|
Table of Content - Volume 13 Issue 2 -February 2020
A comparative study of prophylaxis of post operative nausea and vomiting (PONV) with intravenous ondasetron, granisetron and palonosetron in patients undergoing laparoscopic abdominal and gynaecological surgeries under general anaesthesia
Neha Bharti1, Rajeev Lochan Tiwari2, Anshu SS Kotia3*
1Senior Resident, Department of Anaesthesiology, Atal Bihari Vajpayee Institute of Medical Sciences and Dr Ram Manohar Lohia Hospital, New Delhi, INDIA. 2Director and HOD, Department of Anaesthesiology, Fortis Escorts Hospital, Jaipur. 3Associate Professor, Department of Anaesthesiology, Jaipur National University Institute for Medical Sciences and Research Centre, Jagatpura, Jaipur. Email:health@jnuhealthcare.com
Abstract Background: Post- operative nausea and vomiting is a matter of concern in patients undergoing surgeries under General Anesthesia. People have used several groups of drugs to combat this “BIG LITTLE” problem. 5-HT3 receptor antagonists was heralded as major advancement in the treatment of PONV because of the absence of adverse effects that were observed with commonly used traditional antiemetics. Aim: To compare the prophylactic efficacy of intravenous ondansetron, granisetron and palonosetron, in prevention of Post Operative Nausea and Vomiting (PONV) in patients undergoing Laparoscopic Abdominal and Gynaecological Surgery under General Anaesthesia. To assess the requirement of rescue antiemetic (injection metoclopramide 10mg iv). Methods: This was a prospective randomized double binded study in which 90 patients were allocated to three different groups randomly namely O, G and P (30 in each group). Patients in group O, G and P received Ondansetron 4mg/kg iv, Granisetron 2.5mg/kg iv and Palonosetron 0.075mg/kg iv respectively 5 minutes before induction. Descriptive statistics, mean, standard deviation, one way ANOVA test and fisher’s exact test were used. Results: Percentage of patients having nausea and vomiting were significantly higher in Ondansetron group followed by Granisetron group and was least for Palonosetron group. Postoperatively incidence of nausea at 0-6 hrs were 50%, 43.34% and 10% in group O,G and P respectively (p value=0.002), at 6-12 hrs, 12-24 hrs and 24-48 hrs were significant at p value was <0.05. Postoperatively incidence of vomiting at 0-6 hrs were 36.6%, 26.67% and 10% in group O,G and P respectively (p value=0.04), at 6-12 hrs, 12-24 hrs and 24-48 hrs were significant at p value was <0.05. There was no complaint in palonosetron group in 24-48 hours, where as patient complaining of vomiting also decreased in ondansetron and granisetron group in this period. Significant difference in number of patients requiring rescue antiemetics at different time of study period (p value =0.02). However, frequency of use of rescue antiemetic was non significant in our study. As the frequency of requirement of rescue antiemetic was based on patient satisfaction and demand along with VAS>5, it was completely subjective. We also observed significant difference in number of complete responders at the end of 48 hours(p value=0.01).Conclusion: Palonosetron is better drug for prophylaxis of PONV in patients undergoing Laparoscopic Abdominal and Gynaecological surgeries under General Anesthesia as compared to Ondansetron and Granisetron due to its prolonged duration. Key Words: PONV (Post Operative Nausea and Vomiting), General Anaesthesia, Laparoscopy, Ondansetron, Granisetron and Palonosetron.
INTRODUCTION Laparoscopic surgeries are rapidly emerging as preferred surgical procedures these days. These have considerably decreased the surgical mortality. Post-operative nausea and vomiting (PONV) is a common adverse effect of the Anaesthesia in Laparoscopic Surgery.1,2 PONV causes patient discomfort and can result in unanticipated overnight hospital admission which leads to increased economic costs. Hence, it has been characterized as big “Little Problem” as it is the potential cause for delays in meeting discharge criteria both from the recovery room to ward and from the day ward to home. There is a strong association between PONV and patient dissatisfaction with their Anaesthesia care and thus controlling PONV is strong patient priority.3,4,5Incidence of PONV is 3040% in normal population and touches a peak of 7580% in certain highrisk groups. With the use of lesser emetogenic anaesthetic techniques and advent of newer drugs for the prophylaxis of postoperative nausea and vomiting, the incidence of PONV has come down by 50%, especially with the use of nonopioid medication for pain relief. Patient characteristics, type of surgical procedure, duration of anaesthesia, and surgery are few of the important determinants for risk of PONV. There is involvement of three nerves and seven neurotransmitters for activation of vomiting centre, which makes the prophylaxis and treatment complex.6Introduction of serotonin antagonists and the use of combinations of drugs for analgesia and control of PONV during the past decade is one of the most significant innovations to fight PONV. A number of pharmacological agents (antihistamines, butyrophenones, dopamine receptor antagonists) have been tried for the prevention and treatment of PONV but undesirable adverse effects such as excessive sedation, hypertension, dry mouth, dysphoria, hallucinations and extra pyramidal symptoms have been noted. 5hydroxytryptamine type3 (5HT-3) receptor antagonists are highly efficient in treatment and prevention of PONV and also free of such side effects. 7,8,9 Ondansetron is the first 5HT3 antagonist, used alone or in combination for the prophylaxis due to its lower cost. Granisetron is highly potent, selective and produces irreversible block of 5HT3 receptors. Longer half life of 40 hours, Palonosetron is the second generation 5HT3 antagonist with unique chemical structure.6,7,8,11 Metoclopramide a dopaminergic antagonist structurally related to Procainamide, is an effective agent in treating and preventing vomiting and is useful in oesophageal reflux disease, gastro paresis, dyspepsia and other gastrointestinal disorders9Studies have also shown that antiemetic prophylaxis with 5hydroxytryptamine subtype3 (5HT3) antagonists provided clinically effective prevention of postoperative nausea and vomiting with statistically significant difference in their efficacy and duration of action. However, due to its prolonged duration and minimal side effects, Palonosetron is found to be better drug for antiemetic prophylaxis of PONV in patients undergoing laparoscopic surgery under General Anaesthesia as compared to Ondansetron and Granisetron.6,10,12,13 We hypothesized that palonosetron being a longer acting and more effective drug would be better in preventing PONV after Laparoscopic Abdominal and Gynaecological surgeries.
AIM Primary Objective – To compare the prophylactic efficacy of three different intravenous 5HT-3 receptor antagonists “Ondansetron, Granisetron and Palonosetron” in patients undergoing Laparoscopic Abdominal and Gynaecological surgeries under General Anaesthesia regarding
Secondary Objective- Evaluate the need for rescue anti emetic (injection Metoclopramide 10 mg iv for control of Post–Operative Nausea and Vomiting.).
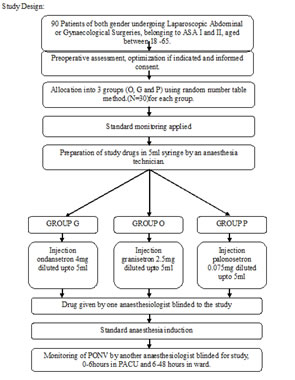
MATERIALS AND METHODS This three arm comparative prospective double blind randomized study was started after approval from Institutional Ethics Committee and conducted at Fortis Escorts Hospital, Jaipur. Sample size calculation was based on the study by Gupta K et al. (2015)6 difference in incidence of PONV in between the groups as 30% Assuming 45% difference in incidence of PONV between the two groups at α = 0.05 and power 90%, the sample size was calculated. Our sample size was 90 patients with 30 patients in each group. In this study, Randomization was done using random number table method. Double blinding was done to avoid bias.(the anaesthesiologist administering the drug and the anaesthesiologist involved in PONV assessment were unaware of the group allocation).In the current study, American Society of Anesthesiologist grade I and II, patients in the age group 18 to 65 years, who were planned for Laparoscopic Abdominal and Gynaecological Operations. A well informed consent (in English or Hindi language) regarding participation in this study was obtained from all the patients a day prior to surgery. Exclusion criteria were patients with allergy to experimental drugs, ASA grade III, IV and V, Opioid dependence, history of PONV and motion sickness and use of antiemetics 24 hr prior to surgery. 90 patients were allocated to three different groups (O, G and P) each using random number table method. Group O received injection Ondansetron 4mg iv bolus 5min before induction (N=30), Group G received injection Granisetron 2.5mg iv bolus 5 min before induction(N=30) and GROUP P received injection palonosetron 0.075mg iv bolus 5 min before induction(N=30). The total volume of the study material was 5 ml by adding normal saline. The study materials were prepared by anaesthesia technician, administered by an anaesthesiologist (blinded to the study), and postoperative observations were done by another anaesthesiologist (blinded to the study).On arrival in the operation room, an iv cannula of appropriate size was inserted into a vein on dorsum of nondominant hand and normal saline solution was attached. All the patients underwent routine monitoring which included noninvasive blood pressure, ECG, peripheral oxygen saturation, capnography in all patients and special monitoring according to the type and duration of surgery.On the day of surgery, a standardized anaesthesia regime was followed. The study drug was intravenously administered 5 minutes before induction after which patients was preoxygenated for 3 minutes. Anaesthesia was induced with 2mg/kg of propofol and 2µg/kg of fentanyl intravenously. Atracurium 0.5mg/kg intravenously was used to facilitate tracheal intubation. An orogastric tube of 14G was inserted which was removed following negative aspirationon completion of surgery. Heart rate, Systolic blood pressure, Diastolic blood pressure, were recorded ten minutes post induction to observe the effect of study drugs on haemodynamics. Anaesthesia was maintained with propofol 50-200mcg/kg/min using a target controlled infusion pump, infusion atracurium as well as sevoflurane in air oxygen(1:1)mixture using low flow anaesthesia. After anesthesia induction, patients were mechanically ventilated with constant flow and I:E ratio of 1:2, and tidal volume (TV) set at 8 ml/kg of ideal body weight. Respiratory rate was adjusted to 8–20 breaths/min to maintain end-tidal carbon dioxide concentration (ETCO2) of 30–40 mmHg at 50 % inspired oxygen with air. Pneumoperitoneum was established with a closed Veress needle technique, and the intra-abdominal pressure was maintained at 12–14 mmHg. After CO2 insufflation, patients were placed in the reverse Trendelenburg position at 20°. At the end of the operation neuromuscular block was decurarized by using neostigmine and glycopyrolate and subsequent extubation was done. For postoperative pain control, injection diclofenac 75 mg in 100ml normal saline iv and injection paracetamol 1gm iv at closure of incision wound (and repeated upon patient request.),along with infiltration of local anaestheticagent (0.25% bupivacaine) at the site of incision will be given.Post Operative assessment of nausea and vomiting was done by another anaesthesiologist blinded to study. Incidence of nausea and vomiting were recorded for (0-6) post operative hours in PACU (Post Anaesthesia Care Unit) and for (6-12, 12-24, 24-48) post operative hours in ward. Number of patients requiring rescue antiemetic were also noted. Patients who did not required any rescue antiemetic at the end of 48 hours were termed as complete responders.Visual analogue scale (VAS) was used to assess post operative nausea and vomiting. Rescue anti emetic was administered when patient had VAS Score > 5, had one or more episodes of vomiting and on patient’s demand. For statistical analysis of data, STATA 12 statistical software (Texas USA) was used. Descriptive statistics were used to describe the baseline characteristics. The quantitative variables were represented as mean and standard deviation where as qualitative variables were presented as number percentages. Continous numerical variables were compared using One way ANOVA test. Dichotomous variables were compared using fisher’s exact test. P value <0.05 was considered significant.
RESULTS In total, 90 patients were screened and found eligible for the current study. Mean age and Mean weight were comparable in all the three groups. No significant difference were observed among the three groups with regard to mean age, mean weight, gender distribution and ASA (p value=0.51, p value=0.24, p value=0.68 and p value=0.58; respectively). Mean ages were 43.27±11.01, 40.03±10.71and 40.77±12.36 years in group O, G and P respectively and mean weight were 63.07±7.78, 61.5±8.06 and 59.77±6.86 Kg (Table 1)
Table 1: Demographic profile
ASA – American Society of Anesthesiologist; M – Male; F – Female The patients were compared of pre-operative vitals (Systolic BP, Diastolic BP, Heart Rate and Respiratory rate) in all the three groups, and no significant difference were observed in mean vitals among the groups. Intraoperative vitals were also monitored 10 minutes post induction to rule out any haemodynamic change that could have occurred due to administration of study drugs. There was no major changes observed in haemodyanamic parameter as compared to base line haemodyanamic parameters.
Table 2: Comparison of Patients having post operative nausea
Significant differences were observed in incidence of nausea at 0-6hours (p value=0.0002), 6-12hours (p value=0.02), 12-24hours(p value =0.04) and 24-48hours(p value=0.02).Percentage of patients having nausea at (0-6) post-operative hours were 50%, 43.34% and 10% for group O, G and P respectively. Percentage of patients having nausea at (6-12) post-operative hours were 40%,30%and10% for group O,G and P respectively. Percentage of patients having nausea at (12-24) post-operative hours were 30%,30% and 6.67%in group O,G and P respectively. Percentage of patients having nausea at (24-48) post-operative hours were 30%,16.67% and 3.34% for group O,G and P respectively. (Table 2, Figure 1) Table 3: Comparison of Patients having post operative vomiting (in PACU)
Significant differences were observed in incidence of vomiting at 0-6hours (p value=0.04), 6-12hours (p value=0.004), 12-24hours(p value =0.02) and 24-48hours(p value=0.03).The percentage of vomiting in 0-6 post operative hour were 36.67%, 26.67% and 10% for groups O, G and P respectively. The percentage of vomiting in 6-12 post -operative hour were 43.33%, 23.33% and 6.67% in group O, G and P respectively.The percentage of vomiting in 12-24 post- operative hours were 23.34%, 16.67% and 0% in group O, G and P respectively.The percentage of vomiting in 24-48 post- operative hour were 20%, 13.4% and 0% respectively. (Table 3, Figure 2) Table 4: Comparison of Patient Requiring Rescue Anti Emetics among the Three Groups
Significant difference was observed in number of patients requiring rescue antiemetics at different time of study period ( p value =0.02). The percentages of patients requiring anti emetic were 43.33%, 26.67% and 10% in group O ,G and P respectively.Frequency of requirement of antiemetics was completely based on episodes of vomiting and request by patient. Frequency of use of rescue antiemetic revealed that the differences were not statistically significant in our study (p value = 0.48). As the frequency of requirement of rescue antiemetic was based on patient satisfaction and demand along with VAS>5, it was completely subjective and hence we observed no statistical significance in this parameter.
Table 5: Comparison of Complete Responders
Significant difference were found in number of complete responders at the end of 48 hours (p value=0.01).The percentage of patient showing complete response were (No PONV at completion of 48 post operative hours) 56.67%, 73.33% and 90% for group O ,G and P respectively.
DISCUSSION The present study was restricted to patients undergoing Laparoscopic Abdominal and Gynaecological Surgeries under General Anaesthesia and aimed to compare the efficacy of injection Ondansetron (4mg), injection Granisetron (2.5mg) and injection Palonosetron (0.075 mg) given as preinduction dose in prevention of post operative nausea vomiting (PONV).We found significant differences in incidence of PONV at different intervals of the study period. We found that pre treatment of inj palonosetron 0.075mg given 5 min before induction is more efficient in preventing PONV at different time duration of our study period. Significant difference was also observed among the patients in three groups regarding use of rescue antiemetic (p value=0.02). However no significant difference was found in frequency of use of rescue antiemetics among the three groups (p value=0.48). None of the patients were reported to have any side effects of either study drugs or the drug used for rescue anti emetic. Our study showed that Palonosetron is better drug for prophylaxis of PONV in patients undergoing Laparoscopic Abdominal and Gynaecological surgeries under General Anesthesia as compared to Ondansetron and Granisetron due to its prolonged duration. Various studies have been done to reduce the incidence of PONV since ether era. A number of pharmacological agents (antihistamines, butyrophenones, dopaminereceptor antagonists) have been tried for the prevention and treatment of PONV but undesirable adverse effects such as excessive sedation, hypertension, dry mouth, dysphoria, hallucinations and extra pyramidal symptoms have been noted. 5-HT3receptor antagonists are devoid of such side effects and are highly effective in prevention and treatment of PONV.15 Our study is in agreement with a study done by Basu A et al. (2011). They observed that the incidence of emesis-free patients during the 0-6 hours period was 100% for group P; 72% for group G and 56% for group O. During the 6-24 hours period incidence of emesis-free patients were 96% for group P; 56% for group G and 32% for group O. So to conclude, a single dose of palanosetron is a superior anti-emetic to granisetron or ondansetron in complete prevention of postoperative nausea and vomiting after middle ear surgery during the first 24 hours period. He did this study in middle ear surgeries which is also known to have high risk for PONV.16 Similar results were found by Gupta K et al. (2014), they observed Incidence of vomiting episode at 04 hours were observed in (25%) of ondansetron group, (5%) of palonosetron group, and (15%) of granisetron group. The difference among the groups was statistically highly significant (P < 0.01). 6Our result was also in accordance to Mandal SK et al. (2017) who found use of rescue antiemetic 6.7%in group Granisetron, 3.3%in group Palonosetron and 30% in group Odansetron. This result was statistically significant with p value =0.009.14 In other research by Lee WS et al. (2015), it was found that no of patient requiring rescue antiemetics was more in palonosetron group than in granisetron group.2 Our study also correlates with a study conducted by Bhattacharya DP et al. (2010). They observed that the antiemetic efficacy of palonosetron is similar to that of granisetron for preventing PONV during the first 24 hours (0-24 hours) after laparoscopic surgery and that Palonosetron is more effective than Granisetron for getting a complete response (no PONV, no rescue medication) for 24-48 hours.10 There are few limitations in our study. First, there was no control group because it would be unethical to deprive some Patients from prophylactic antiemetics to control PONV. Second, the Paediatric patients were excluded from the study. Hence, we could not evaluate effective dose and response of study drugs in paediatric age group.
CONCLUSION Palonosetron is better drug for prophylaxis of PONV in patients undergoing Laparoscopic Abdominal and Gynaecological surgeries under General Anesthesia as compared to Ondansetron and Granisetron due to its prolonged duration. Number of patients requiring rescue antiemetics were significantly less in Palonosetron group.
REFERENCES
Authors who publish with MedPulse International Journal of Anesthesiology (Print ISSN:2579-0900) (Online ISSN: 2636-4654) agree to the following terms: Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution License that allows others to share the work with an acknowledgement of the work's authorship and initial publication in this journal. Authors are permitted and encouraged to post links to their work online (e.g., in institutional repositories or on their website) prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work. |
|
 Home
Home