Official Journals By StatPerson Publication
|
Table of Content - Volume 12 Issue 3 -December 2019
The effect of 0.6µg/kg body weight IV dexmedetomidine in the suppression of sympathoadrenal response to direct laryngoscopy and endotracheal intubation
Sindhu S1, V Y Srinivas2*
1Resident, 2Professor, Department of Anaesthesia, Mysore Medical College, Mysore, Karnataka, INDIA. Email: sindhusuresh1991@gmail.com
Abstract Background and Objective: Direct Laryngoscopy and endotracheal intubation following induction of general anaesthesia is associated with sympatho adrenal responses such as increase in heart rate, raise in systolic arterial, diastolic arterial and mean arterial blood pressure. This sympathoadrenal response may lead to deleterious effects in vulnerable subjects such as those with Hypertension, coronary artery disease and cerebral vascular disease. The present study aims to find out the effectiveness of 0.6µg per kg bodyweight of alpha 2 agonist Dexmedetomidine in suppression of the sympathoadrenal response to direct laryngoscopy and endotracheal intubation. Methodology: The study was conducted on 60 participants aged between 18 – 55 yrs belonging to ASA class one or two undergoing elective surgeries under endotracheal general anaesthesia. The study population was divided into two groups after randomization with 30 participants in each group. Group DEX(Dexmedetomidine) received Inj Dexmedetomidine 0.6mcg per kg body weight diluted to 10ml with normal saline intravenously. Group CT (Control) received 10ml of0.9 % normal saline intravenously. The study drug was administered over 10 minutes using syringe pump followed by induction with inj Thiopentone sodium 5mg / kg and inj vecuronium 0.1mg / kg three minutes before direct laryngoscopy and endotracheal intubation. HR(Heart rate), SBP(systolic arterial blood pressure), DBP(diastolic arterial blood pressure), MAP(mean arterial pressure) were recorded at basal, 2 minutes, 5 minutes, 8 minutes after study drug infusion, before induction, after induction and at intervals of 1minute, 2minutes, 3minutes, 5minutes, 8minutes, 10 minutes and 15 minutes following direct laryngoscopy and endotracheal intubation .Results and Analysis: After analysis of the results it was found that the patients who were administered dexmedetomidine had a statistically significant reduction in heartrate ,systolic and diastolic arterial blood pressure and mean arterial pressure compared to control group . Conclusion: From the findings of our study, it was found that the sympathoadrenal response to direct laryngoscopy followed by endotracheal intubation was suppressed with inj Dexmedetomidine 0.6µg/kg body weight compared to control group. Key Words: Dexmedetomidine, Laryngoscopy and Endotracheal intubation, Attenuation, Haemodynamic responses
INTRODUCTION In the year 1940 Reid and Brace1 made observations regarding the haemodynamic variations in relation to direct laryngoscopy and endotracheal intubation. The Direct laryngoscopy and endotracheal intubation induces an adrenergic response in the form of tachycardia, raise in blood pressure, intracranial and intraocular pressure2,3. Various pharmacological modalities such as lignocaine4, opioids5,6 sodium nitroprusside7, nitroglycerine8, calcium channel blockers.9,10 have been tried but had limitations. Dexmedetomidine shows the preferential affinity towards alpha 2 adrenoceptors. It has alpha 2: alpha 1 binding ratio of 1620:1. There are very few studies done in the past regarding the role of dexmedetomidine hence our study is being taken up to know the effectiveness of 0.6µg/kg body weight of Dexmedetomidine in suppression of cardiovascular system changes to laryngoscopy and intubation11-14.
METHODOLOGY The study was done at a teaching hospital Mysore. Permission was obtained from institute ethical committee. Informed consent was taken from each participant included in the study. A total of 60 participants were included, on preanaesthetic evaluation had a status of ASA grade 1 or ASA grade 2. All of them were in the age group 18- 55 yrs undergoing elective procedures with general anaesthesia and endotracheal intubation. Exclusion criteria for the study defined as patients with co-morbidities like heart disease, kidney disease, liver disease, cerebrovascular diseases and peripheral arterial disease, Hypertension, Bradycardia (<60bpm), hypotension SBP (<100 mmHg),heart block, difficult airway and obesity (BMI>30), Subjects with endocrine problems like thyroid disease and Diabetes Mellitus were also excluded. Among the sixty patients they were randomly assigned into two groups by using sealed envelopes. Envelopes were shuffled and each patient was asked to pick one of them, thus dividing them into two groups of thirty each.The selected envelope was checked by a senior anaesthetist who was not involved in the project and also prepared the drugs, hence blinding was done. Group CT – Control group – was administered 10ml of 0.9% normal saline i.v in 10minutes by a syringe pump 10minutes prior to induction. Group DEX – Dexmedetomidine group – were given injection0.6µg/kg Dexmedetomidine diluted in 10ml with 0.9%normal saline i.v in 10 minutes by using a syringe pump, 10minutes prior to induction. Premedication with tablet alprazolam 0.5mg and a H2 blocker Ranitidine 150mg given the day before surgery. All participants were advised nil per oral the day before surgery. The study subjects vital signs were monitored using a multi para moniter i.e pulse oximetry, Blood Pressure and electro cardiogram(ECG) . Before the study drug infusion heart rate, systolic arterial and diastolic arterial blood pressure and mean arterial pressure were recorded. Later subjects in group CT were administered 0.9% 10ml of normal saline i.v over 10minutes. Likewise subjects in group DEX was received Inj Dexmedetomidine 0.6µg/kg body weight diluted to 10ml of 0.9 %normal saline i.v over 10minutes. Premedication done by administration of inj.Midazolam 0.05mg/kg and inj. ondansetron 0.1mg/kg followed by preoxygenation for 3min with 100% oxygen. All the subjects were administered with 1.5mg/kg body weight of Lidocaine ninety seconds before intubation. All participants were induced with injection Thiopentone 5mg/kg body weight and injection vecuronium 0.1mg/kg body weight three minutes earlier to direct laryngoscopy and intubation followed by mask ventilation with mixture of 50% oxygen with 50% nitrous oxide and 0.6% isoflurane. Later the procedure of direct laryngoscopy and endotracheal intubation done, confirmed of equal air entry on both sides with ETCO2 monitor. Following which fixation of endotracheal tube done and ventilator was connected. Maintenance of general anaesthesia was done by inhalation of 50% nitrous oxide and 50% oxygen with 0.6% isoflurane followed by reversal with Inj neostigmine 0.05mg/kg along with Inj glycopyrrolate 0.01mg/kg after the completion of procedure. The variables like heart rate(HR) ,systolic arterial and diastolic arterial blood pressure(SBP and DBP) ,mean arterial pressure(MAP) were recorded at intervals of 2 minutes, 5minutes and 8 minutes following study drug administration ,prior to and after induction and at intervals of 1minute, 2 minutes, 3minutes, 5minutes 8minutes 10minutes and 15 minutes after direct laryngoscopy and endotracheal intubation. STATISTICAL METHODS The calculation of sample size was done after discussion with the statistician, on the basis of pilot study observations. The observation conducted showed approximately each group should have 23 patients for ensuring a power of study 0.80 for detecting clinically significant variation of 15% in heart rate and mean arterial blood pressure. Assuming of 5% patients drop out, the sample size was calculated at 30 patients in each of the group, allowing a type 1 alpha error =0.05 and a type 2 error of beta=0.2 and power of 0.8. All the statistical methods were carried out through Microsoft excel SPSS for Windows (version 20.0) The study data in the two groups was analysed using descriptive statistics and inferential statistics i.e crosstabs and repeated measure Analysis of Variance (ANOVA) test. A ‘p’ Value < 0.05 was taken as statistically significant and <0.01 was considered as highly significant. RESULTS There was no statistically significant difference in demographics variables like meanage, sex, weight in between study groups. After statistical analysis, the difference in the duration of direct laryngoscopy and endotracheal intubation was statistically insignificant in between two groups.
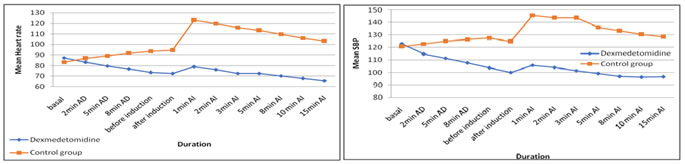
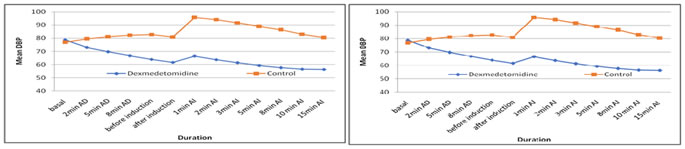
HEART RATE After applying the statistical tests, we found that the difference in the baseline mean heart between Group DEX and Group CT and was statistically insignificant (p = 0.12). After the administration of Dexmedetomidine the difference in the reduction in mean Heart rate response was found statistically highly significant(p=0.00) at certain time intervals such as 2nd, 5th, 8th minute after study drug infusion, before induction, after induction, 1st, 2nd, 3rd, 5th,8th 10th and 15th minute after doing direct laryngoscopy and endotracheal intubation compared to control group. We found that mean Heart rate reading in Group CT was increased i.e. 40bpm compared to baseline at 1st minute following direct laryngoscopy and endotracheal intubation, also followed by a sustained rise in mean Heart rate recording which did not touch the baseline value 15th minute. The maximum variation in the mean heart rate was observed in the Dexmedetomidine group at 1st minute after direct laryngoscopy and endotracheal intubation i.e lowering of mean heart rate by 8bpm compared to baseline reading. Next measurements as per the study protocol demonstrated that mean heart rate was lower than the baseline at various study time intervals and was found to be statistically highly significant(p=0.00).
Figure 1 Figure 2 Figure 3 Figure 4 Figure 1: Graph showing the intergroup comparison of mean Heart Rate (bpm) betweenDexmedetomidine and Control group at various time intervals during the study; Figure 2: Graph representing the intergroup comparison of mean Systolic Blood Pressure (mm Hg) among Dexmedetomidine group (group DEX) and Control group (group CT) at various time intervals during the study; Figure 3: Graph showing the intergroup comparison of mean Diastolic arterial Blood Pressure (mm Hg) among Dexmedetomidine group and Control group at different time intervals during the study; Figure 4: Graph showing the intergroup comparision of Mean Arterial Pressure (mm Hg) between Dexmedetomidine group and Control group at various time intervals during the study.
SYSTOLIC ARTERIAL BLOOD PRESSURE From our study results we found that the baseline Systolic arterial blood pressure was statistically insignificant (p=0.15) between the group DEX and group CT. On analysis of the test results of systolic arterial blood pressure between the group DEX and group CT We found a difference at 2nd,5th,8th minute after drug infusion, before induction, after induction, 1st,2nd,3rd,5th,8th,10th and 15th minute following direct laryngoscopy and endotracheal intubation which was highly significant statistically . Group DEX showed a better decrease in mean systolic arterial blood pressure compared to group CT. Further, the study found that increase of mean Systolic BP 1 minute after the procedure of direct laryngoscopy and endotracheal intubation of 25mmHg in Group CT, but it reached the baseline at 15th minute following the procedure. Where as in Group DEX, we found a statistically significant(p=0.00) fall in mean systolic BP of 17mmHg at 1 minute after procedure of laryngoscopy and intubation, also it remained below the basal value at all study time intervals DIASTOLIC ARTERIAL BLOOD PRESSURE Our study found that the difference in mean Diastolic arterial Blood pressure of baseline and 2 minutes after administration of study drug was statistically insignificant between the group DEX and group CT. The lowering of mean Diastolic arterial blood pressure was significant statistically following drug infusion at 5th minute and further application of the tests results after 8th minute, after administration of study drug, prior to induction, after induction, 1st, 2nd, 3rd, 5th, 8th, 10th and 15th minute following direct laryngoscopy and endotracheal intubation showed reduction in mean Diastolic arterial blood pressure in dexmedetomidine group compared to control group which was highly significant statistically. The highest rise of about 18mmHg in mean Diastolic arterial Blood pressure was recorded in Group CT 1 minute after direct laryngoscopy and endotracheal intubation in relation to the baseline later after 15 minute it almost reached the baseline. Whereas in Group DEX, comparatively a fall in mean diastolic arterial Blood Pressure of 12mmHg in mean after 1 minute of direct laryngoscopy and endotracheal intubation, further Diastolic arterial blood pressure was remained below the baseline at various study time intervals which was found to be highly significant statistically(p=0.00). MEAN ARTERIAL PRESSURE Our study results showed that the baseline mean arterial blood pressure was statistically insignificant between the two groups group DEX and group CT. The lowering of mean arterial pressure at 2nd, 5th, 8th minute after study drug infusion, before induction, after induction, 1st, 2nd, 3rd, 5th, 8th, 10th and 15th minute following direct laryngoscopy and endotracheal intubation in Group DEX was highly significant statistically (p=0.00) compared to Group CT. From our study it was showed that the group CT showed a raise of about 20mmHg in mean arterial pressure compared to baseline at 1 minute following direct laryngoscopy and endotracheal intubation and almost reached the baseline value at 15th minutes later. On the other hand in Group DEX, results showed a decrease in mean arterial pressure by 14mmHg following direct laryngoscopy and intubation at 1st minute in relation to baseline value and it remained lower than the baseline value at various study time intervals which was highly significant statistically (p=0.00).
DISCUSSION Direct laryngoscopy and endotracheal intubation is a noxious stimuli which leads to transient but marked haemodynamic response in the form of tachycardia and hypertension. These responses can cause hazardous consequences like cardiac failure, ischemic myocardium, abnormalities in cardiac rhythm and cerebral hemorrhage in patients with increased blood pressure, cardiac and cerebrovascular disease .15-17 Earlier many methods used such as volatile anaesthetic agents, Xylocaine4 ,narcotic agents5,6direct acting vasodilator7,8calcium channel inhibitors9,10have been tried to decrease the haemodynamic variation to direct laryngoscopy and endotracheal intubation, but had their own disadvantages. Dexmedetomidine emerged as a drug to suppress the sympathoadrenal response to direct laryngoscopy and endotracheal lintubation discovered in various newer studies. Dexmedetomidine a second-generation alpha-2 adrenergic receptor agonist. The food and drug administration (FDA) approved the use of Dexmedetomidine as an ICU sedative in 199918. Dexmedetomidine has a highly preferential affinity towards alpha -2 receptors and has a high ratio of alpha-2/alpha-1 activity (1620:1 as compared to 220:1 for clonidine) and thus has predominant action on alpha-2 adrenoceptor. This ratio is responsible for its potent action on the central nervous system and avoids undesirable effects on cardiovascular system by alpha-1 receptor activation19. it causes Sedation and Analgesia, hypnosis, anxiolysis.20. Depending upon the dose of Dexmedetomidine administered, it leads to a reduction in cardiac rate , systolic and diastolic arterial blood pressure 19. HEART RATE In the difference in baseline mean heart rate between Dexmedetomidine and Control groups was found to be statistically insignificant. Upon giving Dexmedetomidine 0.6mcg/kg showed a fall in mean heart response at 2 minutes, 5 minutes, 8 minutes following drug infusion, before induction, after induction at , 2 minutes, 3, minutes, 5minutes, 8 minutes, 10 minutes and 15 minutes after laryngoscopy and intubation in comparison to the Control group which was statistically highly significant(p=0.00). A decrease in mean heart rate by 8 bpm was observed in Dexmedetomidine group in comparison to baseline in group DEX at 1st minute after direct laryngoscopy and endotracheal intubation whereas, a raise in mean heart rate by 40 bpm in relation to baseline was observed in Group CT and that was found to be highly significant statistically . The similar trend in heart rate response was found in studies done by Scheinin et al21, Jaakola et al22,Basar et al23Kunisawa et al24, Ferdi et al25 and Keniya et al26. SYSTOLIC ARTERIAL BLOOD PRESSURE Between the group DEX and group CT, the difference in baseline mean systolic arterial blood pressure was statistically insignificant. Our results showed a fall in mean Systolic blood pressure upon infusion of Dexmedetomidine at 2nd, 5th, 8th minute after study drug, before induction, following induction and at 2nd,3rd,5th,8th ,10th and 15th minute after direct laryngoscopy and endotracheal intubation in comparison to Control group which was statistically highly significant(p=0.00). This results were in par with the studies done by Jaakola et al22, Sharma AN et al28, Reddy SV et al29, Kewalramani et al30, El - Shmaa et al11 .In Dexmedetomidine group, we found a statistically highly significant (p=0.00) fall of mean Systolic blood pressure of 17 mm Hgin comparison to baseline at 1st minute after direct laryngoscopy and endotracheal intubation and the mean Systolic arterial blood pressure was below the baseline value even at 15th minute after direct laryngoscopy and endotracheal intubation. The greatest rise of about 25 mmhg in mean Systolic arterial blood pressure was observed after direct laryngoscopy and endotracheal intubation at 1st minute and the mean systolic arterial blood pressure approached the baseline value at 15th minute in control group. Thus, in comparison to control group Dexmedetomidine was found to be better in the attenuation of the systolic arterial blood pressure at various time intervals which was highly significant statistically(p=0.00). This correlates with studies done by Jaakola et al22,Kunisawa et al24, Srivastava VK et al31, Rashmi HD et al32, Kewalramani et al30, El-Shmaa et al11 . DIASTOLIC ARTERIAL BLOOD PRESSURE There was a statistically insignificant difference between the group DEX and group CT with reference to the baseline value. The decrease in mean Diastolic arterial blood pressure after administration of Dexmedetomidine at 5th minute and at 8th minute after study drug, before induction and after induction significant statistically compared to Control group. This findings were similar to the studies done by Sharma AN et al28, Reddy SV et al29, Kewalramani et al30, El-Shmaa et al11 .A decrease of about 12mmHg in mean diastolic arterial pressure was found in group Dex where as a greatest increase of about 18mmhg in mean diastolic arterial blood pressure was found in group CT after direct laryngoscopy and endotracheal intubation at 1st minute with reference to the baseline value. Hence Dexmedetomidine was preferentially more effective in attenuating the Diastolic blood pressure response at 1st minute after direct laryngoscopy and endotracheal intubation compared to Control group which was statistically highly significant(p=0.00) . This correlates with the studies such as Jaakola et al22, Kunisawa et al24, Ferdi et al25, Reddy SV et al29, Srivatsava VK et al31, Rashmi HD et al32, Kewalramani et al30, El-Shmaa et al11. In our study, the fall in mean Diastolic arterial blood pressure in Dexmedetomidine group at 2nd, 3rd, 5th, 8th, 10th and 15th minute after direct laryngoscopy and endotracheal intubation was statistically highly significant(p=0.00) compared to Control group. In group CT the mean diastolic arterial pressure had approached the basal value at 15th minute after direct laryngoscopy and endotracheal intubation whereas in group DEX the mean Diastolic arterial blood pressure had remained below the basal value even at 15th minute after intubation . This correlates with the Jaakola et al22, Kunisawa et al24, Ferdi et al25, Reddy SV et al29, Rashmi HD et al32, Kewalramani et al30 and El- Shmaa et al11 studies. MEAN ARTERIAL BLOOD PRESSURE The basal mean arterial blood pressure difference was statistically insignificant in between the group DEX and group CT. The fall in Mean arterial pressure in group DEX at 2nd, 5th, 8th minute after drug infusion, before induction and after induction was highly significant statistically compared to control group. Our study findings validate with the findings of Kewalramani et al30 and El-Shmaa et al11 studies. At 1st minute following direct laryngoscopy and endotracheal intubation, a fall of about 14mmHg in mean arterial pressure was noted in group DEX whereas a highest increase of about 20mmhg in mean arterial pressure was noted in control group when compared to basal value. hence, Dexmedetomidine was effectively suppressed the increase in mean arterial pressure at 1st minute after the procedure compared to Control group which was statistically highly significant in our study. Our findings validate with the findings of Reddy SV et al29, Srivatsava VK et al31, Rashmi HD et al32, Kewalramani et al30, El-Shmaa et al11 studies. The fall in mean arterial pressure at 2nd, 3rd, 5th, 8th, 10thand 15th minute following direct laryngoscopy and endotracheal intubation in group DEX was highly significant(p=0.00) statistically in comparison to group CT . In group DEX, the mean arterial pressure remained lesser the basal value even 15minutes after direct laryngoscopy and endotracheal intubation. In group CT, the mean arterial pressure had reached the basal value at 15th minute after laryngoscopy and intubation. The findings of our study showed similarity with other studies conducted by Reddy SV et al29, Srivatsava VK et al31, Kewalramani et al30, El-Shmaa et al11, Rashmi HD et al32studies.
CONCLUSION Administration of one dose of Injection Dexmedetomidine 0.6µg/kg body weightover 10 minutes intravenous 10 minutes before induction showed a significant suppression of the sympathoadrenal response to direct laryngoscopy and endotracheal intubation .
REFERENCES
|
|
 Home
Home