|
Table of Content - Volume 13 Issue 2 -February 2020
Evaluation of the efficacy of iv labetalol 0.25mg/kg in the attenuation of haemodynamic response to extubation
Sindhu S1, V Y Srinivas2*
1Resident, 2Professor, Department of Anaesthesiology, Mysore Medical College, Mysore. Email: vidyasagar103@gmail.com
Abstract Background: Tracheal extubation evokes various haemodynamic stress response in the form of tachycardia, raised blood pressure ,changes in the heart rhythm which is detrimental to susceptible patients. Hence a study is needed to find a pharmacological drug to attenuate the stress response to extubation. Materials and Methods: 60 participants belonging to ASA 1 or 2 of age group 18 – 55yrs were randomly divided into groups of 2. Group Lt received injection Labetalol iv 0.25mg/kg and group Ct received normal saline. Heart rate ,systolic and diastolic blood pressure were recorded at baseline, 2,5,8 minutes after drug infusion, at extubation, and 1,3,5,8,10 and 15 minutes post extubation. Results: Group Lt showed lowered heart rate, systolic and diastolic blood pressure at extubation and 15minutes post extubation compared to group CT. Conclusion: Injection Labetalol iv 0.25mg/kg effectively attenuated the haemodynamic stress response to extubation. Key Words: Labetalol, extubation, haemodynamic response.
INTRODUCTION Securement of airway by General anaesthesia with endotracheal intubation is the gold standard practice, this is followed by endotracheal extubation which is associated with autonomic disturbances such as hypertension, tachycardia, arrhythmias due to epipharyngeal and laryngopharyngeal stimulation. Extubation is also associated with coughing, straining and bronchospasm1-2 Many methods had been tried such as avoiding lighter planes of anaesthesia during extubation ,usage of lidocaine, calcium channel blockers, opiods have been tried for attenuation of sympathoadrenal response to extubation but not associated with 100% efficacy.3 Labetalol is an adrenergic receptor blocking agent with mild alpha-1 and predominant beta-adrenergic receptor blocking actions. It is an oral and parenteral antihypertensive drug that is alpha-1 and nonselective beta-1 and beta-2 adrenergic antagonist.4 Labetalol lowers the systemic vascular resistance (alpha-1 blockade) and there by decreases the blood pressure, whereas the response of tachycardia caused by vasodilatation is attenuated by simultaneous beta blockade. There is no effect on cardiac output.5 Hence a study is needed to evaluate the efficacy of 0.25mg/kg of iv labetalol in the attenuation of haemodynamic response to extubation.
METHODOLOGY After obtaining informed risk consent from all the participants and ethical committee clearance, the 60 participants of age group 18-55 yrs belonging to ASA class 1 or 2 were allocated into two groups of 30 each based on shuffled opaque sealed envelopes containing the name of the group. Patients with cardiac, renal and hepatic impairement, cerebral disease, difficult airway, heart blocks, bradycardia(heart rate <60bpm) were excluded from the study. Group Ct received 10ml of normal saline intravenously over 10minutes using a syringe pump before extubation. Group Lt received injection Labetalol 0.25mg/kg diluted upto 10ml with normal saline given over 10minutes before extubation. All the subjects were premedicated with injection Midazolam 0.05mg/kg body weight and injection ondansetron 0.1mg/kg body weight and induced with injection thiopentone 5mg/kg and injection vecuronium 0.1 mg/kg. Anaesthesia was maintained with oxygen,nitrous oxide, isoflurane with intermittent dose of injection vecuronium. Group Lt received injection Labetalol 0.25mg/kg diluted upto 10ml with normal saline given over 10 minutes before extubation and Group Ct - received 10ml of normal saline intravenously over 10minutes before extubation. At the end of the procedure, neuromuscular blockade was reversed with Inj neostigmine 0.05mg/kg body weight and Inj glycopyrrolate 0.01mg/kg body weight. Haemodynamic parameters such as heart rate, systolic and diastolic blood pressure were recorded at baseline,2,5,8 minutes after drug infusion, at the time of extubation and at 1,3,5,8,10 and 15 minutes postextubation. STATISTICAL ANALYSIS The calculation of sample size was done after discussion with the statistician, on the basis of pilot study observations. The observation conducted showed approximately each group should have 23 patients for ensuring a power of study 0.80 for detecting clinically meaningful difference by 15% in haemodynamic parameters. With assumption of 5% patients would drop out, the final study sample size was fixed at 30 patients in each group, allowing a type 1 alpha error =0.05 and a type 2 error of beta=0.2 and power of 0.8. All the statistical methods were carried out through Microsoft excel SPSS for Windows (version 20.0)
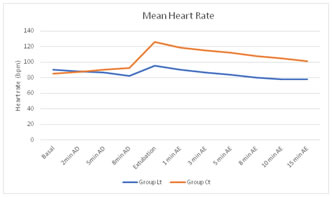
RESULTS There was no statistically significant difference in correspondence to demographic variables such as age, sex and weight. HEART RATE The difference in baseline heart rate was statistically insignificant in between the two groups. Group Lt showed a decrease in mean heart rate at 1,3,5,8,10 and 15 minutes postextubation compared to group Ct which was statistically significant. The mean heart rate remained below the baseline even at 15minute postextubation in group Lt which was statistically significant compared to group Ct. At extubation the mean heart rate was increased by 6bpm in labetalol group whereas in control group the mean heart rate was increased by 41bpm which was statistically significant.
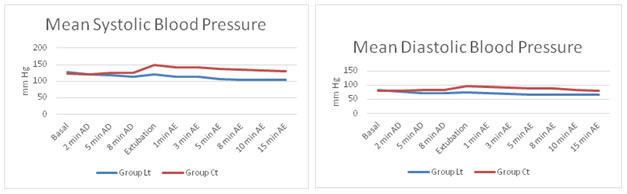
Figure1: showing changes in mean heart rate between labetalol and control group. SYSTOLIC AND DIASTOLIC BLOOD PRESSURE The baseline systolic and diastolic blood pressure were statistically insignificant between the two groups. Group Lt showed a decrease in mean systolic and diastolic blood pressure at extubation,1,3,5,8,10 and 15 minutes postextubation which was statistically significant compared to group Ct. The mean systolic and diastolic blood pressure remained below the baseline even at 15th minute postextubation which was statistically significant. At extubation, the mean systolic and diastolic blood pressure was decreased by 7mmhg and 6mmhg respectively in labetalol group whereas in control group , the mean systolic and diastolic blood pressure was increased by 25mmhg and 19mmhg respectively which was statistically significant.
Figure 2 Figure 3 Figure 2: showing changes in mean systolic blood pressure between Labetalol and control group; Figure 3: showing changes in mean diastolic blood pressure between Labetalol and Control group. DISCUSSION Extubation process in general anaesthesia is associated with autonomic disturbances in the form of increased heart rate and blood pressure due to raised catecholamines levels, anxiety, pain which is detrimental in cardiovascular and cerebrovascular patients.6 Therefore attenuation of extubation response is necessary. Labetalol is a is a salicylamide derivative. It has alpha: beta blockade ratio of 1:7 for iv and 1:3 for PO administration7. Labetalol exhibits equilibrium-competitive antagonism at beta and alpha receptors. The intrinsic activity or partial agonism action at beta- 2 receptors in the vasculature and by causing blockade of alpha receptors is responsible for vasodilator effect of the drug8. In our study, after infusion of 0.25mg/kg of labetalol group showed statistically significant decrease in mean heart rate and systolic and diastolic blood pressure after drug infusion and 15 minutes postextubation compared to control group. At extubation we noticed an increase of mean heart rate by 6bpm and decrease in systolic and diastolic blood pressure by 7mmhg and 6mmhg in Labetalol group. Our study results reveals that labetalol group showed a better control over haemodynamic parameters. In the study conducted by Younes M M et al9, the mean heart rate was decreased by 10bpm at extubation and mean arterial pressure was decreased by 25mmhg. Thus labetalol was effective in controlling haemodynamic response to extubaion. In the study conducted by patel H S et al10 at extubation the mean heart rate was decreased by 7mmhg, systolic blood pressure was decreased by 1mmhg and diastolic blood pressure was decreased by 3mmhg in labetalol group. Labetalol was more efficient in controlling Heart rate at 5th and 15th min postextubation having statistical significance in comparing with esmolol. This is probably because the difference in timing of administration of drug. In the study conducted by Babita et al.4 labetalol showed a effective attenuation of intubation response compared to fentanyl group. Various studies such as kunakeri SB et al11, Singh SP et al12, Kumar A et al13 labetalol effectively attenuated the sympathoadrenal response to intubation. In the study conducted by Attari et al.14 patients who were administered labetalol had a better haemodynamic control compared to morphine group. There was no statistically significant side effects in our study.
CONCLUSION From our study we concluded that administration of 0.25mg/kg of iv labetalol 10 minutes before extubation effectively attenuated the haemodynamic response to extubtion.
REFERENCES
Policy for Articles with Open Access |
|
 Home
Home