Official Journals By StatPerson Publication
|
Table of Content - Volume 12 Issue 3 -December 2019
The effect of acute normovolemic hemodilution on hematocrit and systemic oxygen delivery during cardiopulmonary bypass: A prospective randomized study
Pushpa Jagannath1, Suman S2*, PrasannaSimha M3, Manjunatha N4
1,2Assistant Professor, 4Professor and HOD, Department of Anaesthesia, SJICR, Bengaluru, Karnataka, INDIA. 2Professor, Department of Cardiothoracic and Vascular Surgery, SJICR, Bengaluru, Karnataka, INDIA. Email: drpushpajagannath@gmail.com
Abstract Background: Acute normovolemic hemodilution(ANH) is the removal of whole blood from a patient while restoring the circulating blood volume with an acellular fluid shortly before an anticipated significant surgical blood loss. We studied the effect of ANH in cardiac surgical patients on hematocrit and systemic oxygen delivery during cardiopulmonary bypass. We compared the hematocritvalues and systemic oxygen delivery during cardiopulmonary bypass(CPB) of patients undergoing valvular heart surgeries with and without ANH. Materials and Methods: The study was a prospective randomized trial. Fifty patients who underwent valvular heart surgery from September, 2014 to December, 2014 in Sri Jayadeva Institute of Cardiovascular Sciences and Research, Bengaluru were enrolled in the study. They were randomly allotted to either the ANH group or conventional management group. The hemoglobin values, hematocrit values, mean arterial pressure, systemic oxygen delivery and cardiopulmonary bypass flows during cardiopulmonary bypass were noted and compared between the groups. The data was analyzed using Chi square test and Student’s t –test. Results: The two groups were comparable demographically. The hematocrit in the ANH group was lower as compared to the control group throughout the cardiopulmonary bypass duration, achieving statistical significance at lowest temperature (P value = 0.036). The DO2 values were comparable in both the groups throughout CPB (P value = 0.45,0.71,0.77). It can be attributed to the higher flows in the ANH group during cardiopulmonary bypass. Key Word: ANH, Hematocrit, Systemic oxygen delivery, Valvular heart surgery
INTRODUCTION Patients undergoing cardiopulmonary bypass (CPB) procedures are prone to a variety of hemostatic derangements that necessitate frequent transfusions of allogeneic blood products1. Preventing allogenic blood transfusions during cardiac surgery and in the postoperative period is important as they are associated with worse short and long term outcome. ANH is an effective means of reducing the risk of blood transfusion in these patients2.‘Acute Normovolemic Hemodilution (ANH) is the removal of whole blood from a patient while restoring the circulating blood volume with an acellular fluid shortly before an anticipated significant surgical blood loss’.3 The goal is to reduce the amount of red blood cells loss during the intra-operative and immediate post-operative period, as well as to conserve a certain amount of blood from destructive effects of the CPB1. ANH causes reduction in the hematocrit of the patients and increases the magnitude of hemodilution that occurs with the initiation of CPB4. The degree of hemodilution has been reported to be one of the significant factors affecting cerebral oxygenation during cardiopulmonary bypass5.On the other hand ANH causes reduction in the viscosity of the blood which could improve the microcirculation with resultant improved oxygen delivery6. Thus studying the effects of ANH on hematocrit and whole body and brain oxygen delivery is important. Hemoglobin is a major determinant of whole body oxygen supply7. We studied the effect of ANH on the degree of hemodilution and systemic oxygen delivery during cardiopulmonary bypass. We compared the hematocrit and systemic oxygen delivery(DO2) values during CPB of the patients undergoing valvular surgery with and without pre cardiopulmonary bypass ANH.
MATERIALS AND METHODS The study was a prospective randomized trial. Fifty patients undergoing valvular heart surgeries were included in the study after informed consent. The exclusion criteria were: age less than 18 or more than 65 years, preoperative hematocrit less than 30%, prior history of neurological problems, preoperative severe LV dysfunction, coagulopathies, significant/ symptomatic carotid artery stenosis, emergency surgery or redo surgery. After recruitment they were randomized into two groups. The demographic characteristics were recorded. Standard perioperative anesthetic and surgical protocols were followed.ANH group underwent removal of blood before administration of heparin. Volume of blood to be removed was calculated based on the patient’s weight, the starting hemoglobin value and a target hematocrit of 22% on CPB using the formula Volume to be drawn =
Where Hct CPB is the calculated CPB hematocrit which is calculated using the formula
Standardized CPB techniques were used in both the groups. The CPB circuit was primed with 1000 ml of 0.9% NS and 500 ml of RL. Pump flow was maintained between 2.0 to 2.4 L/min/ m2. The MAP during CPB was maintained between 55 and 70 mm of hg. The patients were cooled to 28 degrees Celsius. Hemoglobin (Hb), Hematocrit, Oxygen saturation (SaO2), Partial pressure of oxygen in arterial blood(PaO2), Lactate values, Mean arterial pressure(MAP) and temperature were noted at various time points – before induction of anesthesia, after induction of anesthesia, before ANH, after ANH, before going on CPB, during initiation of CBP, at lowest temperature on CPB, during rewarming and after administration of protamine. Cardiopulmonary bypass flows were noted at initiation of CPB, lowest temperature and rewarming. Hematocrit values, CPB flows, Mean arterial pressure values and Delivery of Oxygen (DO2) values of both the groups during the described time points were compared. The requirement of intraoperative blood transfusion in both the groups was also compared. Delivery of oxygen was calculated by the formula7 DO2(Delivery of oxygen) = CaO2 x CO Where, CaO2(Oxygen content of blood)= (Hb x 1.39 x SaO2)+ (PaO2 x 0.003) CO =Cardiac Output (Pump Flows during CPB) Hb = Hemoglobin value SaO2 = Oxygen saturation in arterial blood. PaO2 = Partial Pressure of Oxygen in arterial blood. Statistical Analysis: Medcalc (12.12 Version) statistical software was used. Nominal data was compared using Chi Square test. Continuous data was compared using Independent t test and Paired t test. The null hypothesis was that the means of the two groups were the same. If the significance P value was less than or equal to 0.05 the null hypothesis was rejected. RESULTS Demographic characteristics and the details of the procedure performed are compared in table 1 and 2. The mean age of the ANH group was 42.56±13.6 years and control group was 41.12±12.88 years. Both the groups did not differ with respect to age, gender, types of surgeries performed, cardiopulmonary bypass time and cross-clamp time.
Table 1: Demographic Characteristics and CPB and Cross-clamp times in both the groups.
Table 2: Types of surgeries in both the groups.
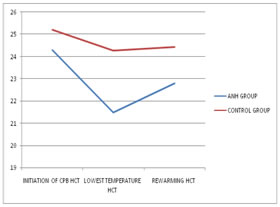
The hematocrit at the initiation of CPB was lower (24.3± 5.0) in the ANH group as compared to the control group(25.2± 5.2)but the difference was not statistically significant( P value=0.57). The hematocrit at the lowest temperature during CPB was lower(21.5±4.7) in the ANH group as compared to the control group(24.3±4.5)and the difference was statistically significant( P value=0.036) . The hematocrit during rewarming in CPB as compared was lower(22.8±4.2) in the ANH group as compared to the control group(24.4±3.5)but the difference was not statistically significant( P value=0.14).The hematocrit was lowest in the ANH group at lowest temperature. We attribute it to increasing hemodilution with time. The hematocrit fell below eighteen in two patients in the ANH group and two patients in the control group. The threshold for transfusion during CPB was kept as hematocrit less than eighteen. Blood was added twice to pump in the ANH group and thrice in the control group.
Table 3: Hematocrit values (In Percentage) in ANH and Control groups.
Figure 4: Line Graph depicting trend of hematocrit values in ANH and Control Groups.
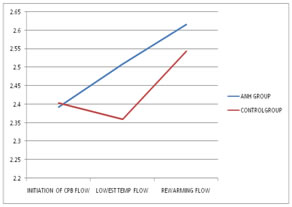
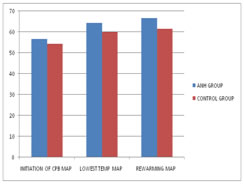
The CPB flows at the initiation of CPB as compared were similar (2.39± 0.23) in the ANH group as compared to the control group (2.4± 0.22) and the difference was not statistically significant (P value = 0.85). The CPB flows at the lowest temperature during CPB was higher (2.51± 0.26) in the ANH group as compared to the control group (2.36± 2.36) and the difference was statistically significant ( P value=0.05) . The CPB flows during rewarming in CPB as compared was higher (2.62 ± 0.18) in the ANH group as compared to the control group (2.54± 0.27) but the difference was not statistically significant ( P value=0.29). Figure 5: Line Graph depicting trend of cardiopulmonary bypass flows in ANH and Control Groups The mean arterial pressure (MAP) at the initiation of CPB was similar in the ANH group as compared to the control group.The mean arterial pressure(MAP) at the initiation of CPB was similar(56.64± 10.1) in the ANH group as compared to the control group(54.44± 10.79)and the difference was not statistically significant(P value = 0.46). The MAP at the lowest temperature during CPB was higher(64.32± 7.74) in the ANH group as compared to the control group(59.88±7.92)and the difference was statistically significant(P value = 0.05). The MAP during rewarming in CPB as compared was higherin the ANH group (66.56±7.48)as compared to the control group(61.52± 7.75)and the difference was statistically significant(P value = 0.02).
Figure 6: Bar Graph comparing MAP values in ANH and Control Groups(Unit = mm of Hg).
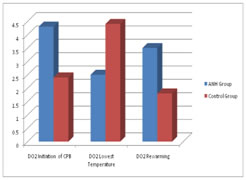
The DO2 values were comparable in both the groups. The difference was not statistically significant at initiation of CPB(P value = 0.45), lowest temperature during CPB (P value = 0.71) and rewarming during CPB(P value = 0.77). Figure 7: Bar Graph comparing DO2 values in ANH and Control Groups
DISCUSSION The hematocrit was lowest in the ANH group at lowest temperaturewhich is probably because of increasing hemodilution with time. Despite the lowered hematocrit, systemic oxygen delivery (DO2) was maintained and comparable with the control group. There was no increase in incidence of acidosis or increased lactate levels in the ANH group as compared to the control group. This might be because the CPB flows were higher in the ANH group as compared to the control group achieving statistical significance at lowest temperature. This might have ensured the higher MAP in the ANH group as compared to the control group which was statistically significant at lowest temperature and rewarming during CPB. During bypass human body undergoes a change in body temperature, a rapid reduction in hematocrit and a loss of pulsatile flow. Assuming a steady state of anesthesia, cerebral metabolic requirement of oxygen varies primarily in inverse relation to brain temperature. However, the cerebral blood flow is also influenced by variables like Cerebral metabolic requirement of oxygen(CMRO2), PaCO2, hematocrit, mean arterial pressure, cardiopulmonary bypass flow and brain perfusion, pulsatility and CPB duration. The effect of variables like brain temperature, MAP, PaCO2 has been studied extensively but the variables like pulsatility, hematocrit or flow rate have received far less attention. Short term neurologic outcome has been related to perioperative blood loss and not to CPB Hematocrit8. Experimental evidence suggests that a hematocrit below 20% may be associated with an abnormal flow distribution to the organs. However, a hematocrit values in the range of 15% to 18% commonly seen during the initial stages of CPB are well tolerated clinically. Physiologic compensatory mechanisms, anesthesia and hypothermia may be responsible6. Cook et al conducted a study to assess the factors affecting cerebral oxygenation during normothermic bypass and hypothermic cardiopulmonary bypass and its adequacy. They concluded that during normothermic bypass, cerebral blood flow increased secondary to hemodilution and decreased cerebral vascular resistance but a normal matching of oxygen demand and delivery was maintained. During hypothermic bypass, hemodilution and hypothermia had equal and opposing effects on cerebral vascular resistance and blood flow with hypothermia, brain oxygen demand and supply both reduced but wasnot closely coupled9 We had calculated the amount of blood to be removed in the ANH group according to the aforementioned formula. According to the formula, on the initiation of CPB the hematocrit should have been higher or equal to twenty two percent in all the patients in ANH group. Despite this, the hematocrit fell below eighteen in two patients in the ANH group. Blood was added twice to pump in the ANH group. This might be because the degree of hemodilution during CPB and the amount of surgical bleeding prior to bypass are not entirely predictable. The efficacy of ANH in avoiding autologous blood transfusion is controversial10.Multiple studies have analyzed the advantages of ANH in terms of reduction of allogenic blood transfusions. This study though not powered to detect such a difference, noted a similar reduction. Taketani et al, Mahoori A et alreported decreased requirement of autologous blood transfusion with ANH11,12. While others like Hohn et al report absence ofreduction in allogenic blood transfusion in cardiac surgery.10 Barile et al conducted a meta-analysis of twenty nine randomized controlled trials which included a total of 2439 patients to assess the incidence of ANH-related number of allogeneic blood transfusions. They concluded that ANH reduces the number of allogeneic blood transfusions in the cardiac surgery setting and resultsin a reduction in the rate of patients who underwent blood transfusions2. Limitations: While our study has evaluated the effect of ANH on hematocrit and systemic oxygen delivery during CPB, it did not investigate the effect of the lowered hematocrit on intraoperative and postoperative organ perfusion and function. Also, our study was not powered to detect the difference in incidence of allogenic blood transfusion between the groups.
CONCLUSION Acute normovolemic hemodilution before cardiopulmonary bypass might lead to decrease in hematocrit values during cardiopulmonary bypass as compared to patients who have not undergone ANH. But the incidence of hematocrit going below the transfusion trigger was similar in both the groups. There was no difference in incidence of blood transfusion in both the groups though our study was not powered to detect statistically significant difference. Delivery of oxygen was maintained in the ANH group despite lowered hematocrit values which was probably due to the higher cardiopulmonary bypass flows in the ANH group as compared to the control group.
REFERENCES
|
|
 Home
Home