Official Journals By StatPerson Publication
|
Table of Content - Volume 12 Issue 2 -November 2019
Comparison of the performance of LMA proseal versus I-GEL under dexmedetomidine sedation
G Amarappa1, Vishwanath2*, Lohit3, Balaraju TC4, Amitha MN5
1Associate Professor, 2,3Assistant Professor, 4Professor and HOD, 5Postgraduate, Department of Anaesthesiology and Critical care, Navodaya Medical College, Hospital and Research Centre, Raichur, Karnataka, INDIA. Pincode-584101
Abstract Background: Airway management during general anaesthesia is at most important step as it involves haemodynamic changes secondary to sympathetic system stimulation, which is more profound with laryngoscopy and endotracheal intubation compared to supraglottic airway devices (SAD). Among all SADs laryngeal mask airways (LMA) are very widely popular in management of general anaesthesia. Dexmedetomidine combination provides better conditions for insertion of LMAs. In this study we compared the performance of LMA proseal versus I-gel under dexmedetomidine sedation. Aim: To compare the performance of LMA proseal versus I-gel under dexmedetomidine sedation in terms of ease of insertion, number of attempts of insertion, time taken for insertion, haemodynamic changes and complications. Materials and Methods: Sixty patients of ASA 1 and 2 scheduled for elective surgeries under general anaesthesia were randomized into two groups of 30 each. LMA proseal and I-gel were used in group-P and group-I respectively. Both the devices were compared in terms of ease of insertion assessed using Modified Lund and Stovener criteria, jaw relaxation using Young’s criteria, number of attempts for insertion, time taken for insertion, hemodynamic changes and complications. Results: The ease of insertion was easy in 93% of cases in I-gel group, whereas it was easy in 83.3% cases in LMA proseal group. This is statistically significant with p value of ˂ 0.05. Similarly 25 patients of group I had better jaw relaxation compared to 22 patients of group P, which is statistically significant with p value 0.04. 28 insertions in group I were in the first attempt and only 2 patient required 2nd attempt. 25 patients in the group P required only one attempt and 5 patients required 2nd attempt. The attempt of insertion was statistically significant between the two groups (p<0.05). The mean duration of insertion of I-gel and proseal were 15.90±2.52 and 17.80 ±1.69 seconds respectively, which was statistically significant (p<0.05). Heart rate and blood pressure changes were statistically significant within and between two groups. 5 patients in both the group had post extubation cough, and 2 patients in group I and 8 patients in group P had blood tinged LMA after removal. Conclusion: I-gel has better insertion conditions compared to LMA Proseal in terms of ease of insertion, jaw relaxation, number of attempts for insertion, time taken for insertion, hemodynamic changes, and complications. Key Words: laryngeal mask airway, proseal LMA, I-gel.
INTRODUCTION Airway management during general anaesthesia is at most important step as it involves haemodynamic changes secondary to sympathetic system stimulation, which is more profound with laryngoscopy and endotracheal intubation compared to supraglottic airway devices (SAD).1 Apart from haemodynamic changes, trauma to the airway is also a significant problem with endotracheal intubation.2 Among all SADs laryngeal mask airways (LMA) are very widely popular in management of general anaesthesia.3 LMA secures airway but with some limitations such as it does not prevent acid aspiration.4 Proseal LMA, because of its drain tube and dorsal cuff, it prevents aspiration.5 I-gel is a non-cuffed devise but has drain tube and hence it also prevents aspiration.6 Dexmedetomidine with propofol provided good LMA insertion conditions.7 In this study performance of LMA proseal is compared with I-gel under dexmedetomidine sedation.
MATERIALS AND METHODS A prospective randomized study was conducted in our institute during december 2016- august 2018 on the topic “Comparison of ease of insertion of laryngeal mask airway proseal and i-gel under dexmedetomidine- sedation”. The study was undertaken after obtaining ethical committee clearance and informed written consent from all patients. Sample size calculation was done using open epi software and the formula N = 2(Zα+Zβ)2σ2/Δ2. At 95% of confidence level, 5% of α error, Zα=1.96 At 80% of power Zβ=0.84. The sample size calculated is 30 in each group. Allocation into two groups was be done by computer generated randomization table. Sixty patients aged 18-60 years, scheduled for various elective surgical procedures undergoing general anaesthesia belonging to ASA (American society of anaesthesiologists) class I and II were included in the study. Patients with cardiorespiratory illness and those prone for gastric aspiration were excluded. LMA proseal and I-gel were used in group-P and group-I respectively. After preanaesthetic evaluvation all patients were kept nil per mouth as per standard guidelines. In pre-anaesthetic area for all patients 20G IV cannula was secured and injection metoclopramide 10 mg iv and injection ranitidine 50 mg iv were given 30 min prior to anaesthesia induction. After shifting to OR, baseline parameters recorded. Dexmedetomidine 1 mcg/kg in 100 ml normal saline was given over 10 minutes. Patients were preoxygenated for 3 minutes, and premedicated with injection glycopyrolate 0.004 mg/kg iv, injection midazolam 0.03mg/kg iv, injection fentanyl 2µg/kg iv. Patient were induced with injection propofol 2 mg/kg iv. If required, further increment of propofol 0.5mg/kg will be given every 30sec until the loss of consciousness and loss of eyelash reflex. After adequate depth of anesthesia was achieved, the device of appropriate size was inserted after lubrication with water based jelly by the anaesthesiologist experienced in both device insertions. LMA proseal and I-gel were used in group-P and group-I respectively. Insertion is attempted to a maximum of 3 attempts. However the conditions during laryngeal mask airway insertion are only graded at first attempt. Correct position of the device was confirmed by bilateral symmetrical chest movements on manual ventilation, no audible leak of gas and lack of gastric insufflations. Both the devices were fixed by taping the tube to the chin and well lubricated gastric tube was introduced in to the stomach. Patients were kept on spontaneous ventilation with Bain’s circuit. Anaesthesia maintained with 0.7% halothane, 66% N2O, 33% O2. At the completion of surgery halothane, N2O stopped and LMA removed. Oxygen given by face mask till recovery. The patient is monitored with ECG, pulse oximeter and NIBP throughout procedure. Ease of insertion was measured based on Modified Scheme of Lund and Stovener (Table 1),7 and jaw relaxation based on Young’s criteria (Table 2).7 Number of attempts for insertion and time taken for insertion were noted. Postoperatively patients were observed for complications such as presence of blood on the device, trauma to the airway and laryngo-bronchospasm. Table 1: Modified scheme of Lund and Stovener for grading conditions during LMA insertion
Table 2: Young’s criteria for jaw relaxation
RESULTS AND STATISTICAL ANALYSIS Statistical analysis was done using SPSS software 16.0. Data obtained is tabulated in the Excel sheet analysed. Mean ± standard deviation is calculated. Chi-square test for proportions in qualitative data. Student’s unpaired t – test for Quantitative data. P< 0.05 was considered statistically significant. Demographics and other characteristics of the patients of either group are comparable (Table 3).
Table 3: Comparison of demographics and other characteristics
The ease of insertion of I-GEL was easy in 25 patients compared to that of proseal which was easy to insert in 20 patients. This is statistically significant with p value of 0.03. (Table 4).
Table 4: Comparison of conditions of LMA insertion
Similarly 25 patients of group I had better jaw relaxation compared to 22 patients of group P, which is statistically significant with p value 0.04 (Table 5).
Table 5: Comparison of jaw relaxation
Table 6 shows 28 insertions in group I were in the first attempt and only 2 patient required 2nd attempt. 25 patients in the group P required only one attempt and 5 patients required 2nd attempt. The attempt of insertion was statistically significant between the two groups (p<0.05).
Table 6: showing number of attempts taken to insert device in each group
Table 7 shows the mean duration of insertion of I-gel and proseal in patients were 15.90±2.52 and 17.80 ±1.69 seconds respectively and was statistically significant (p<0.05).
Table 7: Time duration of insertion
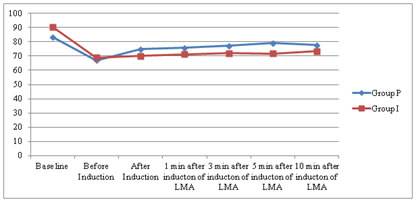
Table 8 and graph 1 show that the heart rate changes between the two groups and within the groups were significant after induction. Table 8: Hear rate changes within the group and between groups
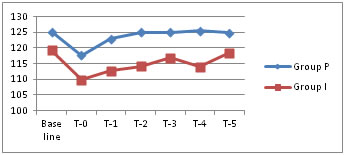
Graph 1: Hear rate changes within the group and between groups Table 9 and graph 2 show SBP changes between the group I and group P which were significant. Table 9: SBP changes within the group and between groups
Graph 2: SBP changes within the group and between groups
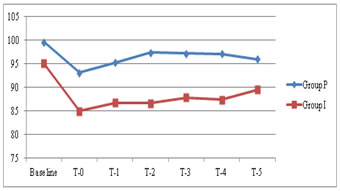
Table 10 and graph 3 show MAP changes between the two groups were statistically significant. Table 10: MBP changes within the group and between groups
Graph 3: MBP changes within the group and between groups Table 11 shows 5 patients in both the group had post extubation cough, and 2 patients in group I and 8 patients in group P had blood tinged LMA after removal. Table 11: Device related complications
DISSCUSSION Securing airway during general anaesthesia with endotracheal tube involves sympathetic stimulation and haemodynamic instability, and possible trauma to the airway. [1,2] Supraglottic airway devices are the better alternative to endotracheal tubes as they avoid complications of endotracheal intubation.[3] Proseal LMA forms better seal surrounding glottis opening because of dorsal cuff and prevents aspiration because of drain tube.[5] I-gel is a device without any inflatable cuff creating anatomical seal with perilaryngeal structures.[6] Dexmedetomidine provides awake sedation, good haemodynamic stability and postoperative analgesia. Dexmedetomidine with propofol provided good LMA insertion conditions which is in accordance with Nellore SS, et al who found that propofol with dexmedetomidine provides excellent overall insertion conditions and hemodynamic stability.7 In this study performance of LMA proseal is compared with I-gel in patients undergoing elective surgeries under general anaesthesia and dexmedetomidine-propofol sedation. In our study the ease of insertion of I-gel was better than proseal. Our finding is similar to the study conducted by Singh et al which shows ease of insertion for I-gel was better than proseal.[8] This can be explained by the findings of the study conducted by Levitan et al who presumed that on insertion of LMA with inflatable mask, the deflated leading edge of the mask can catch the edge of the epiglottis and cause it to downfold or impede proper placement of the tongue. 9 It is also supported by Brimacombe et al who presumed that difficulty in inserting the LMA-Proseal was caused by larger cuff impeding digital intraoral positioning and propulsion into the pharynx. 10 In our study the number of attempts of insertion of I-gel was less compared to proseal. This is supported by Chauhan et al who observed that the number of manipulations required were more with proseal compared to I-gel and it resulted in corresponding hemodynamic changes. 11 In our study the mean duration of insertion of I-gel was significantly less compared to that of proseal. It is suppored by the study conducted by Gattward et al which shows the duration of insertion was less for I-gel.12 Our study finds that I-gel had 6% of cases with blood staining on the device after removal whereas proseal had 26.7% of cases, which is statistically significant with p value of ˂ 0.05. This can be explained by the findings of Singh et al who reported that the incidence of trauma to the tongue, lip and teeth was observed in 16.7% patients with proseal compared to 3.3% patients with i-gel.[8] It is supported by Levitan et al who presumed that inflatable masks have the potential to cause distortion, venous compression and nerve injury.9 Our study finds that both the study groups had equal incidence of post extubation cough. Other complications like bronchospasm, laryngospasm, vomiting and hoarseness of voice did not occur in two groups. Our study finds that use of dexmedetomidine before induction had significant effect on hemodyamic changes in both proseal and I-gel groups but I gel group had better haemodynamic parameters than proseal. This is in accordance with Uzumugil F et al who compared dexmedetomidine-propofol and fentanyl-propofol for insertion of LMA. They concluded that former combination provides more successful LMA insertion comparable to fentanyl, while preserving respiratory functions.13 Our study had some of the limitations. Insertions were done in patients with normal airway and normotensive patients, therefore present results may not apply to patients with difficult airways and hypertensive patients. There was no blinding in the data collection, which is a possible source of bias.
CONCLUSION Performance of I-gel was compared with Proseal LMA in patients of ASA class I and II coming for elective surgeries under general anaesthesia and dexmedetomidine sedation. I-gel was better in view of ease of insertion, time taken for insertion, attempts of insertion, haemodynamic stability and also less traumatic to airways than proseal. Therefore I-gel performs better than proseal.
REFERENCES
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home