|
Table of Content - Volume 13 Issue 2 -February 2020
Evaluation of anaesthetic techniques for surgery of upper extremities
Koj Jarbo1, Keya Chakraborty 2*, Dhrubajyoti Sarkar3, Pratap B Kaushik4
1,3Senior Specialist, Professor and Head, Department of Anaesthesiology, Tomo Riba Institute of Health and Medical Science (TRIHMS), Naharlagun, Arunachal Pradesh, INDIA. 2Assistant Professor, Department of Anaesthesiology, Ramakrishna Mission Seva Pratisthan and Vivekananda Institute of Medical Sciences, Kolkata, West Bengal, India 4Lecturer-Statistics, Department of PSM, RNT Medical College, Udaipur, Rajasthan, India.
Abstract Background: The anaesthetic technique used in surgeries of upper extremities is determined by factors such as urgency, presence of coexisting health problems, preference of patient, availability of equipments and drugs, preference and experience of the anaesthetist and surgeon. Methods: This is a retrospective study of all the upper extremity surgeries requiring anaesthesia services that occurred in the period between 1st October, 2014 to 30th September, 2019 in the department of Anaesthesiology, TRIHMS, Naharlagun, Arunachal Pradesh, India. The anaesthesia techniques used for surgeries of upper extremities were evaluated in this study. Anaesthesia methods were recorded as general anaesthesia (GA) and regional anaesthesia (RA). General anaesthsia was classified into GA with Endotracheal Intubation, GA with LMA and GA with Face Mask and RA was classified into Brachial Plexus block (Inter-scalene, Supraclavicular, Infraclavicular or Axillary), Intravenous Regional Anaesthesia ( Bier Block ) and Distal Nerve Block subgroups. RA groups were further categorized into those performed with and without the use of aids such as Ultrsound or Nerve stimulator. Results: During the study period, a total of 771 patients, 498 male and 273 female, underwent surgeries for upper extremity. The commonest site operated upon was forearm. The most frequently employed anaesthetic technique during the total study period was general anaesthesia (73.8%). In the first 3 years of the study period, all the patients received GA (100%), and in the 5th year, the usage of RA jumped to 175 (67.56%). All the RAs were performed with the aid of Ultrasound. The most commonly performed RA was Supraclavicular Brachial Plexus Block. Conclusions: In recent years, regional anaesthesia administration in surgery of upper extremities is gradually increasing, and Supraclavicular brachial plexus block is the most frequently performed regional anaesthesia. There may be a need to explore the use of other forms of regional anaesthesia. Keywords: Upper extremity surgery, General anaesthesia, Regional anaesthesia, USG-guided nerve block.
INTRODUCTION General Anaesthesia (GA) and Regional Anaesthesia (RA) have been successfully used for upper extremity surgeries1,2. In the past, general anaesthesia was frequently the method of choice for upper extremity surgery due to lack of training and experience in the field of regional anaesthesia as well as fear of complications including vascular puncture, local anaesthetic toxicity, pneumothorax, and patient discomfort 3. However, the advantages of GA, including control of airway and the familiarity of the technique by the majority of anaesthesiologists are overshadowed by clear benefits of regional anaesthesia, which includes intra operative as well as postoperative analgesia, excellent muscle relaxation during surgery, decreased opioid requirements, greater haemodynamic stability, increased efficiency in the operating room, decreased Postoperative Nausea and Vomiting (PONV), reduced Post Anaesthetic Care Unit (PACU) stay, decrease in unplanned hospital admission for pain control, as well as greater patient satisfaction 4, 5. RA is particularly desirable and effective in elderly and high-risk patients undergoing upper and lower extremity surgeries 6. The use of electrical nerve stimulation to locate peripheral nerves was introduced in 1962 7. Several advantages have been attributed to this technique, including a higher success rate, the avoidance of vascular injury and paresthesias, and associated neurological injuries 8-10. The use of a Peripheral Nerve Stimulator (PNS) has been the ‘gold standard’ for performing peripheral nerve blocks for the last two decades. However, with the recent developments in high-frequency imaging, the use of Ultrasound (US) technology has significantly increased for nerve localization 11,12. The US-guided technique offers reported additional advantages, including avoidance of intraneural/intravascular injection, decrease in dose and volume of local anaesthetics, faster onset time, improved block quality, decreased pain from muscular contractions, prolonged postoperative analgesia, and decreased need for rescue analgesics 13-15. In this study, we compiled and evaluated the various kinds of anaesthetic techniques practiced for upper extremity surgeries in the past 5 years at Tomo Riba Institute of Health and Medical Sciences (TRIHMS), Arunachal Pradesh, India.
METHODS After obtaining approval from the institutional ethics committee, all the patients who underwent upper extremity surgeries during the study period were included. This is a retrospective study of all the anaesthetic technique performed for upper extremity surgeries over a period of 5 year period between 1st October, 2014 to 30st September, 2019 in the department of Anaesthesiology, TRIHMS Hospital, Naharlagun, Arunachal Pradesh, India. Data were collected and analyzed from the Operation Theatre Record Books. Data collected included the age and sex of the patients, indication and the surgery performed. Anaesthesia techniques were recorded as GA, RA, and combined RA with GA. GA was further classified into GA with Endotracheal intubation (ETT), GA with LMA and GA with face mask, RA was further classified into Interscalene Brachial plexus block (ISB), Supraclavicular Brachial plexus block (SCBPB), Axillary Brachial plexus block (AXBPB), Suprascapular nerve block (SSNB), wrist block (WB), Radial and Ulnar nerve block (RUNB) and Intravenous Regional Anaesthesia (Bier Block). Regional Anaesthesia groups were further categorized into those performed with and without the use of aids such as Ultrasound or Nerve stimulator. The various anaesthetic techniques used for upper extremity surgeries were grouped and recorded year wise for evaluation. Descriptive statistics were presented as patient number and percentages (%) for nominal variables. Statistical analysis has been done using EPI INFO-7 Software and by chi-squared test, p-value of less than 0.05 is considered to be significant.
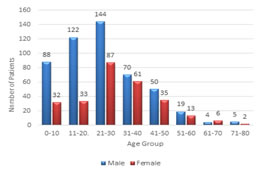
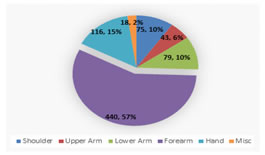
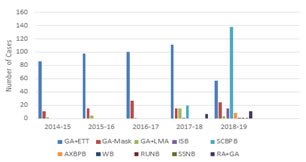
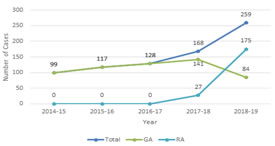
RESULTS During the study period, a total of 771 patients 498 male and 273 female, underwent upper extremity surgeries: 99, 117, 128,168 and 259 patients in the first, second, third, fourth and fifth year of the study period respectively. The demographic profile of the patients according to age and sex are as shown in the Figure-1. Analysis shows that the maximum number of patients belonged to the age group of 21-30 years of age 231 (29.96%) and the males (65.1%), with a M:F =1.86:1, outnumbered females across almost all age groups. The distribution of cases as per the indication for and site of surgeries are as shown in Figure-2. Analysis shows that forearm was the most frequently operated site 440 (57%) followed by shoulder 116(15%). Of the total 771, 569 (73.8%) patients received GA, 184 (23.86%) patients received RA or distal nerve blocks, and 18 (2.33%) patients received combined GA/Sedation and RA. The year wise breakdown of the anaesthetic techniques employed (Figure. 3 and Table 1) shows that in the first 3 years of the study period all the patients were given GA, maximum being the GA with endotracheal tube intubation and the least being GA with LMA. In the year 2017-18, of the total of 168 patients, 141 (83.93%), 20 (11.9%), and 7 (4.2%) patients received GA, RA and RA combined with GA respectively. And, in the year 2018-19, of the 259 patients who underwent upper extremity surgeries, only 84 (32.43%) patients were provided GA, whereas, 163 (62.93%) patients received RA in the form of Brachial Plexus Block (ISB, SCBPB, AXBPB, SSNB, WB) and 1 (0.38%) patient was given distal nerve block (RUNB). The remaining 11(4.24%) patients also received RA, but they required supplementation with Sedation/GA. Among the RA techniques the most frequently performed RA is Supraclavicular Brachial Plexus Block, which comprised 19 (70.37%) in the year 2017-18 and 138 (78.85%) in the year 2018-19. All the RA were performed under sono-guidance. It has been observed that in the last two years, the number of cases gradually increased and there is a significant (p-value <0.001) increase in the practice of regional anaesthesia with decrease in the practice of General anaesthesia (Figure-4 and Table-2). Figure 1: Distribution of Patients According to Age and Sex Figure 2: Distribution of Cases Figure 3: Distribution of Type of Anaesthesia Figure 4: Technique of Anaesthesia and Number of Cases
Table 1: Different Techniques of GA and RA practiced
Table 2: Trend of Anaesthesia Technique
DISCUSSION Nerve block anaesthesia being cheaper than GA has many advantages such as anaesthesia targeted at the operative site, excellent postoperative pain relief, decreased opioid use and reduced recovery time [16,17]. Obasuyi BI et al reported a predominant use of GA (84%) for upper extremity surgeries, which is comparable with our observation made in the initial three years of the study, wherein GA (100%) was the only technique of choice, but on the contrary, in the last two years of our study the practice of RA was significantly high (16.07% and 67.56% respectively) [18]. Patel AA et al reported in their study that of all the upper limb surgeries, 20% are performed under peripheral nerve block and 80% are performed under general anaesthesia, which is comparable with our observation made in the year 2017-18 with GA 83.93%, RA 16.1% of which 7 (4.2%) patients received RA combined with GA [19]. But the same is not comparable with our observation made in the year 2018-19, wherein 67.56% were provided RA and only 32.43% patients were provided GA. This may be due to their multicentic and total study duration data analysis effect and availability of equipment can be an added issue. Schnittger T et al and Rukewe A et al reported low utilisation of regional anaesthesia and peripheral nerve blocks and have blamed on deficiencies of training, equipments and drugs, which is comparable with our observation of the initial three years [20,21].In our study, it is observed that the annual total number of upper extremity surgical cases have steadily increased from 99 patients in the year 2014-15 to 259 patients in the year 2018-19. This may be ascribed to progressive availability of better services and upgradation of our centre, compounded by increase in population. Our study showed that both GA and RA provided effective surgical anaesthesia for upper extremity surgical procedures, irrespective of the location or complexity of surgery for all the 771 patients studied. Regional anaesthesia when used as a sole technique or in conjunction with GA proved adequate for surgery in our study population. In our study, all the patients in the first 3 years of the study period received GA, and none were provided RA. In the year 2017-18, the usage of RA rose to 16.07% from 0% in the preceding 3 years, and in the year 2018-19, it further increased to 67.56%, thus indicating a significant change in the practice of anaesthetic techniques for upper extremity surgeries. This change in the trend of practice of anaesthetic techniques may be ascribed to the availability of necessary resource person, training, drugs and equipments during the period of beginning and progressive increase in the usage of RA. Availability of ultrasound with proper training promotes the practice of regional anaesthesia safely for surgeries of upper extremities. CONCLUSION: The use of RA for upper extremity surgery is steadily increasing in the recent years which is a positive development in a resource limited setting, and the most commonly RA technique employed is USG-guided Supraclavicular Brachial Plexus Block. There is a need to explore and encourage the use of other forms of regional anaesthesia also for upper extremity surgery.
REFERENCES
Policy for Articles with Open Access
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home