Official Journals By StatPerson Publication
|
Table of Content - Volume 12 Issue 3 -December 2019
Evaluation of ondansetron and granisetron for prevention of spinal induced hypotension
Dnyaneshwar R Fating1*, Shailesh Chouksey2, Sanjay B Agrawal3
{1Associate Professor, 2Senior Resident, Department of Anaesthesiology} {3Statistician-cum-Assistant Professor, Department of PSM} IGGMC Nagpur, Maharashtra, INDIA. Email: dfating@gmail.com
Abstract Background: Spinal anaesthesia, a type of regional anaesthesia is a very commonly used anaesthesia technique for lower abdominal and lower limb surgeries. Apart from sympathetic blockade Bezold Jarisch Reflex (BJR) is one of the mechanism responsible for hypotension and bradycardia associated with spinal anaesthesia. Action of ondansetron and granisetron as 5HT3 antagonist may have an effective role in prevention of incidence of hypotension and bradycardia occurring after spinal anaesthesia. Aim: To study the effects of Ondansetron and Granisetron administered intravenously in premedication on haemodynamic changes associated with spinal anaesthesia. Material and Methods: prospective observational study included total 100 patients posted for lower abdominal surgeries under spinal anaesthesia. One group received injection ondansetron (group o) 4 mg intravenously and other group received injection granisetron (group g) 1mg intravenously. After spinal anaesthesia incidence of bradycardia and hypotension noted in both the group. Results: 8% incidence of bradycardia was found in group-o as compared to group-g (20%). Fall in blood pressure was more in group-g than group-o. Only 5 patients of group-o received vasopressor compared to 13 patients of group-g. Conclusion: ondansetron is better than granisetron for prevention of bradycardia and hypotension after spinal anaesthesia in lower abdominal surgeries. Key Words: Spinal anaesthesia, ondansetron, granisetron.
INTRODUCTION Spinal anaesthesia, a type of regional anaesthesia is a very commonly used anaesthesia technique for lower abdominal and lower limb surgeries. Because of excellent surgical relaxation, reduced stress response, maintenance of consciousness and prevention of aspiration, subarachnoid block has become the preferred mode of anaesthesia. However it has certain disadvantages like hypotension, bradycardia, failure of block etc. The reported incidence of hypotension is 33% and that of bradycardia is 13%, in non-obstetric patients. In obstetric, non-labouring patients, the incidence of hypotension increases as high as 50–60%.1 Hypotension occurs due to decrease in systemic vascular resistance because of sympathetic block which leads to redistribution of central blood volume to lower extremities and splanchnic beds resulting in decreased venous return to heart. This hypotension and bradycardia may have deleterious effects on geriatric patients, obstetric patients and patients having ischaemic heart Disease. Hypotension can be managed with fluids, medications, and physical methods like positioning, leg bindings, etc2 Bezold Jarisch Reflex (BJR) is one of the mechanisms responsible for hypotension and bradycardia associated with spinal anaesthesia. Vigorous contraction of poorly filled ventricles due to reflex sympathetic activation mediated through baroreceptors because of decrease venous return, cause release of serotonin. This serotonin acts on 5HT3 chemoreceptors present on cardiac vagal afferents. Signal from cardiac vagal afferent stimulates serotonin chemoreceptors i.e. 5HT1 and 5HT2 in cardiovascular centre of brain stem. Activation of these serotonin chemoreceptors leads to stimulation of parasympathetic activity causing bradycardia and blockade of sympathetic activity causing hypotension.3, 4 5HT3 receptor antagonist like Ondansetron and Granisetron are routinely used in premedication for prevention of postoperative nausea and vomiting5. Both being 5HT3 receptor antagonist, have serotonin (5HT) receptor antagonist action on CTZ (Chemoreceptor Trigger Zone) of the Area Postrema as well as peripheral (Enteric and Cardiac) receptors. Considering this 5HT3 antagonist action, they may have an effective role in prevention of incidence of hypotension and bradycardia occurring after spinal anaesthesia5. Hence the present study was planned to evaluate the role of Ondansetron and granisetron in prevention of hypotension and bradycardia associated with spinal anaesthesia.
MATRIAL AND METHODS After obtaining written informed consent and satisfying inclusion and exclusion criteria for 100 patients were included in study. Patients were kept nil by mouth for 6 hrs. On the day of surgery Intravenous access secured with intravenous cannula. In operation theatre Patient preloaded with ringer lactate (10 ml/kg) and multipara monitor with facility of Non-invasive blood pressure (NIBP), Electrocardiogram (ECG), pulse oxymetry (SPO2) attached. Patients received either Inj. Ondansetron 4 mg or Inj. Granisetron 1 mg intravenously slowly after dilution in normal saline up to 5 ml before 10 minutes of spinal anaesthesia. Baseline parameters Heart rate, Systolic Blood Pressure (SBP), Diastolic Blood Pressure (DBP), Mean Arterial Blood Pressure (MABP), SPO2 were recorded. Spinal anaesthesia with 25 G spinal needle performed in L3-L4 interspace in lateral position with table kept in horizontal position. After free flow of cerebrospinal fluid Inj. Bupivacaine 0.5% hyperbaric 3.2 ml injected intrathecally in subarachnoid space. Patient immediately turned supine. Completion of spinal anaesthesia was considered as time 0 min, readings of HR, SBP, DBP, MABP(2/3DBP+1/3SBP) were recorded at 1 min , 3 min, 5 min, 7 min, 10 min, 15 min, 20 min, 30 min, 40 min till 90 min or completion of surgery whichever was earlier. Sensory level was accessed with pin prick method and observations were noted. Intraoperative incidence of hypotension and bradycardia were noted and treated with Inj. Mephenteramine 6 mg and Inj. Atropine 0.6 mg respectively. Patients with inadequate analgesia, requiring analgesic medication or general anaesthesia were excluded from study. Statistical Analysis: Continuous variables (age, height, weight, intraoperative vital parameters and duration of surgery) were presented as Mean ± S.D. Categorical variables (Gender, ASA status, vasopressor requirement, anticholinergic requirement and level of Anaesthesia) were expressed in frequency and percentage. Age, duration of surgery, intraoperative vital parameters between 2 groups were compared by performing unpaired t-test. Categorical variables between 2 groups were compared by performing Pearson’s chi square test. <0.05 was considered significant. Statistical software STATA version 13 and SPSS software version 21 were used for analysis.
OBSERVATION AND RESULTS Our study included total 100 patients of ASA physical status I and II posted for elective infra-umbilical surgeries. Patients of age group 20- 60 yrs. were divided into two groups namely Group O (n= 50) and group G (n=50).
Table 1: Distribution of patients according to age, weight and height
Table 2: Sex distributions of patients in two groups
Chi square test 0.39, d.f. = 1, p=0.529 no significant association Patients in both the groups were comparable with respect to sex (p value > 0.05 non-significant)
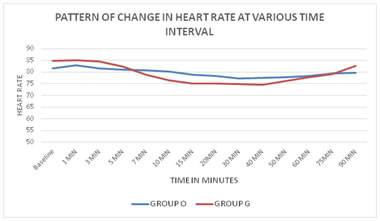
Table 3: Pattern of change in heart rate at various time interval
Graph 3: Changes in Heart Rate at various time interval in two groups
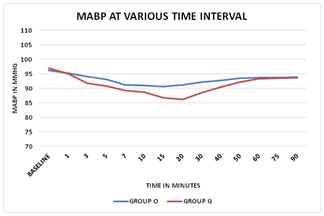
Table 4: Pattern of intraoperative changes in mean arterial Pressure
Graph 4: Pattern of intraoperative changes in Mean Arterial Pressure The study suggest that when 1 mg I.V. Granisetron or 4 mg I.V.Ondansetron were used before spinal anaesthesia, in both the groups there was a gradual decrease in mean arterial pressure which started 1st minute after spinal Anaesthesia and continued till 15 minutes in Group O compared to 20 min in Group G. After mentioned time interval, mean arterial pressure started to increase and became almost stable after 40 minutes of surgery. The fall in mean blood arterial pressure was more in group of patients those who received iv granisetron than that of Ondansetron and it was significant from 15th minute until 30th minute of surgery.
Table 5: Requirement of vasopressor and anticholinergic
Above table indicate that there is significant difference in requirement of vasopressor (P value= 0.035). With significantly less requirement in Group O than Group G.
Table 6: Incidence of bradycardia in both Groups
Incidence of bradycardia was significantly lower in Group O than Group G with P value = 0.0495
DISCUSSION Spinal anaesthesia also called sub-arachnoid block is form of neuraxial regional anaesthesia in which local anaesthetic or opioid agent is injected intrathecally in subarachnoid space. It is safe and effective form of anaesthesia which is most common and preferred technique of anaesthesia (with > 90% success rate)6 over general anaesthesia for lower abdominal and lower limb surgeries. Local anaesthetic injected in subarachnoid space in cerebrospinal fluid (CSF) provides temporary sensory and motor block. Spinal induced hypotension and bradycardia has always been concern for anaesthesiologists. Hypotension after spinal anaesthesia is multifactorial but they can be mainly attributed to sympathetic blockade (responsible for peripheral vasodilatation), Bezold jarisch reflex, unopposed parasympathetic activity, blockade of cardio-accelerator fibres etc. Various methods are used to prevent spinal induced hypotension and bradycardia like fluids, medications, but none is ideal. Ondansetron and Granisetron are 5HT3 receptors antagonists mainly used to prevent postoperative nausea and vomiting. References are available regarding prevention of spinal induced hypotension and bradycardia with 5HT3 antagonists. Action is mediated through Bezold jarisch reflex. So the present study titled “Evaluation of Ondansetron and Granisetron for prevention of spinal induced hypotension” was done. Present study was done on patients of both the sexes posted for elective lower abdominal surgeries. Total 100 patients were included in the study. They were divided in two groups- Group O – Ondansetron Group – 50 Patients Group G - Granisetron group – 50 Patients Mean age ± S.D. for group O and group G were 46.66 ± 9.48 and 45.7 ± 9.23 respectively. Range for both the study group was 20 to 65 years. Statistically patients in two groups were comparable (P value = 0.384) with respect to age. Mean height ± S.D. for group O and group G were 163.88 ± 8.03 and 163.6 ± 4.77 respectively. Also mean weight ± S.D for group O and group G were 61.1 ± 8.88 and 64.26 ± 8.27 respectively. Patients in both the groups with respect to height (P value = 0.388) and weight (P value=0.215) were statistically comparable. In both the groups male population was predominant i.e. 62% male patients in group O and 68% in group G. But statistically male and female were comparable in both the groups (P value- 0.529). Duration of surgery in two groups was fairly comparable as mean ± S.D. for group O was 70.3 ± 18.85 and group G was 71.1 ± 13.93 (P value - 0.809) In our study we administered Ondansetron 4 mg and Granisetron 1mg intravenously in premedication 10 minutes before spinal anaesthesia. The purpose of administering the drugs 10 minutes before spinal anaesthesia was to obtain its peak effects at the onset sympathetic blockade. In most of the studies, on prevention of postoperative nausea and vomiting, the dose of Ondansetron and Granisetron was 4mg and 1mg respectively. (Ronald D. Miller and et al 2015 page no. 2965)7 Laxmi L et al in year 2017 studied the effect of various doses of Ondansetron as 4 mg and 8 mg on maternal haemodynamic posted for caesarean section under spinal anaesthesia and they found no additional benefits of increased dose.8 In present study, patients of ASA grade I and II were included excluding patients on any antihypertensive drug treatment or patients with history of diabetes mellitus type II. Majority of patients i.e. Group O (86%) and Group G (88%) were belonged to ASA grade I. Which was statistically comparable as P value > 0.05 (P = 0.766) Statistical analysis of all the four parameters did not reveal any significant difference between the two groups of patients. In our study T6 level was required to have adequate analgesia for lower abdominal surgeries, so we administered 3.2 ml of 0.5% hyperbaric bupivacaine 7,9,10. Assessment of sensory level was done by pin prick sensation at 2 min interval. 44 patients in the group O and 43 patients in group G had T6 level. Only 2 patients in group O and 3 patients in group G had T5 level. Rest of the patients in group O and G had T7 level. The difference in sensory level in two groups was statistically not significant (P value- 0.67). In our study baseline mean heart rate was 81.5 ± 10.66 in Group O and 84.82 ± 10.41 in Group G which was comparable statistically. After spinal anaesthesia, gradual fall in heart rate was noted up to 30 minutes in group O compared to 40 min in Group G and afterwards increase till end of surgery. When intragroup statistical analysis was done there was significant fall in heart rate from 7 to 75 minutes in Group G compared to 15 to 50 minutes in Group O. The pattern of fall in heart rate was observed at more time interval in Group G as compared to Group O. On intergroup comparison the fall in heart rate was statistically significant only at 10 and 15 minutes. Overall incidence of bradycardia was more in Group G (n=11) in contrast to Group O (n=4) which was statistically significant (P value = 0.0495) The anticholinergic i.e. atropine was used in only one patient of Group G and none of the patient in Group O. Our results correlate with study results of Marashi et al (2014) they also concluded that spinal induced bradycardia can be prevented with IV Ondansetron11. Also BK Shrestha and et al (2014) studied they effect of Granisetron in prevention of Hypotension and Bradycardia due to spinal anaesthesia. They concluded that Granisetron given intravenously does not decrease the incidence of hypotension and bradycardia following subarachnoid block in patients undergoing lower abdominal surgery which also supports our result findings12. Arivumani TA and et al in 2016 in their study found that episodes of bradycardia in parturient were low in Ondansetron group which also favour our result findings13. S. Nallam and et al in 2015 during their study with IV Ondansetron on haemodynamic monitors of patients posted for shoulder arthroscopic surgery under interscalene neuraxial block. Got results which suggested that patients receiving IV Ondansetron have less episodes of hypotension and bradycardia which again have similarity with our study results14. The baseline mean arterial blood pressure in Group O and Group G were 96.93 ± 7.06 and 96.24 ± 7.90 respectively which were statistically comparable. Following subarachnoid block, fall in mean arterial blood pressure was observed in Group O up to 15 minutes of time interval as compared to 20 minutes of time interval in Group G. Afterwards increasing trends were noted till the end of surgery. The intragroup statistical analysis of mean arterial blood pressure at various time interval compared with baseline was suggestive of significant fall in mean arterial blood pressure from 3 to 60 minutes in Group O, contrary to 1 to 75 minutes of surgery in Group G. On intergroup comparison fall in mean arterial blood pressure was statistically significant at 15, 20 and 30 minutes of time interval. So when the effects of spinal anaesthesia achieved, mean arterial blood pressure was more stable in Group O compared to Group G. This results can also be consolidated by the requirement of vasopressor which was found to be in 5(10%) cases of Group O and 13(26%) cases of Group G which was also statistically significant(P=0.0395). Study by Omyma et al in 2015 included 4 groups of drug Ondansetron, Granisetron, Ephedrine and control group with normal saline. They found that despite of decrease in mean arterial blood pressure in all groups the fall was least in patients receiving IV Ondansetron and maximum fall was noted in patients receiving normal saline. These results are in correlation of our study results15. Marashi and et al (2014) in there study concluded that Ondansetron IV significantly reduces the incidence of spinal induced hypotension. These results are also similar with results of our study 11. T. Sahoo et al, 2012 also studied the effect of iv Ondansetron 4 mg on haemodynamic parameters occurring in parturient undergoing elective caesarean section. They concluded that Ondansetron 4 mg iv given 5 min before subarachnoid block reduces the incidence of hypotension and requirement of vasopressor1. In same way Arivumani T and et al 2016 found similar results with iv Ondansetron.14 Ahmed A, Eldaba, Yasser M. Amr et al. (2015) when used 1 mg Granisetron as premedication before spinal anaesthesia, observed that it significantly reduces the occurrence of spinal induced decrease in MAP16. In year 2014 Shah SARA and et al studied the effect of iv Ondansetron 8 mg given prior to spinal anaesthesia in elderly patient their results are also in favour of our study17. Manal M. Rashad , Manal S. Farmawy in year 2013 found that in parturient females undergoing elective caesarean section, intravenous 4 mg Ondansetron before subarachnoid block significantly decreased both the hypotension and the doses of vasopressor which are in consensus with our results. Any study is incomplete without mentioning the side effects and limitations. In our study known and specific side effects of Ondansetron and granisetron like QTc prolongation was not found in patients of both the groups. The limitation was that our study did include obstetric, paediatric and geriatric patients, so this study results cannot be applied to these group of patients’ population. Control group was not taken in this study so randomised control study is required to substantiate the results of our study. In present study, observations and analysis of data is suggestive of better haemodynamic stability with Ondansetron after spinal anaesthesia for lower abdominal surgeries.
CONCLUSION From our study we can conclude that 4 mg intravenous Ondansetron is more effective than intravenous 1 mg Granisetron in prevention of hypotension and bradycardia associated with spinal anaesthesia in lower abdominal surgeries.
REFERENCES
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home