|
Table of Content - Volume 13 Issue 2 -February 2020
Comparison of anesthetic effect of ropivacaine with dexmedetomidine and clonidine in patients undergoing lower limb surgery: A prospective study
Ravishankar V1, Sathesh Kumar BM2*
1Assistant Professor, Department of Anesthesiology, Sree Mookambika Institute of Medical Sciences, Kulasekharam, Tamil Nadu, INDIA. 2Senior Resident, Department of Anesthesiology, CMC, Vellore, Tamil Nadu, INDIA. Email: drshankar278@gmail.com
Abstract Background: Epidural anesthesia is one of the major methods of anesthesia to induce analgesic and anesthesia effect before surgery. Local anesthetics are injected into the epidural space after identifying it by touys needle. Adjuvants are often added to the local anesthetics in this technique to attain faster effect. The anesthetic effect depends on the combination used. The present study aimed to evaluate the anesthetic effect ropivacaine with dexmedetomidine and clonidine in patients undergoing lower limb surgery. Materials and Methods: Total of 70 patients were included in this study on the basis of inclusion and exclusion criteria. All the patients were explained about the study protocol and informed consent was obtained. 70 selected patients were divided into two groups each of 35. In G-I (Ropivacaine (0.75%/15 ml)+ Dexmedetomidine (1 mcg/kg) and G-II Ropivacaine (0.75%/15 ml)+Clonidine (1 mcg/kg) were administered epidurally before starting the surgery. All patients demographic, ASA scale, co morbid conditions, time to onset of sensory and motor block were noted and compared. Results: Males were more in both groups compared to females. Mean age was more in group-II compared to group-I. Mean weight and height is more in group-I compared to group-II. Group-I had more of ASA grade-1 patients when compared to group-II. Significant difference observed in anesthetic efficacyin group-I compared with group-II. 31 patients had a sensory blockage of T6 and above in group 1 whereas only 23 had blockage of T6 and above in group 2. Mean motor block not showed any significant difference between the groups. Conclusion: The study results conclude that the addition of 1mcg/kg dexmedetomidine as an adjuvant to 0.75% ropivacaine in epidural anesthesia causes an early onset and prolonged duration of sensory analgesia. Key Word: Anesthesia, epidural, dexmedetomidine, ropivacaine, motor block, clonidine
INTRODUCTION Epidural anaesthesia is a versatile technique used for providing both anaesthesia and analgesia in the post operative period. It may be combined with other forms of regional anaesthesia or general anaesthesia. It provides intra operative hemodynamic stability and has been proven to reduce perioperative stress response thus causing a decrease in the complications and help in improving patient outcome. It also helps in early mobilization of the patient by providing relief to post operative pain and decreases the incidence of thromboembolic events.1-3 Epidural anaesthesia using bupivacaine has been researched in detail in the past. In the recent years ropivacaine is being used increasingly due to similar analgesic properties but with lesser motor blockade and cardio toxicity. A slightly larger dose of ropivacaine is required when compared to bupivacaine but the addition of an adjuvant helps in reducing the total dose required for local anaesthesia and adjuvant also enhances the efficacy, thereby increasing the duration of action and the intensity of blockade4,5 A number of agents such as opioids, ketamine, and alpha agonists can be used as adjuvants to local anaesthetics that act synergistically thereby increasing the efficacy of the local anaesthetic drugs, decreasing the total required dose and toxic side effects of both groups of drugs.6,7]The duration and the quality of analgesia can be improved when a local anaesthetic is combined with an alpha 2 adrenergic agonist as adjuvant. Both dexmedetomidine and clonidine are alpha 2 adrenergic agonists potentiates local anaesthetic effects and have analgesic properties. Clonidine is an alpha 2 adrenergic agonist that enhances the action of local anaesthetic drugs on administration via the epidural or intrathecal route. It acts by blocking the A and c fibres and it causes local vasoconstriction thereby decreasing the intensity and duration of analgesia. It is known to cause sedation and the side effects of its use are bradycardia and hypotension8. Dexmedetomidine is a newer alpha 2 adrenergic agonist and is about 8 times more selective a2 adrenoreceptor agonist than clonidine and hence allows the use of higher drug dosage with less alpha1 effect. It has been found to have hemodynamic stability, anxiolytic, analgesic, sedative, neuroprotective and anaesthetic sparing effect. It causes intense motor blockade and co-operative sedation without increasing the incidence of the adverse effects9. Clonidine and Dexmedetomidine act on both pre and post synaptic sympathetic nerve terminals and also has central action which causes a decrease in the sympathetic outflow, leading to its analgesic, sedative, and hemodynamic effects 10. The effects of clonidine as an adjuvant with local anaesthetics have been studied extensively and it effectively prolongs the duration of action of the local anaesthetics when given epidurally. The aim of our study was to compare the effect of Clonidine versus Dexmedetomidine when given as an adjuvant to Ropivacaine in epidural anaesthesia for lower abdominal and lower limb surgeries.
MATERIALS AND METHODS Study settings: This study was conducted in the Department of anesthesiology, SreeMookambika Institute of Medical Sciences, Kulasekharam, Kanyakumri (Dist), Tamil Nadu. The study period was one year.
Inclusion criteria
Exclusion criteria
Groups Group-I: Ropivacaine (0.75%/15 ml)+ Dexmedetomidine (1 mcg/kg) Group-II: Ropivacaine (0.75%/15 ml)+ Clonidine (1 mcg/kg) Procedure: After approval of the study protocol by our Institutional Human Ethics Committee, written informed consent was taken from each patient. ASA status I and II patients of either sex, aged between 18-65 years, weighing 50-70kgs, undergoing lower limb or lower abdominal surgery under epidural anaesthesia enrolled in this study. All the patients visited on the day prior to surgery, explained in detail about the anaesthetic procedure and informed written consent was obtained. The patients were kept nil orally 6hrs prior to the day of surgery. On arrival to the operation theatre, following insertion of an 18-G venous cannula, 500mL of Ringer Lactate was infused to the patient before epidural anaesthesia. Standard monitors like ECG, Non-invasive blood Pressure and SpO₂probe was attached and baseline parameters recorded. Inj. Ranitidine 50mg i.v and Inj. Metoclopramide 10mg slow i.v half an hour before the surgery. Group I was given Dexmedetomidine 1mcg/kg with ropivacaineepidurally, whereas Group II was given 1mcg/kg of clonidine with ropivacineepidurally. Patients were positioned and 15ml 0.75% ropivacainewith adjuvant was administered epidurallyin L3-L4 interspace through a standard midline approach using a 18-G tuohy needle and all patients were supplemented with oxygen - 4L/min via a face mask throughout the procedure after positioning the patient. Sensory block was assessed using sterile pin prick method in the mid-axillary line on both sides of the chest, motor block was assessed using a modified Bromage scale (grade 0⇾ no paralysis; grade I⇾ unable to raise extended leg; grade 2⇾ unable to flex the knee, grade 3⇾ unable to flex the ankle). Sensory and motor block was assessed every minute for the first 10mins and thereafter every 10mins during the surgery and every 15mins postoperatively and be recorded. The highest dermatome level of sensory blockade and motor blockade were recorded. Recovery time for the sensory blockade is considered as two dermatome regression of anaesthesia from the maximum level; motor block duration is the time to return to grade 1on the modified Bromage scale. Postoperative pain was assessed by using the Visual Analog Scale (VAS 0 ⇾ no pain and VAS 10 ⇾ worst possible pain) at 4, 8, 12 and 24 hour. Patients with a VAS score of 3 or more was given Inj. Tramadol 50mg slow i.v. The time of patient’s first request for postoperative analgesia after the surgery was recorded as duration of postoperative analgesia. Statistical analysis: Statistical Package for Social Sciences (16.0) version used for analysis. The data was expressed in number, percentage, mean and standard deviation. Unpaired t test applied to find the statistical significant between the groups. p value less than 0.05 (p<0.05) consider statically significant at 95% confidence interval.
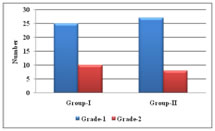
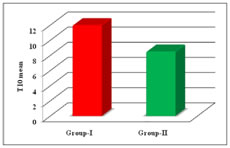
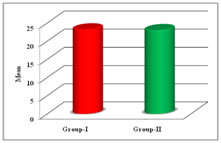
RESULTS This study included 70 patients were divided into two groups. Group-I had more males compared to group-II but females were more in group-II compared to group-I. Group-II showed more mean age compared to group-I. 61.14 kg was mean age of group-I which is higher than group-I 58.63kg. Mean high was more in group-I compared to group-II (table-1). Grade-1 ASA was more in group-II compared to group-II. In group-I had more grade-2 ASA score compared to group-I (Graph-1). In group-I more patients were undergoing HER compared to group-II. 12 patients in group-I and 15 in group-II undergone VH surgery (Table-2). Group-I showed significant efficacy compared to group-II in T6 and above blockage (Graph-2). In group-I 3 patients showed T5 block compared to group-II where only 2 had. 28 in group-I and 21 patients in group-II showed T6 block. 4 in group-I and 12 in group-II showed T8 block (Table-3). Motor block of nerves in both groups showed similar effect which was not statically significant (Graph-3). Group-II significant duration of blockade and dermatome compared to group-I. Blockade and dermatome regression between the groups showed significant difference (p<0.001) (Table-4). Table 1: Comparison of demographic data of the patients between group-I and group-II
Figure 1: Distribution of patients based on ASA physical status between group-I and group-II
Table 2: Distribution of patients based on type and duration of surgery between group-I and group-II
Figure 2: Comparison of efficacy of the drugs between group-I and group-II
Table 3: Comparison of sensory blockade between group-I and group-II
(*p<0.05 significant compared Group-I with Group-II)
Figure 3: Comparison of mean motor blockage between group-I and group-II Table 4: Comparison of mean duration of blockade, dermatome regression between group-I and group-II
(*p<0.05 significant compared Group-I with Group-II) DISCUSSION Epidural anaesthesia is considered as a gold standard technique as it provides complete, dynamic anesthesia and post operative analgesia. The benefits include suppression of stress response by sympatholysis, stable hemodynamics with reduction in cardiac morbidity, reduction in pulmonary complications due to active physiotherapy and early mobilization, reduced blood loss and decrease in thromboembolic complications following surgery. Chandran S et al compared the characteristics of 0.75% Ropivacaine and 0.5% bupivacaine and concluded that ropivacaine and bupivacaine at these doses produced equally effective anesthesia. 0.75% ropivacaine produce adequate intensity of motor and sensory blockade and its comparable to 0.5% Bupivacaine with reduced side effects. Hence we used 0.75% Ropivacaine to provide epidural anesthesia11. Dexmedetomidine is known to have eight times more affinity than clonidine for alpha adrenergic receptors, however there are no studies documenting the equivalent doses of epidural dexmedetomidine and clonidine12-14. A number of studies have used epidural clonidine at doses of 1-4mcg/kg,and it has been noted that the hemodynamic side effect are dose dependent. It has been suggested that epidural clonidine at a dose 1mcg/kg prolongs analgesia without producing unwanted side effects. Epidural dexmedetomidine has been studied at doses ranging from 1-2mcg/kg and it was observed that at doses less than 1mcg/kg dexmedetomidine does not prolong the block of ropivacaine. Hence in our study, we have used equal concentration of 1mcg/kg of clonidine and dexmedetomidine as an adjuvant to ropivacaine in epidural anesthesia. In this study, we compared two alpha agonists-clonidine and dexmedetomidine with 0.75% ropivacaine in the epidural route for lower abdominal and lower limb surgeries. The study was conducted in 70 patients between the ages of 18 to 65 years who were randomly assigned into two groups. Group RD received 15ml f 0.75% Ropivacaine with 1mcg/kg of dexmedtomedine and group RC received 15ml of 0.75% Ropivacaine with 1mcg/kg of clonodine, both groups received a total volume of 16ml.The demographies of both groups were found to be comparable with respect to age, gender, height, weight and surgery duration as there was no statistically significant difference(p>0.05). Our study showed significantly earlier onset of sensory blockade in the patient receiving dexmedetomidine (8.53±1.81minutes) when compared to the patients receiving clonidine (11.93±1.96 minutes). There was significantly higher dermatomal spread in group RD. this findings was consistent with the previous observations made by Bajwa et al, who found that the onset of sensory analgesia at T10 was faster in the group receiving dexmedetomidine (8.52±2.36min) when Compared to ten patients receiving clonidine (9.72±3.44min) and there was also associated with a faster and higher level of sensory blockade. It has been observed that when dexmedetomidine is administrated epidurally it reaches a maximum concentration in the CSF within 5minutes with a distribution half life of 0.7 minutes. There is a dose dependent anti nociceptive effect of epidural dexmedetomidine which has been associated to its affinity for the alpha 2 receptors on the spinal cord. Dexmedetomidine also has higher lipid solubility in comparison to clonidine. This may be the probable cause for the enhanced potency of epidural dexdemetomidine over clonidine8. In this study we found that the duration on sensory analgesia was more in group RD (316±31.15minutes) than group RC (281±37minutes) which was statistically significant (p=0.000). In the study done by Sukminder Jit Singh Bajwa et al, they found a significantly longer time to first rescue top up in the dexmedetomidine group (342.88±29.16minutes) than the clonidine group (310.76±23.76 minutes)15. This may be because they had also used onset of incisional pain to indicate analgesia time, however the higher doses of dexmedetomidine (1.5mcg/kg) and clonidine (2mcg/kg) may be considered to explain the prolonged duration in comparison to our study. We found no statistically significant difference time to complete motor blockade, between the two groups, group RD in 23.00±4.27 minutes and group RC in 23.07±4.63 minutes). Bajwa et al found that patients receiving dexmedetomidne (17.24± 5.16minutes) achieved grade 3 motor blockade in less time than those receiving clonidine (19.52 ± 4.06) as an adjuvant15. This may be attributed to the larger doses of dexmedetomidine (1.5mcg/kg) and clonidine(2mcg/kg) used in their study. CONCLUSION The study results conclude that the addition of 1mcg/kg dexmedetomidine as an adjuvant to 0.75% ropivacaine in epidural anesthesia causes an early onset, good dermatomal levels and prolonged duration of sensory analgesia in comparison to 1mcg/kg clonidine.
REFERENCES
Policy for Articles with Open Access
|
|
 Home
Home