Utility of video stylet in evaluating vocal cord mobility after thyroid and para thyroid surgery compared with direct laryngoscopy
Khatija Y Dalvani1, Jigisha P Badheka2*, Vrinda Oza3, Jaykishan Gol4, Mayur Patel5
1Tutor, 2Associate Professor, 3Assistant Professor, 4IIrd Year Resident Doctor,5IInd Year Resident Doctor, Department of Anaesthesiology, P.D.U Medical College,Rajkot, pin code-360001,INDIA.
Email: jagu_jigi@yahoo.com, dalvanikhatija@gmail.com
Abstract Background: Following thyroid surgery, it is necessary to rule out reccurent laryngeal nerve palsy which can be done by indirect laryngoscopy (IDL), video laryngoscopy or fiber-optic laryngoscopy (FL). FL is the gold standard for VCF assessment, but having limitations like high cost, availability and difficult technique. Video-stylet allows good assessment of VCF with less sympathetic stimulation. Aim of our study was to compare Macintosh laryngoscopy and video stylet for ease of vocal cord visualization, assessment of VCF, hemodynamic stability and patient comfort. Method: After approval from ethical committee, prospective study was carried out on 100 patients of 18-60 years of ASA grade I to III of either sex undergoing thyroid or parathyroid surgery with pre-operative normal VCF on IDL. They were randomly divided into two groups of 50 each: Group A - Direct laryngoscopy (DL) and Group B- Video stylet. Patient’s comfort, ease of vocal cord visualization, VCF and hemodynamic parameters were noted at the time of extubation and were statistically analyzed. Postoperative IDL was performed to confirm the findings. Results: We found better visualization of VC and stable hemodynamics with video stylet compared to DL. Patient comfort with group B is better compared to group A. Conclusion: Video styl et al lows accurate assessment of VCF with good patient comfort and stable hemodynamic in the immediate post-operative period compared to DL.
Key Words: Thyroid surgery, Parathyroid Surgery, Vocal cord mobility, Video Stylet, Recurrent Larygeal nerve palsies
INTRODUCTION
Recurrent Laryngeal Nerve (RLN) Palsy is a recognized complication after Thyroid and Parathyroid surgery. The reported incidence of permanent nerve damage was 1-3% and temporary nerve injury was 5-8% 1.Unilateral RLN palsy results in swallowing dysfunction, breathy voice and aspiration in early postoperative period while bilateral RLN palsy results in airway compromise requiring emergency tracheostomy. So, early diagnosis of RLN palsy is crucial to avoid such complications. There are various methods available to test normal functionality of Vocal cords (VCF) like Fiberoptic Laryngoscopy (FL), Indirect laryngoscopy(IDL), video-laryngoscopy and use of Ultrasonography (USG). FL is considered gold standard for detecting abnormality of VCF as it allows better visualization of VC. But FL is costly, requires training to perform the procedure and causes patient discomfort. USG is also not readily available. Macintosh Laryngoscopy is frequently used to assess VCF after extubation and it is routinely used in our institute but it is associated with rise in hemodynamic parameters due to sympathetic stimulation. Video-stylet is a good alternative to assess VCF. No studies have used the video stylet for assessment of VCF. So, we decided to compare Macintosh Laryngoscopy and Video-stylet to assess VCF, ease of vocal cord visualization, hemodynamic stability and patient comfort.
MATERIALS AND METHODOLOGY
After approval from ethical committee, this prospective study was carried out on 100 adult patients of ASA grade I to III in age group of 18-60 years of either sex undergoing thyroid and parathyroid surgery with pre-operative normal VCF on IDL. They were randomly divided in to two group of 50 each:
Group A - Direct laryngoscopy (DL)
Group B- Video- stylet
Pre-anaesthetic evaluation was done and ASA grading done accordingly. Preoperative Indirect Laryngoscopy (IDL) was done to rule out any preexisting vocal cord dysfunction and documented and patient with any vocal cord dysfunction were excluded from the study. All routine preoperative investigations including Hb, RBS, RFTs, TFT, Coagulation Profile, Chest X Ray, X Ray Neck AP and Lateral view and 12 lead ECG were done. Written and informed consent was obtained. Standard monitors like NIBP, pulse oximeter and continuous ECG were applied to all patients. All patients were given general anesthesia according to standard protocol. An immediate postoperative examination was performed at the time of extubation either with laryngoscope (DL) or with video stylet in group A or B respectively. Patient comfort, Ease of VC visualization, postop voice quality and change in haemodynamic parameters were noted in both the groups. Post Operative VCF was assessed by DL or Video stylet and confirmed by IDL on follow up. Ease of vocal cord visualization was noted as “Good” (Fully visible vocal cord), “Fair” (Partially visible vocal cord) or “Poor” (Not visible). Post operative voice quality was assessed in both groups. Monitoring of Hemodynamic parameters was done at 1 min,3 min,5 min,10 min and 15 min after extubation in both the groups.
STATISTICAL ANALYSIS:
Continuous variables are presented as the mean ± SD and categorical variables are presented as frequencies (percentage of patients). The P value < 0.05 was considered as statistically significant.
RESULTS
Our study shows that demographic data were comparable in both groups (Table 1). We found that ease of vocal cord visualization was good with video-stylet compared to DL (Table 2 and Figure 1).Postop voice quality is also good with video stylet compared to DL. (Figure 2) We found better hemodynamic stability with group B compared to group A (Table 3 and Figure 3)
Table 1: Demographic distribution
Table 2 : Ease of vocal cord visibility
Table 3 : Hemodynamic parameter
TABLE 1: DEMOGRAPHIC DATA
|
Group A
(Mean ± SD) |
Group B
(Mean ± SD) |
P value |
Age |
39 ± 12.11 |
41.34 ± 12.08 |
0.33 |
Weight |
53.5 ± 8.967 |
52.56 ± 9.033 |
0.60 |
Height |
151.24 ± 4.405 |
151.22± 3.732 |
0.98 |
Sex Ratio (M/F) |
8/42 |
10/40 |
0.60 |
TABLE 2: EASE OF VOCAL CORD VISIBILITY
|
|
Group A |
Group B |
Fully Visible |
Good |
25 (50%) |
40 (80%) |
Partially Visible |
Fair |
10 (20%) |
10(20%) |
Not Visible |
Poor |
15 (30%) |
0 |
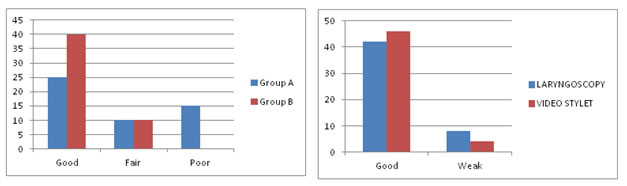
Figure 1: Ease of vocal cord visibility Figure 2: Post op voice quality
Table 3: HEMODYNAMIC PARAMETERS
|
Mean HR |
|
MAP |
|
|
Group A |
Group B |
P value |
Group A |
Group B |
P value |
At 1 Mins |
82.56±5.23 |
85.84±8.37 |
0.02 |
74.43±3.061 |
78.51±4.902 |
0.0001 |
At 3 Mins |
80.54±5.17 |
85.75± 8.47 |
0.0003 |
74.45±3.245 |
76.61±4.636 |
0.008 |
At 5 Mins |
80.56±4.95 |
85.94±7.70 |
0.0001 |
74.84±3.202 |
77.75±4.671 |
0.0004 |
At 10 Mins |
81.52±5.55 |
86.63±8.030 |
0.0004 |
74.86±3.064 |
77.82±3.846 |
0.0001 |
At 15 Mins |
80.40±5.02 |
85.68±8.00 |
0.0001 |
74.64±3.050 |
77.54±3.407 |
0.0001 |
|
|
|
|
|
|
|
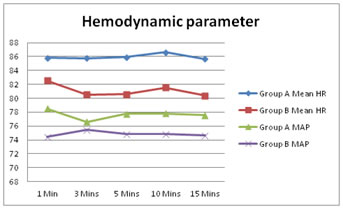
Figure 3
DISCUSSION
Thyroidectomy is a common surgical procedure performed worldwide and RLN injury remains one of the major postoperative complication. Unilateral RLN palsy can lead to hoarseness of voice whereas bilateral RLN palsy leads to RLN palsy leads to airway obstruction and jeopardize the life of patient.(2). So assessment of VCF is of vital importance in both preoperative and postoperative evaluation of patients undergoing this type of surgery. Assessment of VC movement at the time of extubation is done with conventional Laryngoscopy by Macintosh but very often patients cough and gag making proper assessment difficult. Macintosh laryngoscopy is also associated with rise inhemodynamic parameters due to sympathetic stimulation which may be deleterious in susceptible individuals. Video stylet is a good alternative to assess VCF. With video-stylet upward force required to align the oral, pharyngeal and laryngeal axes to obtain glottic view can be reduced. So Videostyl et al lows ease of vocal cord visualization with less sympathetic stimulation. Several studies have been done to assess the function of VC with use of direct laryngoscopy, fiberoptic laryngoscopy, USG. But no study has used Videostylet for assessment of VC. So, we decided to do this study to compare DL and videostylet for assessment of VC function. Kundra P et al3 have compared the patient comfort and assessment accuracy of post-operative vocal fold mobility with Macintosh laryngoscope and Nasal fiberoptic endoscope (NFE)and assessed the vocal cord mobility, patient reactivity score and hemodynamic parameters. They have found that NFE provides accurate assessment of vocal fold mobility with reasonable patient comfort as compared to Macintosh Laryngoscope while in our study we have compared Macintosh laryngoscope and Videostylet and assessed VCF, ease of visualization, hemodynamic parameters and patient comfort. Lacoste L et al 4 have compared direct, indirect and fiberoptic laryngoscopy to evaluate vocal cord paralysis after thyroid surgery and found that Flexible laryngoscopy was easy to perform in 96.5% of the patients versus 65 and 55 % with the direct and indirect laryngoscopies. Variations in monitored cardiovascular parameters were significantly lower with flexible and indirect laryngoscopies than with direct laryngoscopy. In our study we found better ease of visualization of vocal cord and stable hemodynamic with videostylet compared to Macintosh laryngoscope. Amarjeet Kumar et5 al have done an observational study for the assessment of functionality of vocal cords using ultrasound before and after thyroid surgery and they found USG can be a good alternative for examination of functionality of vocal cord perioperatively. In our study, we compared DL and videostylet for assessment of VC function.USG requires expertise but videostylet is easy to use. Dionigi et al6 have used Fiberoptic Nasal larygoscopy (FNL) for detection of VC palsy after thyroid surgery While our study compared videostylet and Macintosh laryngoscopy for VCF evaluation.
CONCLUSION
Video stylet for assessment of VCF is technically easy, more accurate, with less hemodynamic changes and comfortable for the patients compared to Macintosh laryngoscope. Ease of visualization of VCF is better with video stylet compared with Macinosh laryngoscopy.We propose that video stylet can be used routinely for the postoperative evaluation of VCF by all anesthesiologists for thyroid and parathyroid surgery.
REFERENCE
- Jeannon, J. , Orabi, A. A., Bruch, G. A., Abdalsalam, H. A. and Simo, R. (2009), Diagnosis of recurrent laryngeal nerve palsy after thyroidectomy: a systematic review. International Journal of Clinical Practice, 63: 624-629
- Hayward NJ, Grodski S, Yeung M, Johnson WR, Serpell J. Recurrent laryngeal nerve injury in thyroid surgery: A review. ANZ J Surg. 2013;83:15–21
- Kundra, Pankaj, Vinoth Kumar, Krishnamachari Srinivasan, Surianarayanan Gopalakrishnan, and Sudeep Krishnappa. "Laryngoscopic Techniques to Assess Vocal Cord Mobility following Thyroid Surgery."ANZ Journal of Surgery 80.11 (2010): 817-21
- Lacoste L, Karayan J, Lehuedé MS, Thomas D, Goudou-Sinha M, Ingrand P, et al. A comparison of direct, indirect, and fiberoptic laryngoscopy to evaluate vocal cord paralysis after thyroid surgery. Thyroid 1996;6:17-21.
- Amarjeet Kumar,Chandni Sinha,Ajeet Kumar,Akhilesh Kumar Singh,Harsh Vardhan,KrantiBhavana,and Ditipriya Bhar.Assessment of functionality of vocal cords using ultrasound before and after thyroid surgery: An observational study.Indian J Anaesth.2018Aug; 62(8):599-602.
- Dionigi, G., Boni, L., Rovera, F. et al. Postoperative Laryngoscopy in thyroid surgery : proper timing to detect reccurent laryngeal nerve injury.Langenbecks Arch Surg (2010) 395: 327-331.
- Hermann M, Alk G, Roka R, Glaser K, Freissmuth M. Laryngeal recurrent nerve injury in surgery for benign thyroid diseases: Effect of nerve dissection and impact of individual surgeon in more than 27,000 nerves at risk. Ann Surg. 2002;235:261–8
- Joliat GR, Guarnero V, Demartines N, Schweizer V, Matter M. Recurrent laryngeal nerve injury after thyroid and parathyroid surgery: Incidence and postoperative evolution assessment. Medicine. 2017;96:e6674.
- Mihai, R., and Randolph, G.W. (2009). Thyroid Surgery , Voice and the Laryngeal Examination — Time for Increased Awareness and Accurate Evaluation, World Journal of Endocrine Surgery, September-December; 1(1):1-5
- Djearadjane S, Rajan S, Paul J, Kumar L. Efficacy of dexmedetomidine as an adjunct in aiding video laryngoscope-assisted assessment of vocal cord movements at extubation following total thyroidectomy. Anesth Essays Res [serial online] 2019 [cited 2019 Jul 1];13:25-30.