|
Table of Content - Volume 14 Issue 1 - April 2020
Levobupivacaine versus ropivacaine for orthopaedic surgeries under epidural anaesthesia - A prospective study
Kanika Garg1, Robina Makker2*, Nidhi Anand3, Madhuri Sharma4, Vinay Rai5
1PG Student, 2,4Associate Professor,3,5Professor, Department of Anaesthesia, Sgrrimandhs, Patel Nagar, Dehradun, INDIA. Email: robinamakker@yahoo.co.in
Abstract Background: Problem statement: Comparing the effectiveness of 0.5% Levobupivacaine and 0.75 % Ropivacaine for epidural anaesthesia for elective lower limb orthopedic surgeries. Methodology: Sixty patients between the age 18-55 years posted for elective lower extremity surgery were enrolled for prospective double blind study, randomized into two groups of thirty each. One group(group A) received 15 ml of 0.5% Levobupivacaine and the second (group B) received 15 ml of 0.75% Ropivacaine for epidural anaesthesia. All patients were in ASA class I and II with height between 150-180 cm. Epidural catheter was inserted by standard technique. Sensory and motor blockade characteristics and haemodynamic parameter were compared. This study was performed in Shri Guru Ram Rai Institute of Medical and Health Sciences after clearance from the institute’s ethical committee. Subjects included sixty adult patients ( age between 18 and 55 years ), scheduled to undergo orthopaedic surgery of lower extremity. Results: Regarding motor block onset, mean times in group R and group L were 9.53±2.6 and 10.53±2.71 minutes respectively and p value came to be 0.075, the difference being non significant statistically. However, highly significant difference (p value < 0.001) was found when the times at which maximum motor block appeared, were compared : group R - 36.67±8.06 minutes, group L - 25.37±8.03 minutes (Table 1). Also, highly statistically significant difference was found in grade of motor block between two study groups. Conclusion: Time of onset of block sensory and motor maximum level of sensory block were similar in both groups. There was statistically significant difference between groups with regards to onset and intensity of motor blockade, patients in group B had less time of onset and higher grade of motor block. There was no difference in duration of motor blockade and analgesia between the groups. Keywords: Ropivacaine, Levobupivacaine, epidural anaesthesia, lower extremity, orthopaedic
INTRODUCTION Regional anaesthesia has lot of advantages over general anaesthesia (GA) for lower limb orthopaedic surgeries.1 Epidural anaesthesia is preferred technique2 as it overcomes the limitations of intrathecal anaesthesia such as less duration, rapid sympathoplegia, non-extendable, short analgesia duration and spinal headache. Lignocaine and Bupivacaine have been the most commonly used agents for this technique. Duration of anaesthesia with Lignocaine is intermediate whereas Bupivacaine can cause severe central nervous system (CNS) and cardiac side effects after inadvertent intravascular injection. Ropivacaine and Levobupivacaine have only recently started to be used in epidural anaesthesia, with better therapeutic index3. Though both agents are readily available, they have not replaced use of Bupivacaine. With this view and as not much work has been done in this regard, a randomized study was performed to compare 0.5% Levobupivacaine and 0.75% Ropivacaine for regional anaesthesia via epidural route in orthopaedic surgery of lower extremity.
MATERIAL AND METHODS This study was performed in Shri Guru Ram Rai Institute of Medical and Health Sciences after clearance from the institute’s ethical committee. Subjects included sixty adult patients ( age between 18 and 55 years ), scheduled to undergo orthopaedic surgery of lower extremity. All patients were in ASA class I and II. Patients with co-morbid conditions like hypertension, diabetes mellitus, ischaemic heart disease and obesity with body mass index (BMI) more than 30 were excluded. Other exclusion criteria were pregnancy, emergency surgery, height less than 150 cm and more than 180 cm, raised intracranial pressure, severe hypovolemia, coagulopathy and local infection. After an informed consent was taken, patients were divided into two groups, each comprising 30 patients, using a computerized model to randomize. Injection Ropivacaine 0.75% - Group R (n=30) Injection Levobupivacaine 0.5% - Group L (n=30) Pre-anaesthetic examination on the evening before surgery assessed history and general condition of the patient, airway Mallampati grading, nutritional status, height and weight, detailed examination of the Cardiovascular, Respiratory and Central nervous systems and examination of the spine. Investigations done in all patients were haemogram, routine examination of urine, standard 12-lead electrocardiogram, random blood sugar, blood urea and serum creatinine and coagulation profile An anxiolytic (Alprazolam 0.5 mg) and an H2 receptor blocker (Ranitidine) were given as premedicants and patients kept fasting overnight. Basal haemodynamic parameters (pulse and blood pressure) were noted preoperatively. Patients were given 1.0 mg of injection Midazolam and preloaded with half a litre of Ringer’s Lactate before epidural anaesthesia. Basal haemodynamic parameters (pulse and blood pressure) were noted preoperatively. Patient was connected to a multiparameter monitor to record oxygen saturation (SPO2) and blood pressure (systolic-SBP, diastolic-DBP and mean-MAP). Under asepsis, midline approach was used to enter epidural space through second and third lumbar interspinous space using loss of resistance method. The space was catheterized and tested by a solution of lignocaine-adrenaline. First dose of study drug (5.0 ml) was injected with patient in sitting position, patients were shifted to supine position after one minute and remaining 10 ml of the drug was given. Drugs were prepared and administered by an anaesthetist blinded to study. Blockade parameters (motor and sensory) were noted at one minute interval after injection. Time taken to reach block and maximum level achieved were noted. A fine needle (22 gauge) was used to assess blockade of pain. Bromage scale was the criteria for motor block assessment (0 – Able to perform a full straight leg raise over bed for 5 sec, 1– Unable to perform leg raise but able to flex knee, 2 – Unable to flex the knee but can flex ankle, 3 – Unable to flex ankle but can move toes, 4 – Unable to move toes i.e total paralysis)4 Haemodynamic and respiratory (rate and oxygen saturation) parameters were recorded at regular intervals. Intraoperative and postoperative complications like decreasing blood pressure, variation in heart rate were noted and treated as required. Intervention (injection Mephentermine, fluid infusion) was done if systolic blood pressure fell below 90 millimeters of mercury, or there was a fall of more than 30% from preoperative level. Atropine was used to treat bradycardia. Postoperatively, time elapsed till patients complained of pain at surgical site (analgesia duration) was noted and pain relieved by epidural injection. Time taken for complete recovery of motor power was noted. Record was made of time taken to achieve loss of pin prick sensation at L1 (onset of sensory block) and also time taken to attain highest sensory block. For motor blockade, time taken to attain Bromage scale 1 was taken as onset and Bromage scale 4 as time taken for maximum motor block. Return of patients motor power to Bromage zero was noted as duration of motor block. SPSS version 15.0 was used for statistical analysis. Quantitative variables in both the groups were expressed as mean ± sd and compared using unpaired t-test between groups and paired t-test within each group (comparison with baseline values) at follow-up. The qualitative variables were expressed as frequencies/percentages and subjected to Chi-square test. P-value of less than 0.01 was taken as highly significant and more than 0.05 as non significant. Values less than 0.05 were considered as statistically significant.
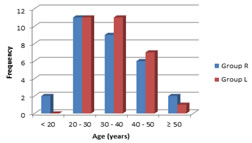
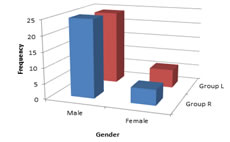
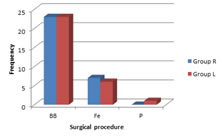
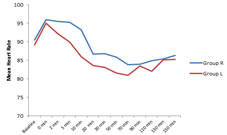
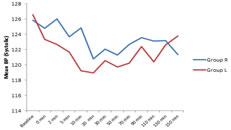
RESULTS Both groups, Ropivacaine (R) and Levobupivacaine (L) were similar in age and sex distribution (Figures 1 and 2), mean age being 32.6±9.39 years in group R and 33.40±7.89 years in group L. Majority of patients were males in age group 20-40 years. The groups were also similar regarding weight, height and operations performed (Figure 3). No statistically significant difference was found regarding onset time and maximum sensory blockade (Table 2) achieved between two groups. Sensory block took mean 7.07±1.76 minutes in group R to start where as it was 7.43±1.68 in group L, with a p value – 0.206, not significant statistically. Sensory block reached its maximum level at mean of 24.43±9.07 minutes in group R and 21.27±5.73 minutes in group L with no significant difference statistically (p value – 0.056). Regarding motor block onset, mean times in group R and group L were 9.53±2.6 and 10.53±2.71 minutes respectively and p value came to be 0.075, the difference being non significant statistically. However, highly significant difference (p value < 0.001) was found when the times at which maximum motor block appeared, were compared : group R - 36.67±8.06 minutes, group L - 25.37±8.03 minutes (Table 1). Also, highly statistically significant difference was found in grade of motor block between two study groups. 20 patients from group R attained Bromage 2 motor block vis-à-vis only 5 patients in group L (p value 0.001). 5 patients from group R versus 13 patients from group L achieved Bromage 4 grade block (p value 0.022). A higher intensity of motor block of Bromage 3 and 4 was attained by 10 patients in group R versus 25 patients in group L, p value being 0.012. If mean grade of motor block is compared between the groups, with a value of 2.5±0.78 in group R and 3.27±0.74 in group L, the difference comes out to be statistically highly significant (p value < 0.001) revealing that group L patients achieved a higher grade block. Thus, it turned out that Levobupivacaine produced faster and more intense motor blockade. As far as the criterias of duration of surgery, time duration of persistence of analgesia and motor blockade were concerned, they were similar in both groups (Table 4). Figures 4 and 5 and Table 5 show haemodynamic changes observed. Haemodynamic parameters recorded at designated intervals did not show any significant statistical difference between the groups. However, statistically significant number of patients developed bradycardia in group L at 10 minute interval from the start and required parenteral Atropine. Hypotension was observed in seven patients and four patients in group R and group L respectively, which was ameliorated by bolus administration of fluid intravenously supplemented by Mephentermine, if required. Apart from hypotension and bradycardia, no other complication was noted in any of patients in either group. Four patients in group R and five in group L required rescue analgesic, p value being 0.359, statistically non significant.
Levobupivacaine has been recently introduced into clinical practice. Levorotatory isomers have been shown to have a safer pharmacological profile5,6 with less cardiac and neurotoxic adverse effects7,8. Decreased toxicity of Levobupivacaine is attributed to its faster protein binding rate9 Ropivacaine, an amide local anaesthetic is pure enantiomer with long duration of action. It is stereoselective and less lipophilic than Bupivacaine, therefore, has a significantly higher threshold for toxicity of cardiovascular and central nervous system. It was decided to compare these two drugs as not much studies are available in published literature comparing these drugs. Ropivacaine, Bupivacaine, Levobupivacaine have been used in many studies for regional anaesthesia9-15 and drawn a conclusion that a ratio of 1:15 for Levobupivacaine and Ropivacaine is equipotent. In our hospital 15 ml of 0.5% of Bupivacaine is routinely used for lower extremity orthopaedic surgeries under epidural anaesthesia, in a total dose that becomes 18 ml including 3 ml test dose. This is calculated as 1.0 ml / segment upto 150 cm of height and adding 0.1 ml / segment for every 5.0 cm of increasing height2. The mean height in our study being 170 cm in both groups and considering that a block upto T10 (13 segments) is required for lower limb surgeries, total volume required would be 18 ml. Hence, in both groups 15 ml was selected as the volume of study drug other than the test dose. Patients with lower extremity injuries find lateral position uncomfortable, therefore epidural block was given in sitting position. Patients were turned supine after giving 5.0 ml drug to ensure a dense block of the thickest sacral nerve roots1. Study groups were similar with respect to demographic parameters. No statistically significant difference was found in onset time of sensory block between the groups, the time being 7.07 ±0.76 min. with ropivacaine (R) and 7.43 ±1.68 min. with levobupivacaine (L). Study conducted by Peduto et al..17 also showed no statistically significant difference in onset of sensory block the times being 29±24 min. and 25±22 min. with Levobupivacaine and Ropivacaine respectively. In variance to our study, their patients depicted more time was taken in all subjects for sensory block onset, irrespective of the drug used, as they assessed absence of pain to pin prick at T10 in contrast to L1 in our study. Various studies comparing Bupivacaine with either RS Bupivacaine or Ropivacaine also did not find significant difference in sensory block onset time.18-20 The level of sensory block varied from T11 to T4 in our study with 4 patients in group R and 1 patient in group L achieving a maximum level of T4 sensory block. 0.75% ropivacaine has been used by studies by Jeffery A Katz et al..20, Thompson GE et al..21and Wolff AP et al..22 with findings of a block of sensory level upto T5 and T4 corroborating with our study. Cox et al..found, maximum sensory spread to be at T8 with 0.5% levobupivacaine12. This is at variance with our study, probably, because the total volume of drug used for this study was 3 ml less (15 ml) than that was used in our study (18 ml). The maximum level of sensory block was achieved in a mean time of 24.43±9.07 mins and 21.27±5.73 mins in group R and L respectively, which was found to be not a statistically significant difference. Cox et al. showed this time to be 25 minutes in a study comparing different concentrations of Levobupivacaine (0.5% and 0.75%) and Bupivacaine (0.5%) 12 . These are similar to our study. Jaffery A Katz et al..20, Bannister J et al..23 and Dusanka Zaric et al..24 have compared sensory block characteristic of Ropivacaine and Bupivacaine, their studies did not report a significant statistical difference when the times to reach maximal sensory block were compared. This finding is similar to that arrived on our study. Duration of analgesia was 260.77±48.54 mins with Ropivacaine vs. 252.47±33.5 mins with Levobupivacaine, difference not significant statistically. This is at variance, though not significant, with studies of Cox et al..12 ( 0.5 % Levobupivacaine – 377 mins, 0.5% Bupivacaine – 345 mins ), Concepcion M et al..26 – 298 +_47 and Dusanka et al..24 – 353+_11.9 mins. However, Jaffrey A Katz et al..20,25, Thompson GE et al..21 showed significantly higher duration of analgesia ( 6.5+_0.4 hours, 8.1+_0.89 hours, 6.6+_2.0 hours respectively ) which could be because of higher volume ( 20 ml in contrast to 15 ml in our study) of drugs used in their studies. Brockway MS et al..18showed 272 mins as duration of analgesia while using 0.75% Ropivacaine, which is comparable with present study. Supplemental analgesia was required in 4 patients of Ropivacaine group and 5 patients in Levobupavacaine group, not different statistically. In a study by Peduto et al..17 , supplemental analgesia was required in 1 patient receiving Levobupivacaine and in 2 patients receiving Ropivacaine ( p value = 0.99 ) which compares with our study The mean time for the onset of motor blockade in group R was 9.53±2.6 minutes and it was 10.53± 2.71 in the other group. This was found to be non significant statistically. Time taken to attain grade 1 on Bromage scale was recorded as the start of motor blockade. Intense motor blockade, grade 4 of Bromage scale, was seen in 13 patients in group L patients where as this degree of motor blockade was seen in only 5 patients of group R. Our findings are comparable to those of Peduto et al. as the also found similar difference in intensity of paralysis of motor function between Levobupivacaine and Ropivacaine. A highly significant difference (p value < .001) was found between our study groups when mean times (group R – 36.67 +_8.06 min, group L – 25.37+_8.03 min) to achieve maximum motor blockade were compared. Motor paralysis lasted for 227.97 +_ 46.22 min in group R compared to 214.57 +_ 28.99 min in group L, the difference being statistically non significant. Our findings are similar to those reported by Peduto et al... No significant difference emerged between two groups on comparison of vital parameters such as BP, HR. A statistically insignificant difference was observed in incidence of hypotension (group R – 7, group L – 4). These findings are again consistent with other studies such as of Peduto et al. who observed non significant difference in incidence of hypotension (2 in group L and 8 in group R, p value – 0.16) between their study groups. CONCLUSION REFERENCES
Policy for Articles with Open Access
|
|
 Home
Home