Official Journals By StatPerson Publication
|
Table of Content - Volume 12 Issue 2 -November 2019
Comparison of haemodynamic responses to insertion of i-gel and endotracheal tube: A randomized controlled study in adult patients posted for elective surgery under general anaesthesia
N Gusain1, S Mitra2*, M Agrawal3
1Post Graduate Resident, 2Associate Professor, 3Professor Department of Anaesthesiology, Rohilkhand Medical College and Hospital, Pilibhit Bypass Road, Bareilly (U.P) Pin- 243006, INDIA. Email: subhromitra16@gmail.com
Abstract Aim: The purpose of this study is to compare the effects of i-gel insertion and Endotracheal intubation on heart rate, systolic and diastolic blood pressure and mean arterial blood pressure during elective surgeries under general anaesthesia in paralyzed patients. Material and Methods: Eighty patients of American Society of Anaesthesiology Physical Status I or II undergoing general anaesthesia for General Surgery and ENT surgery procedures were randomly allocated in two groups of 40 patients each. Group E had laryngoscopy and endotracheal intubation done for their airway management and Group I underwent insertion of i- gel TM. Both the groups were compared for haemodynamic parameters at induction of anaesthesia, then immediately after insertion or intubation, and subsequently at 1 minute, 3 minutes and 5 minutes after introduction of i-gel or Endotracheal tube. Observations and Results: The increase in heart rate with i- gel insertion was significantly less than endotracheal intubation till 3 minutes (p<0.0001). The increase in systolic blood pressure on comparison between the two groups immediately after insertion of device, 1 min, 3 min and 5 min after insertion of respective devices, was less with i- gel (p <0.05). The diastolic blood pressure increased more in Group E as compared to Group I (p<0.05) and the rise in the mean arterial blood pressure was also lower in Group I. Conclusion: Both Endotracheal intubation and i- gel insertion produced increase in heart rate, systolic blood pressure, diastolic blood pressure and mean arterial blood pressure, however the increase was less with insertion of i- gel. Hence, i- gel insertion has better haemodynamic stability compared to laryngoscopy and endotracheal intubation. Key Words: Endotracheal tube, i- gel, laryngoscopy, haemodynamic response.
INTRODUCTION Administration and maintenance of general anaesthesia necessitates tracheal intubation in most of the cases but the procedure is not without adverse effects. Induction of general anaesthesia is known to induce clinically relevant changes in hemodynamic variables probably generated by direct laryngoscopy and endotracheal intubation which appear to be attenuated by alternative airway managements. Tracheal intubation causes a reflex increase in sympathetic activity that may result in hypertension and tachycardia. Though in the majority of patients undergoing anaesthesia, these responses are transient and probably of little consequence, they may be harmful to some patients, mainly those with myocardial or cerebrovascular diseases1. The extent of the reaction is affected by many factors: the technique of laryngoscopy and intubation and the use of various devices, like tracheal tube, laryngeal mask airway (LMA) supraglottic airway devices. The laryngeal mask airway (LMA) was designed as an alternative to tracheal intubation to maintain a patent airway during anaesthesia with minimal morbidity. Since the development of the LMA in 1983 by Archie I.J Brain, several other supraglottic devices have been introduced for management of airway, aiming to offer simple and effective alternatives to tracheal intubation2.The i-gel is a relatively new supraglottic device with an anatomically designed mask made of a soft, gel like and transparent thermoplastic elastomer. It has no cuff to inflate, providing easy use and stability after insertion, as well as reducing the possible stimulatory effects of tissue compression3. Different studies have shown that i-gel and classic or proseal LMA can be used safely during positive pressure ventilation with stable hemodynamics and normal oxygenation and ventilation4. We are hypothetizing that there will be less hemodynamic response with i-gel insertion as compared to endotracheal tube intubation and therefore plan to conduct a prospective, randomized study to examine the hemodynamic changes produced by inserting an i-gel or endotracheal tube in consenting healthy normotensive anaesthetized patients after their approval for participating in the study.
MATERIAL AND METHODS Following approval by the Board of Thesis/Research committee, Department of Anaesthesiology, and Ethical committee, RMCH, Bareilly, 80 patients posted for elective surgeries of specialities like general surgery and ENT surgery, belonging to ASA grade I or II of either sex, aged 18-60 yrs, weighing 50-80 kg and Mallampati class I or II were recruited for this study. Patients who refused for procedure, had probability of difficult intubation, Mallampati class>II, emergency surgery, full stomach, obesity (BMI>30kg/m2), cardiovascular diseases and uncontrolled hypertension, high intra cranial pressure (ICP) and patient’s with contraindications for insertion of supraglottic devices were excluded from the study. The patients were randomly divided into two groups: Group “I” and “E” with 40 patients in each group. In Group I, proper sized i-gel was used, while in Group E, endotracheal tube of appropriate size was used to manage the airway of the patient. All patients were kept nil per oral night before surgery and received Tab Ranitidine 150mg and Tab Alprazolam 0.25mg orally in night. On the day of surgery, intravenous drip was started 30 min before surgery and Inj. Glycopyrrolate 0.2mg was given. After shifting the patient to the operating room, monitors were attached and baseline readings were taken. Patients were premedicated with Inj. Ranitidine 50 mg, Inj. Ondansetron 4 mg, Inj Butyrophenol 1mg. Induction was done with propofol 2.5mg kg-1 and succinylcholine 1.5mg kg-1 and heart rate, systolic blood pressure, diastolic blood pressure and mean arterial blood pressure were recorded. Intubation was done with either proper size i-gel supraglottic device or appropriate sized endotracheal tube. Confirmation of ventilation was done by adequate chest rise and auscultation. Patient was connected to ventilator with closed circuit. Heart rate, systolic blood pressure, diastolic blood pressure and mean arterial blood pressure was recorded after induction, then immediately after insertion or intubation, and subsequently at 1 minute, 3 minutes and 5 minutes after introduction of i-gel or Endotracheal tube. These parameters were recorded by an accompanying anaesthetist. In case of laparoscopic surgeries, the parameters were recorded before creation of pneumoperitoneum. Maintenance was done with O2 and N2O in the ratio 40:60 and 1% Isoflurane was started. Bolus dose of vecuronium (0.08- 0.1mg kg-1) was given after intubation. 1mg of vecuronium was given as top up during surgery. Ventilator setting of Tidal Volume and Respiratory Rate was adjusted to keep the EtCO2 30-35mmHg. Respiratory rate was kept between 12 to 14 breaths per min. At the end of the surgery reversal was done with neostigmine 0.05mg kg-1 and glycopyrolate 0.008mg kg-1. After pharyngo-tracheal suction, extubation was done. Ethical Committee Approval: Ethics committee approval was received for this study from the Institutional Ethics Committee (IEC) of Rohilkhand Medical College and Hospital, Pilibhit Bypass Road, Bareilly (U.P.) Pin- 243006. Statistical Analysis: Data was summarized as mean ± standard deviation with confidence interval of 95% or as percentages. Statistical analysis was performed using by SPSS version 26. Numerical variables were normally distributed and compared by unpaired ‘t’ test. Paired t- test was performed for comparing mean percentage of improvement in the groups. A p value less than 0.05 was considered as statistically significant.
RESULTS Table 1: Comparison of sex and age (years) in the two groups
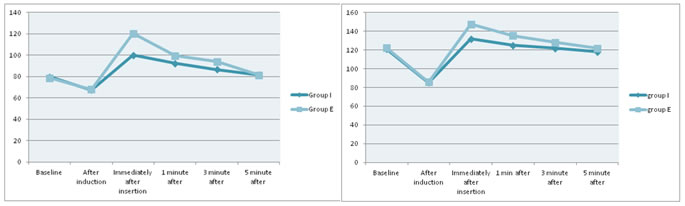
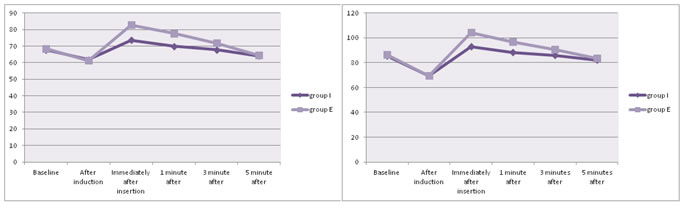
No statistically significant difference between the two groups was seen with respect to age, sex, weight, ASA status and Mallampati class (p>0.05). Figure 1 Figure 2 Figure 3 Figure 4 Figure 1: Comparison of mean heart rate; Figure 2: Comparison of Mean Systolic Blood Pressure; Figure 3: Comparison of Mean Diastolic Blood Pressure; Figure 4: Comparison of Mean Arterial Blood Pressure
Figure 1, In our comparative study, changes in heart rate were seen in both the groups after insertion of i- gel or endotracheal intubation. The mean heart rate remained elevated for up to 3 minutes in both group I and group E. However, the increase in values were statistically significantly lower in group I immediately after insertion, 1 min and 3 min after as compared to group E (p<0.0001). Figure 2, In our comparative study, changes in mean systolic blood pressure were seen in both the groups after i- gel insertion/ endotracheal intubation. The mean systolic blood pressure was statistically highly significant between the two groups immediately after insertion, 1 min and 3 min (p<0.0001) and statistically significant at 5 min (p=0.0029). Figure 3, In our comparative study, changes in mean diastolic blood pressure were seen in both the groups after i- gel insertion or endotracheal intubation. The mean diastolic blood pressure was statistically highly significant between the two groups immediately after insertion and 1 min (p< 0.0001), while it was statistically significant at 3 min (p=0.0002). The mean diastolic blood pressure changes between the two groups became insignificant at 5 min (p=0.6976). Figure 4, In our comparative study, changes in mean arterial blood pressure were seen in both the groups after airway instrumentation. The increase in mean arterial blood pressure was statistically highly significant between the two groups immediately after insertion, 1 min and 3 min after (p< 0.0001), while it became statistically insignificant at 5 min (p=0.079).
DISCUSSION Laryngoscopy and endotracheal intubation has been the most widely accepted safest technique to secure the airway in patients under general anaesthesia. The haemodynamic response during laryngoscopy and endotracheal intubation is the result of oropharyngeal and tracheal stimulation. The possible complications include transient hypertension, tachycardia and arrhythmia. Most patients with normal heart functions may tolerate such changes without serious complications while in patients with altered cardiac reserves, these haemodynamic turbulences may be hazardous5. The i-gel TM supraglottic airway (Intersurgical Ltd, Wokingham, Berkshire, UK) is a novel supraglottic airway device (SAD) which was introduced for clinical practice in 2007 by Dr Muhammed Aslam Nasir. It is made of thermoplastic elastomer which is soft, gel- like and transparent3. The i- gel works in harmony with the patient’s anatomy with minimum compression and displacement trauma. There was no significant difference in the age, sex, weight, ASA grading and Mallampati class between the two groups. Haemodynamic parameters: The cause and effect relationship that the induction agent might have had on the haemodynamic changes can be discounted owing to the use of similar premedication and induction agents and muscle relaxants in both the two groups. In our study we found that there was no significant difference between the two groups at the baseline. However, on insertion of the respective airway device, change in mean heart rate was seen which remained elevated for up to 3 minutes in both Group I and Group E. The increase in values was statistically significantly lower in Group I immediately after insertion, 1 and 3 minutes after insertion as compared to Group E (p less than 0.0001 in all the three time intervals). At 5 minutes after insertion, the increase in heart rate in the two groups was not statistically significant (p=0.4974). This was similar to the studies done by Ismail et al6, Badheka et al7 and Das et al8. In our study, we found that changes in systolic blood pressure in Group I was less than Group E. The systolic blood pressure increased from baseline in both the groups and remained elevated for up to 3 minutes in both Group I and Group E. However, the increase in values was statistically highly significantly lower in Group I immediately after insertion, at minutes 1 and 3 as compared to Group E (p less than 0.0001 in all three intervals) which was in agreement with study conducted by Jindal et al9. In our study, it was seen that the diastolic blood pressure was increased from baseline in both the groups, but the increase was statistically more significant in Group E compared with Group I immediately after insertion, 1 min and 3 min but comparable in both the groups at the 5th min, similar to Jindal et al9 and Atef et al10.In our study, we noted that the increase in MAP from baseline values similar to Dhanda et al11 and Zanfaly et al12.Contrary to our study, Elgebaly et al13 did not document a significant change in haemodynamic parameters between the endotracheal tube and i- gel which could be due to administration of fentanyl. However, they did report a larger requirement of fentanyl in the endotracheal tube group. The transient increase in haemodynamic parameters as seen in our study can be attributed to the increased sympathetic nerve activity resulting in release of catecholamine which have a short half life of 10 seconds to 1.7 minutes and are quickly degraded by catechol-O-methyltransferase or monoamine oxidase14. The lack of mechanical stimulation caused by laryngoscopy and ETT intubation during insertion of i- gel is a major reason for the attenuated haemodynamic responses15. The mechanical stimulation during laryngoscopy is transmitted by the trigeminal, glossopharyngeal and vagus nerves to the vasomotor centre in the brain which stimulates sympathoadrenal axis6. Supraglottic airway devices are generally thought to cause minimal stress responses; however, this might not be true in some supraglottic devices which have large oropharyngeal cuffs. The i- gel is made of gel like thermoplastic elastomer called Styrene Ethylene Butadiene Styrene (SEBS) which is soft and fits snugly onto perilaryngeal framework. It has a noninflatable preshaped cuff that minimally stimulates pharyngeal structures and changes its own shape after placement to fit perfectly with the pharyngeal structures rather than pushing them3. The preshaped cuff also precludes inflation, which might further increase haemodynamic stress.
CONCLUSION The present comparative study concluded that i- gel causes less haemodynamic changes (HR, SBP, DBP, and MAP) in anaesthetized patients compared to laryngoscopy and endotracheal intubation. Hence, we conclude that the i-gel is a suitable and safe alternative to cuffed Endotracheal tube for airway management in elective fasted adult patients undergoing surgeries under general anaesthesia.
REFERENCES
|
|
 Home
Home