Official Journals By StatPerson Publication
|
Table of Content - Volume 12 Issue 2 -November 2019
Priming by atracurium and its effects on intubating conditions
Khyati R Vaghela1*, Ashutosh M Vyas2*, Jigisha P Badheka3, Vandana S Parmar4, Sanjay Sadadiya5
1Assistant Professor, 2,3Associate Professor, 4Professor and HOD, 5Senior Resident, Department of Anaesthesiology, P.D.U. Medical College, Rajkot , pin code 360001,INDIA. Email: khyati210@gmail.com
Abstract Background: Use of succinylcholine for endotracheal intubating is associated with several side effects. Non depolarizing muscle relaxants are used for intubation whenever succinylcholine is contraindicated, but has delayed onset of action. ‘Priming principle’ is the method used to reduce the delayed onset and improve the intubating conditions of non depolarisers. We evaluated priming by atracurium and its effects on intubating condition. Method: Eighty patients of either gender, aged 15-65 years, American Society of Anaesthesiologist physical status I–III scheduled for elective surgical procedures under general anaesthesia required intubation. The patients were randomly allocated into two groups of 40 patients each. Patients received priming with inj. Atracurium 0.1 mg/kg iv, induction with inj. thiopentone sodium 7mg/kg iv and intubating dose of inj. atracurium 0.6 mg/kg iv after 3 min of priming and intubation was done at 90 seconds in group A and120 second in group B. Patients were observed for intubating conditions during intubation, after intubation and any adverse effects. Results: 9 patients (22.5%) had excellent intubating condition and 31(72.5%) patients had good intubating condition in group A. 31 patients(72.5%) had excellent intubating condition, while 9 patients (22.5%) had good intubating condition in group B. No any patients had fair or poor intubating condition in both the groups. Mean total score were statistically highly significant in both the groups. (<0.0001).No any complication was noted. Conclusion: We concluded that priming method can be used to facilitate rapid endotracheal intubation when use of suxamethonium is contraindicated or undesirable. There were excellent intubating conditions (hemodynamic stability, good jaw relaxation, open vocal cords and rarely coughing/straining or muscular movements during intubation and laryngoscopy) at 120 seconds with inj.atracurium 0.6 mg iv and good intubating conditions at 90 seconds with inj. atracurium 0.6 mg iv after priming of 0.1 mg of inj. Atracurium. Key words: atracurium, intubating condition, priming,
INTRODUCTION Atracurium is benzyl-isoquinoliniumdiester, non-depolarizingneuromuscular blocking agent of intermediate duration of action and slower onset around 2 minutes and produce adequate relaxation required for intubation after 3 minutes.1,2 Although Suxamethonium is preferred over atracurium for endotracheal intubation as due to faster onset with profound muscle relaxant.3 but due to various side effects like hyperkalaemia, arrthymias, intracranial and intraocular pressures, postoperative myalgias, rarely malignant hyperthermia.3, 4 So, when it’s use is undesirable or contraindicated like in motor neuron disease, muscular dystrophies, severe burns , malignant hyperthermia , old CVA with residual pares etc, endotracheal intubation can be achieved if large dose of non-depolarizing muscle relaxant is given. However, such larger doses of neuromuscular blocking drugs may cause side effects and prolonged neuromuscularblockade5. The priming principle6is based on the administration of a small (subparalysing) dose of non-depolarizing neuromuscular blocking drug a few minutes before the intubating dose causes 70-75% occupancy of cholinergic receptors without any significant effect on neuromuscular activity followed by second larger dose after priming dose rapidly increases receptor occupancy to over 90%, suitable for endotracheal intubation. Many studies suggest that the priming dose should be 15-20% of intubating dose and priming interval time to be 2-4 minutes. So, we decided to study effects of inj.atracurium as priming agent (0.1 mg ) and ideal time to achieve intubation, effect on intubating conditions after intubating dose of inj. atracurium (0.6 mg ) and observe adverse effects if any.
MATERIAL AND METHODS After obtaining approval of the institutional ethical committee and written informed consent, this prospective, randomized, comparative study was carried out in our hospital. 80 patients of aged15-65 years, either gender, American Society of Anaesthesiologist physical status (ASAPS) Grade I to III, scheduled for elective surgical procedures under general anaesthesia required intubation were included in study. Patients with history of allergy drug reactions, congenital heart disease, any anticipated airway difficulties, neuromuscular diseases and on drugs known to interact with neuromuscular relaxant drugs were excluded from study. All the patients were randomly allocated into two groups by computer generated random sequence in 40 patients each Group A : priming with 0.1 mg/kg and intubation at 90 seconds after intubating dose of 0.6 mg/kg Group B : priming with 0.1 mg/kg and intubation at 120 seconds after intubating dose of 0.6 mg/kg All patients,Inj. Dextose normal saline was started in iv line after confirming nil by mouth status for 8 hrs and pre-medicated with Inj. Glycopyrrolate 4mcg/kg iv, Inj. Ranitidine 1 mg/kgiv , Inj. Ondansetron 0.08 mg/kg iv, Inj. DiclofenacSodium1.5 mg/kg iv, All the patients were pre-oxygenated with 100% O2 for 3 minutes. Priming was done with Inj.Atracurium 0.1 mg/kg in both groups. General anesthesia was given in both groups with Inj. Thiopentone Sodium 7 mg/kg, 3 minutes after administration of priming dose. The patients in group A and B received Inj. Atracurium 0.6 mg/kg as an intubating dose. Train of four (TOF) twitch count and strength were recorded at 90 seconds after intubating dose in groups A and after 120 seconds in group B. i.e. just before intubation. Intubating conditions were assessed with following parameters and noted during intubation, just after intubation and were noted with the scoring system as shown in table 1.
Table 1
The intubating conditions were noted depending upon the total scores and consider condition as Excellent (score10-12), Good (score7-9), Fair (score4-6), Poor (score0-3). Anesthesia was maintained by intermittent positive pressure ventilation with N2O:O2 (2:1), isoflaurane, intermittent Inj.atracurium were given when required. Pulse rate, automated non-invasive blood pressure, oxygen saturation and ECG were monitored . Neuromuscular blockade was assessed by train of four (TOF) responses using Fisher and Paykel Healthcare (Innervator 272) peripheral nerve stimulator by stimulating the ulnar nerve at wrist and observing number of twitches and strength of contraction of adductor pollicismuscle. STATASTICAL ANALYSIS Collected data were tabulated and analysed by using graph pad prism online calculator. The mean values with standard deviation were calculated for all the parameters and comparison between the two groups was made using unpaired student’s t-test. For qualitative variable data, chi square was applied. The difference between the two groups was said to be statistically significant if p is < 0.05, statistically highly significant if p is < 0.0001.
OBSERVATION AND RESULTS In our study, Demographic profile were comparable in both the groups (p >0.05) regarding age, sex, weight and ASA physical status among both the groups. We conducted this study in general surgeries, Ear nose throat surgeries and orthopaedic surgeries in which endotracheal intubation was required which was comparable in both the groups (p >0.05). Jaw relaxation : In group A, 24 (60 %) patients had good relaxation and 16 ( 40 %) had moderate jaw relaxation, whereas In group B, 39 (97.5 %) patients had good relaxation and only 1 (2.5 %) patient had moderate jaw relaxation. None patients had poor jaw relaxation from both groups. Position of vocal cords: This was assessed as 3 grades : open ( fully relaxed ), semi closed ( partially relaxed ) and closed. In groups A, 33 (82.5%) patients had open vocal cords, 7 (17.5%) semi closed. In group B, 38 (95%) had open, 2 (5%) semi closed had semi closed vocal cord. No patient had closed vocal cord from both groups. Coughing/straining response to intubation: In groups A, 38 (95%) patients whereas in group B, 39 (97.5%) patients had nil incidence of coughing/straining. In groups A, 2 (5%) patient and in group B, 1 (2.5%) patient had had moderate incidence. None patient from both groups had severe incidence of coughing/straining in response to intubation. Muscular movement during intubation: In group A, 39 (97.5%) patients and in group B 39(97.5%) patients had no muscular movement during intubation. Only one patient (2.5%) from both groups had mild movement while none patient from both groups had severe muscular movement during intubation.
Table 2: Neuromuscular junction blockage ( at the time of intubation )
Table 3: Mean total score in both groups
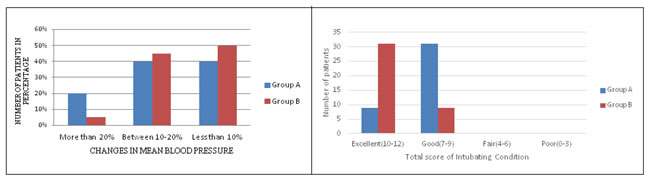
Figure 1: Change in mean blood pressure before and after intubation Figure 2: Total score of observed parameters Figure 1 shows that Change in mean blood pressure before and after intubation were comparable in both groups (p >0.05). Figure 2 showed that 22.5 % patients in group A and 72.5 % patients in group had excellent intubation condition whereas 77.5 % patients in group A and 22.5 % patients in group had good intubation condition . No patient had fair or poor intubating condition from both groups. No any patient had complained of diplopia, difficulty in swallowing or fall in Oxygen saturation in our study. DISCUSSION Priming has shown to accelerate the onset of block , so intubation can be performed within 90-120 seconds after the intubating dose. Priming dose occupies 70-75% of post synaptic nicotinic receptors and when intubating dose is given after 3 minutes of priming dose, it blocks more rapidly the remaining receptors necessary for intubation may be due to priming dose blocks pre-synaptic nicotinic receptors, reducing release of acetylcholine so that the intubating dose produces paralysis more rapidly7.The disadvantage of priming dose to an awake patient is a subjective feeling of discomfort8. Some patients are very sensitive to priming dose can develop profound paralysis (such patients where excluded from study ). Other problem is priming dose of up to 20% of total dose may develop muscle weakness, loss of airway control prior to the induction agent, so we used smaller priming dose 16.67% of total dose. Some studies suggest that 2-3 times the ED95 of a non- depolarizing agent (slightly more) may be used for intubation when priming principle is utilized9.Thus, for atracurium comes to 0.46-0.69 mgkg-1 (ED95 of atracurium is 0.23 mgkg-1). We used a slightly higher dose (total dose 0.7 mgkg-1) because trials done with total dose atracurium 0.6 mg/ kg were not satisfactory even at 3 minutes. Mohamed Naguib et al10 compared different time interval between priming dose and the intubating dose of atracurium and concluded that when priming dose of atracurium is give 3 min before the intubating dose provides an alternative to succinylcholine for rapid endotracheal intubation. So, in our study we kept the priming interval of 3 minutes. Glass P et al11 determined the priming dose of vecuronium, pancuronium and atracurim that resulted in the most rapid onset of neuromuscular blockade. The demographic profile of our study was comparable between two groups , which was similar to other studies in which age, sex and ASA physical status of surgery were comparable in both group similar to results of Hemlata Jaradi et al study12. In our study, we found thatno patients had poor jaw relaxation and closed vocal cords in both groups. Patients had good jaw relaxation and open vocal cords when intubation was done at 120 seconds after intubating dose as compared to 90 seconds after intubating dose. This observation was comparable with study of Dr. L. D. Mishra et al 13. HemlataJaradi et al12 observed the same results when intubating dose of atracurium was given 3 minutes after priming dose as compared to the group in which no priming dose of atracurium was given. So, we can say that atracurium produce adequate intubating conditions after 120 sec with priming method . In our study,mild coughing was found in only 2 patients in group A and 1 patient in group B, rest patients had no coughing in response to direct laryngoscopy which was similar to observation by Dr. L. D. Mishra et al 13and Hemlata Jaradi et al12. Scheller et al and Minogue et al14 observed that direct laryngoscopy and intubation were associated with coughing/straining and abnormal muscular movements if muscle relaxation and depth of anesthesia were inadequate. In our study, 78 patients had no any muscular movements, only 2 patients had mild muscular movements in response to direct laryngoscopy and intubation in both groups. These results are comparable with studies of Hemlata Jaradi et al 12, Dr. L. D. Mishra et al13, Mohamed Naguib et al 10. In our study, we observed that there was slight increase in mean blood pressure in both groups after intubation, increase in mean blood pressure was more when intubation was done 90 seconds as compared to 120 seconds after intubation. Kwong Fah Koh et al compared the intubating conditions after succinylcholine and after atracurium (0.5-0.75 mg/kg) and concluded that Atracurium increases heart rate and blood pressure associated with laryngoscopy and intubation but less changes compare to succinylcholine. Mohammad-Hadi Safaee et al15 observed hemodynamic changes in patients after direct laryngoscopy and intubation. In our study, 39 patients (97.5%) had 3 twitches with reduced strength (75% blockage) and 1 patient (2.5%) had 2 twitches with reduced strength (80% blockage) at the time of intubation in a group where intubation was done at 90 seconds after intubating dose. 18 patients (45%) had 3 twitches with reduced strength (75% blockage) and 22 patients (55%) had 2 twitches with reduced strength (80% blockage) at the time of intubation in a group where intubation was done at 120 seconds after intubating dose. So, there were adequate intubating conditions in both the groups in our study. Mohamed Naguib et al10 observed that all the patients with priming dose of atracurium was given 3 minutes before intubating dose had around 78% neuromuscular blockage at the time of complete twitch suppression of muscle on train of four at the time of intubation after intubating dose of atracurium. In our study, no patient complained of diplopia, difficulty in swallowing, fall in oxygen saturation after receiving a priming dose of 0.1 mg / kg.
CONCLUSION We have observed that by using priming principle (0.1 mg/kg, inj. Atracurium ), there were excellent intubating conditions at 120 seconds and good intubating conditions at 90 seconds after intubating dose ( 0.1 mg/kg , inj. Atracurium ), without any side effects. Thus, this priming method may be used to facilitate rapid endotracheal intubation when use of suxamethonium is contraindicated or undesirable.
REFERENCES
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home