Comparison of efficacy of intrathecal bupivacaine plus fentanyl and ropivacaine plus fentanyl in infraumblical surgeries
Abstract Background: Bupivacaine and Ropivacaine are the commonly used drugs in spinal anesthesia. The efficacy of these drugs along with adjuvant fentanyl, remains works better but the question remains unsolved that whether bupivacine plus fentanyl or ropivacine plus fentanyl, which works better. Hence this study was undertaken to compare the efficacy and side effects of these drugs for infraumblical surgeries. Methods: This prospective randomized, double blinded study was conducted among patients undergoing infraumblical surgeries in Sri Muthukumaran Medical College Hospital and Research Institute, Chennai during months of August 2018 to July 2019, for elective surgical procedures. Eighty patients were included in the study with forty cases in group A (Bupivacaine plus fentanyl) and forty cases in group B (Ropivacine plus fentanyl). Data analysis was done using SPSS version 17. Results: Intrathecal isobaric bupivacaine plus fentanyl combination produces a significantly longer duration of analgesia, sensory block and motor block when compared to intrathecal isobaric ropivacaine plus fentanyl combination. Hemodynamic parameters and adverse effects were similar in both the groups with no statistical significant differences. Conclusion: Ropivacaine plus fentanyl causes less motor blockade than bupivacine plus fentanyl and ropivaince plus fentanyl has a greater degree of motor sensory differentiation, it can be used in day care surgery.
Key Words: Bupivacine, Ropivaine, fentanyl, Efficacy, spinal anesthesia
INTRODUCTION
Spinal anaesthesia is a common technique widely used for lower abdominal and lower limb surgeries. Bupivacaine and Ropivacaine are the commonly used drugs for this procedure. Bupivacaine, the most widely used local anesthetic agent, is a chiral compound 1 and racemic mixture of S (−) and R (+) enantiomers. Similarly Ropivacaine, which is an amidetype local anaesthetic, also been used widely for spinal anaesthesia in recent days.2 Although ropivacaine and bupivacaine are quite similar in structure, the former is relatively less toxic in terms of cardiovascular and central nervous systems effects 3. There is evidence that suggests that epidural ropivacaine results in greater sensory blockade and motor block sparing and has lower cardiac toxicity3 potential than bupivacaine.4 To maintain the advantage of an intrathecal anaesthetic agent while improving intra and post operative analgesia, an analgesic adjuvant can be used.5 Some studies have shown that intrathecal opioids can greatly enhance analgesia from subtherapeutic doses of local anaesthetic.6,7 Fentanyl is an opioid that has shown to enhance the analgesic potency of ropivacaine and bupivacaine for spinal anesthesia. 8 Various studies have compared the efficacy and side effect profile of intrathecal bupivacaine and ropivacaine in different surgeries.9,10,11 Whereas, there were only few studies which compared intrathecal use of ropivacaine and bupivacaine along with fentanyl as an adjuvant.10 Hence, this study was undertaken to compare the efficacy and side effects of intrathecal isobaric Bupivacaine plus fentanyl and isobaric ropivacaine plus fentanyl combination for infraumblical surgeries.
MATERIALS AND METHODS
This prospective randomized, double blinded study was conducted among patients undergoing orthopedic surgeries, urological surgeries and lower abdominal surgeries in Sri Muthukumaran Medical College Hospital and Research Institute, Chennai during months of August 2018 to July 2019, for elective surgical procedures. Eighty patients between the age group of 19-60 years, who belongs to American Society of Anesthesiologists (ASA) grade I and II were included in the study. Patients with spinal deformity and previous spinal surgeries were excluded from the study. The study was approved by the ethical committee of this institution. Informed consent was obtained from the study participants before starting the study. The study patients were randomized and divided into two groups with forty participants in 15 mg of 0.5% bupivacaine (3 ml of isobaric bupivacine) with 25 mcg of fentanyl (0.5 ml) in group A and another forty participants in ropivacaine (15 mg of 0.5%) with 25 mcg fentanyl (0.5 ml) in group B. Detailed history and the observations were documented in a proforma by the principal investigator. In the preoperative room, baseline recording of heart rate, respiratory rate, systolic blood pressure and conscious levels of the patients were noted. Based on computer generated random numbers, patients were allotted to either group A or group B. Respective drugs were administered through caudal block in left lateral position using a 23‑gauge short bevel needle under aseptic condition. Neither sedatives nor opioids were administered intraoperatively. HR, BP, SPO2 were recorded just before and after surgical incision and every 5min thereafter till the end of surgery. The duration of motor blockade was defined as time from zero time to return of muscle tone to normal grade or ability to stand. All observed parameters of the study were documented. Visual Analogue Scale (VAS) was used to assess the pain after 4 hours of surgery. Data was entered in Microsoft excel and data analysis was done using statistical tests like chi square test, independent sample t test, Z test and ANOVA, wherever appropriate in Statistical Package for Social Sciences (SPSS) version 17.
RESULTS
In this study among Group A patients (Bupivacaine with Fentanyl) 30% of the participants were less than 30 years of age, 25% of the participants were between 31-40 years of age. In the age group of 41-50 years 30% of the participants were recorded and 15% of the participants belonged to 51-60 years of age group. Likewise among Group B patients 35% of the participants were below 30 years of age, 32.5% of the participants were between 31-40 years of age, 22.5% of the participants were between 41-50 years of age group. in the age range of 51-60 years 10% of the participants were noted in this study. The mean age of the study participants in Group A was 37.98±9.43 and mean age of the participants in Group B was 36.76±6.33. p value was found to be statistically not significant. (p value 0.7117) Among Group A participants 52.5% of them were males and 47.5% of them were females and in Group B 57.5% of the participants were males and 42.5% of the participants were females. the difference between group A and group B for sex was found to be statistically insignificant with p value of 0.6530 Based on ASA classification 97.5% of the participants in Group A were under ASA I and 95% of the Group B participants were under ASA II. The p value was found to be not significant between participants treated with Bupivacaine with Fentanyl and Ropivacaine with Fentanyl. Orthopedic surgery was done for 55% of the participants in Group A and 62.5% of the participants in Group B, abdominal surgery was the type of surgery for 30% and 27.5% of the participants in Group A and B respectively. Urological surgery was done for 15% of Group A patients and 10% of the Group B patients. The difference in type of surgery between group A and group B was not found to be statistically significant. (p value 0.7279).
Table 1: Characteristics of participants in each group
Variables |
Group A (%)N=40 |
Group B (%)N=40 |
P value |
Age group |
|
≤ 30 years |
12 (30) |
14 (35) |
0.7117 |
31- 40 years |
10 (25) |
13 (32.5) |
41-50 years |
12 (30) |
09 (22.5) |
51-60 years |
06 (15) |
04 (10) |
Mean age (±SD) |
37.98±9.43 |
36.76±6.33 |
0.4989 |
Gender |
|
Male |
21 (52.5) |
23 (57.5) |
0.6530 |
Female |
19 (47.5) |
17 (42.5) |
ASA class |
|
ASA I |
39 (97.5) |
38 (95) |
0.5562 |
ASA II |
1 (2.5) |
2 (05) |
Type of surgery |
|
Orthopedic surgeries |
22 (55) |
25 (62.5) |
0.7279
|
Lower abdominal surgeries |
12 (30) |
11 (27.5) |
Urological surgeries |
06 (15) |
04 (10) |
The mean onset of sensory block among Group A participants was 2.67±0.72 and Group B participants were 3.22±0.53 respectively. The difference in onset of sensory block among Group A and Group B participants was found to be statistically significant with p value of 0.0002. Mean onset of motor block among Group A participants and Group B participants were 4.77±1.22 and 4.81±1.41 respectively. But the difference was found to be statistically insignificant. The mean duration of anaesthesia among patients treated with Bupivacaine and Fentanyl was 142.56±23.11 and patients treated with Ropivacaine and Fentanyl was 115.13± 16.76. The p value was found to be highly statistically significant. (p value 0.0000). In this current study the difference in mean duration of surgery between Group A and Group B was found to be not statistically significant. The mean duration of motor blockade among Group A patients were 174.16±54.31 and the mean duration of motor blockade among Group B patients was 142.47±38.13. the p value was found to be statistically significant(p value 0.0034). the proportion of cases with Bromage score of 3 for Group A and Group B participants was 38/40 (95) and 31/40 (77.5) respectively. The difference for proportion of cases with Bromage score of 3 was found to be statistically significant. (p value 0.0239)
Table 2: Clinical profile of participants in each group
Variables |
Group A |
Group B |
P value |
Onset of sensory block (in mins) |
2.67±0.72 |
3.22±0.53 |
0.0002* |
Onset of motor block (in mins) |
4.77±1.22 |
4.81±1.41 |
0.8924 |
Duration of anaesthesia (in mins) |
142.56±23.11 |
115.13± 16.76 |
0.0000* |
Mean duration of surgery (in mins) |
112.31±34.79 |
125.14±29.12 |
0.0776 |
Duration of motor blockade (in mins) |
174.16±54.31 |
142.47±38.13 |
0.0034* |
Cases with Bromage score of 3 |
38/40 (95) |
31/40 (77.5) |
0.0239* |
*Significant
The mean heart rate of participants in Group A at baseline was 104.2 and at 120 mins was 97.8 whereas the mean heart rate of Group B participants was 105.1 at baseline followed by 98.9 at 120 mins. Also there was no statistical significant difference in heart rate was found between the two groups.
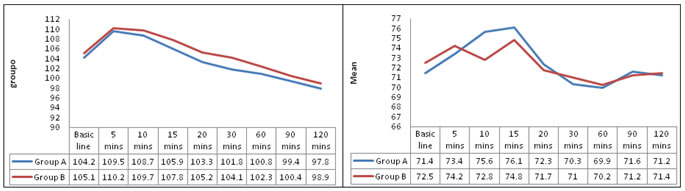
Figure 1 Figure 2
Figure 1: Mean heart rate of participants in group A and group B; Figure 2: MAP of participants in group A and group B
In Figure 1, The Mean Arterial Pressure (MAP) for Group A participants at baseline was found to be 71.4 at 60 mins the MAP falls to 69.9 and at 90 mins there was a rise in MAP to 71.6 followed by 71.2 at 120 mins. While the mean arterial pressure for Group B participants was found to be 72.5 at baseline, at 10 mins the MAP was 72.8 and a hike in MAP was found at 15 mins followed by a fall in mean arterial pressure and at 120 mins the MAP was 71.4. Also there was no statistical significant difference in MAP was found between the two groups.
In Figure 2, In this study Nausea and Vomiting was present in 5% and 2.5% of Group A and Group B patients respectively. Urinary retention was noted among 2.5% of the Group A and Group B patients each. Pruritis was present among 2.5% of the Group B participants and Hypotension was seen among 2.5% of the Group B participants where Group A participants had no pruritis or Hypotension as adverse effect. No statistically significant differences were found between the two groups, with respect to adverse effects.
Table 3: Proportion of Adverse effects in each group
Adverse effects |
Group A |
Group B |
Nausea and vomiting |
2 (5) |
1 (2.5) |
Pruritis |
0 |
1 (2.5) |
Urinary retention |
1 (2.5) |
1 (2.5) |
Respiratory depression |
0 |
0 |
Hypotension |
0 |
1 (2.5) |
DISCUSSION
In this study in both the groups the sensory block was reported in cephalad direction till T7. Similarlt studies conducted by Mantouvalou et al.,12 and Ogun et al.,11 found a similar cephalad extent of sensory block after isobaric bupivacaine or ropivacaine subarachnoid anesthesia. However, Malinovsky et al.,9 found a lower cephalad extent (median dermatome level T9) of anesthesia associated with less intense anesthetic blockade in the ropivacaine group, resulting in requirement of supplemental analgesia to perform surgery. This difference can be explained by use of fentanyl as adjuvant in our study which improves the quality of the block as well as the increased drug volume could have led to a higher cephalad extent of the local anesthetic solution. In the present study, Nausea and Vomiting was present in 5% and 2.5% of Group A and Group B patients respectively. Urinary retention was noted among 2.5% of the Group A and Group B patients each. Pruritis was present among 2.5% of the Group B participants and Hypotension was seen among 2.5% of the Group B participants where Group A participants had no pruritis or Hypotension as adverse effect. No statistically significant differences were found between the two groups, with respect to adverse effects. Whereas McNamee et al.,13 in their study found 6% patients in the ropivacaine group to have bradycardia and required atropine to treat the same; they had used a higher dose of ropivacaine that is, 3.5 ml 0.5%, total of 17.5 mg. The result of our study is comparable with a study done by Koltka et al.,10 2009, who also did not found statistically significant difference in HR and arterial blood pressure in their study.
CONCLUSION
Intrathecal isobaric bupivacaine plus fentanyl combination produces a significantly longer duration of analgesia, sensory block and motor block when compared to intrathecal isobaric ropivacaine plus fentanyl combination. As ropivacaine is less lipophilic than bupivacaine causes relatively less motor blockade and it has a greater degree of motor sensory differentiation, it can be used in day care surgery.
ACKNOWLEDGMENT
I would like to thank all, who has guided me by extending their knowledge and experience right from the inception to the completion of the work. Also, I would like to acknowledge the medical superintendent and all the staffs, for their support during the study period. Last but not least I am thankful to my study participants, without whom, this study would not have been possible.
REFERENCES
- Calvey TN, Williams NE. Isomerism and anaesthetic drugs. In: Calvey TN, Williams NE, editors. Principles and practice of pharmacology for anaesthetists. 3rd Edn. Oxford: Blackwell Science; 1997. p. 108-45.
- Boztuğ N, Bigat Z, Ertok E, Erman M. Intrathecal ropivacaine versus ropivacaine plus fentanyl for out-patient arthroscopic knee surgery. Journal of international medical research. 2005 Jul;33(4):365-71.
- Scott DB, Lee A, Fegan D, Bowler GM, Bloomfield P, Lundh R. Acute toxicity of ropivacaine compared with that of bupivacaine. Anesth Analg 1989;69:563-9.
- Knudsen K, Beckman SurkulaM, Blomberg S, Sjovall J, Edvardsson N. Central nervous and cardiovascular effects of IV infusions of ropivacaine. Br J Anaesth 1997;78:507-14.
- De Kock M, Gautier P, Fanard L, Hody JL, Lavand’homme P: Intrathecal ropivacaine and clonidine for ambulatory knee arthroscopy: a doseresponse study. Anesthesiology 2001; 94: 574 – 578.
- Ben-David B, Solomon E, Levin H, Admoni H, Goldik Z: Intrathecal fentanyl with small-dose dilute bupivacaine: better analgesia without prolonging recovery. Anesth Analg 1997; 85: 560 – 565.
- Wang C, Chakrabarti MK, Whitwam JG: Specific enhancement by fentanyl of the effects of intrathecal bupivacaine on nociceptive afferent but not on sympathetic efferent pathways in dogs. Anesthesiology 1993; 79: 766 – 773.
- Seetharam KR, Bhat G. Effects of isobaric ropivacaine with or without fentanyl in subarachnoid blockade: A prospective double-blind, randomized study. Anesthesia, essays and researches. 2015 May;9(2):173.
- Malinovsky JM, Charles F, Kick O, Lepage JY, Malinge M, Cozian A, et al. Intrathecal anesthesia: Ropivacaine versus bupivacaine. Anesth Analg. 2000;91:1457–60.
- Koltka K, Uludag E, Senturk M, Yavru A, Karadeniz M, Sengul T, et al. Comparison of equipotent doses of ropivacaine-fentanyl and bupivacaine-fentanyl in spinal anaesthesia for lower abdominal surgery. Anaesth Intensive Care. 2009;37:923–8.
- Erturk E, Tutuncu C, Eroglu A, Gokben M. Clinical comparison of 12 mg ropivacaine and 8 mg bupivacaine, both with 20 microg fentanyl, in spinal anaesthesia for major orthopaedic surgery in geriatric patients. Med Princ Pract. 2010;19:142–7.
- Mantouvalou M, Ralli S, Arnaoutoglou H, Tziris G, Papadopoulos G. Spinal anesthesia: Comparison of plain ropivacaine, bupivacaine and levobupivacaine for lower abdominal surgery. Acta Anaesthesiol Belg. 2008;59:65–71.
-
Source of Support: None Declared Conflict of Interest: None Declared
McNamee DA, McClelland AM, Scott S, Milligan KR, Westman L, Gustafsson U. Spinal anaesthesia: Comparison of plain ropivacaine 5 mg ml(-1) with bupivacaine 5 mg ml(-1) for major orthopaedic surgery. Br J Anaesth. 2002;89:702–6.