Tramadol, TURP.
INTRODUCTION Subarachinoid block is considered to be the ideal kind of anaesthesia for Transurethral Resection of Prostate commonly called TURP. The subjects that are taken for TURP are elderly and may have number of systemic diseases. An anaesthetist can be able to review the conscious level and identify early symptoms of prostatic capsular perforation, TURP syndrome and bladder injury under spinal anaesthesia. One of the major issue of Subarachinoid block is hypotension.The extent of block should be controlled for minimizing hypotension in these patients during spinal anaesthesia. Bupivacaine in relatively lower doses can reduce the spinal block level and improve recovery from spinal anaesthesia at a faster rate1.For improving the quality of anaesthesia,prolong duration of SAB and post operative analgesia along with local anaesthetics adjuvant are also added. The addition of opioids in Spinal anaesthesia is well established to prolong the time of post-operative analgesic effect2. Due to the risk of respiratory depression by Opioids, the non-opiate analgesia had been in raise. An analgesic agent called Tramadol that acts on the µ recptors of the Central Nervous system with 6000 folds less affinity for the µreceptor in comparison to morphine3,4. Tramadol blocks the noradrenaline, serotonin and 5-hydroxytreptamine reuptake at the spinal cord level potentiating analgesic effect and prolong the analgesic effects of the Bupivacaine5,6. Unlike an opioid analgesic, Tramadol has a very less effect as a respiratory depressant. As a result, Tramadol can be used for without running the risk of respiratory depression after intrathecal administration. AIMS AND OBJECTIVES To evaluate the impact of spinal administration of bupivacaine with tramadol during post operative analgesia in elderly patients undergoing TURP.
MATERIALS and METHODS After approval of the study protocol by our institutional committee, ASA status I to III patients, aged between 55-75 years, planned for TURP Spinal anaesthesia were inducted in the study. A visit before the operation that was carried out one day before the surgery explained in a very detailed manner about anaesthesia and a consent in the written form was obtained from the patients.The patients were advised nil oral for 6hrs prior to the surgery. Patients with a history of alcoholism or substance abuse, psychiatricillness, spine deformities or any contraindication to Spinal anaesthesia (for eg: coagulation defects, infection at the puncture site, pre-existing neurological deficits , etc.) and subjects who demonstrated an allergic response amide type of local anaesthetics were removed from the study. At operation theatre, following 18-G venous cannula inserted and 500mL of Ringer Lactate was preloaded to the patient before Spinal anaesthesia. Standard monitors like ECG, Non-invasive Blood Pressure, Pulseoximetry and Temperature probe were attached and baseline parameters readings recorded. Inj. Ranitidine 50m.g i.v and Inj. Metoclopramide 10m.g slow i.v given half an hour prior to surgery Fifty patients undergoing TURP surgery were included in this study. Random number sequence was used to admit the patients in one among the two groups: Group T receiving 20mg of Tramadol (Supridol® 50 mg/mL,(Preservarive free) Neon Laboratories ltd.,India.) combined with 7 mg of 0.5% hyperbaric bupivacaine (Anawin® Spinal Heavy; Neon Laboratories ltd.,India) and Group S receiving the same amount(0.4 ml) of normal saline and bupivacaine. 1.4 ml . The total volume of drug solutions was 1.8 ml of 0.4% bupivacaine.SAB was carried out at L3-4 or L4-5 with a midline or paramedian approach. A 25?GQuincke needle in the lateral decubitus position was used.After confirmation of free flow of clear cerebrospinal fluid, the 1.8 ml drug was administered and the patients were then placed in the supine neutral position. The extent of block was assessed on the mid-thoracic line on either sides with a pin-prick every couple of minutes from the block. The peak level of block was identified as the level of block that was the same for four different testing pricks that were consecutive in nature. The VAS score was taken down every half an hour for 6 hours in the postoperative period. In addition, the time of occurence of VAS score 40 mm or when the patient requested rescue analgesic in the nature of intramuscular Paracetamol or Fentanyl was taken down. The time span of analegesia in Group S and T was gathered from the time interval between the time of administration of spinal drug to the time of rescue analgesic with Fentanyl or Paracetamol administered on demand or when the VAS score was was = 40 mm. Sedation scale was observed and recorded for every two minutes for the intial 20 minutes of block, followed by every 10 minutes, till the procedure ended. The sedation scale was given as follows deeply sedated and not arousable = 3, deep sedation but arousable = 2, asleep but easily arousable = 1, fully awake = 0. Hypotension (the fall in mean blood pressure greater than 20% of the basal level or limited than 60 mm of Hg) followed by SAB was treated by bolus intravenous crystalloid therapy and/or 3-6 mg of intravenous bolus dose of ephedrine hydrochloride as and when required. Bradycardia, a condition in which the heart rate is less that 60 b.p.m was treated with atropine 0.6 mg Intravenously. The collected parametric data was analyzed by Student's t test and nonparametric data by Chi-square test, by a statistician of the institution and the results were considered to be significant if (P < 0.05).
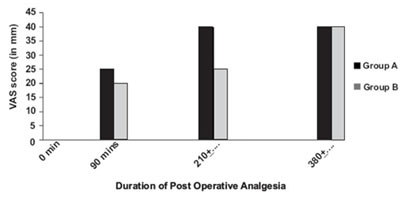
RESULTS The data of two groups - Group S and Group T - were comparable with in age, height, weight and duration of surgery [Table 1]. The duration of analgesia or pain free period in Group S was 208± 10.12 min, comparing to duration in Group T, it was 384 ± 11.82 min, as shown in Table 2. No big variations in the heart rate were observed. In addition, changes were not observed in the average blood pressure, sedation scale, and rate of respiration in either of the groups during the postoperative and intraoperative period [Table 3]. In Group A, a higher VAS score was noticed (= 4) while in Group B a significantly lower VAS score was observed (< 4). The observations were made after 6 hour of the spinal anesthesia. [Figure 1]. No patient on either group had complications like itching, nausea andvomiting, respiratory depression and weakness of lower half of the body in the post operative period
Table 1: Demographic profile of the two groups
Table 2: Comparison of duration of analgesia between Group S and Group T patients
Table 3: Hemodynamic changes and other side effects among two groups in the intra operative period
Figure 1: Comparison of VAS score between the two groups DISCUSSION TURP surgeries are carried out in older patients with a number of related co-morbidities. It is critical that the block level is limited for reducing the hemodynamic instability during spinal anesthesia. The prostate is endowed by sensory branches from the nerves of the pelvic plexus. So a very low spinal block may produce effective analgesia for TURP, but a higher level of block that extens to sensory level of T12–L1 to prevent the pain or discomfort due to the distention of the urinary bladder with fluid for irrigation Although there are several factors influencing the spinal block level, the block level could be more influenced by total dosage of drug, not volume, concentration, or block position. Therefore, intrathecla local anesthetic dosage should be minimized to confine the block level. The majority of anesthesiologists feel that decreased doses of Bupivacaine yield insufficient analgesia. Thus, trials have been done to reduce the dose of intrathecal local anesthetics and increase duration of post operative analgesia with co-administration of additives such as opioids or Tramadol. The use of intrathecal narcotics has become widespread all over the world at the cost of an increased risk for respiratory depression. On the contrary, Tramadol is an analgesic that has less respiratory depressant effects and acts centrally. In addition, it has a decreased affinity for µ receptors in comparison to morphine. The range of dosage for intrathecal tramadol for postoperative analgesia has not been assessed comprehensively till now.11 Therefore, our study was performed to demonstrate that intrathecal administration of 20 mg of tramadol when used with 0.5% bupivacaine extended postoperative analgesia in older patients going through TURP without generating any reactions like nauseaand vomiting, itching and respiratory depression. CONCLUSION To conclude our study showed that 20 mg of Tramadol added to 7 mg of bupivacaine produced a long duration of sensory block as well as a prolonged postoperative analgesia in Elderly patients undergoing TURP compared to bupivacaine alone.
REFERENCES
|
|
 Home
Home