|
Table of Content - Volume 14 Issue 1 - April 2020
M S Prasanthkum1*, S Shaik Mushahida2
1Associate Professor, 2Professor, Department of Anaesthesiology, PSG Institute of Medical and Research Centre, Coimbatore, INDIA. Email: jabarali2009@gmail.com
Abstract Background: : Pain is defined according to the International Association for the study of pain, as “An unpleasant, sensory and emotional experience associated with actual or potential tissue damage or described in terms of such damage” Aim: The aim of the study is to compare the hyperbaric bupivacaine 0.5% and hyperbaric 0.5%+Fentanyl 20 micrograms in spinal anesthesia for elective lower abdominal and lower limb surgery. Methods: This prospective comparative study was conducted in patients of grade I and II physical status, undergoing elective surgeries of lower abdomen and lower extremities aged 18 to 65 years. In Group A 30 patients received 2.5ml of hyperbaric bupivacaine 0.5% with 0.4ml of Normal saline and in Group B 30 patients received 2.5ml of hyperbaric bupivacaine 0.5% with 0.4ml of (20ug) of fentanyl citrate and normal saline was added to 5ml syringe containing 2.5ml of bupivacaine using a 1ml syringe for accuracy. Results: Out of 60 patients, 30 patients included in group A and 30 patients included in group B. In group A meantime for two-segment regression was 83.0 minutes and in group B was 114.5 minutes, time for full motor recovery in group A was 192.7minutes and in group B was 206.6 minutes, the meantime for complete sensory recovery in group A was 214 minutes and in group B it was 242 minutes, the time for the first request of analgesics postoperatively in group A 246.7 minutes and in group B it was 333 minutes. The visual analogue score in group A at 3 hours, 6hours postoperatively and 24 hours was 0.6,4 and 4.0 and, in the group, B was 0.1, 1.7, 2.6. Conclusion: From this study, we concluded that the addition of 20ug of fentanyl to 0.5%hyperbaric bupivacaine in spinal anaesthesia, prolongs the duration of sensory and motor blockade, increase the duration and quality of postoperative analgesia 12 – 24 hours without causing any gross haemodynamic disturbances or adverse effects. Keywords: Fentanyl, Bupivacaine, Hyperbaric, Anaesthesia.
INTRODUCTION Pain is defined according to the International Association for the study of pain, as “An unpleasant, sensory and emotional experience associated with actual or potential tissue damage or described in terms of such damage”.1 Spinal anaesthesia consists of the temporary interruption of nerve transmission within the subarachnoid space produced by injection of a local anaesthetic solution into cerebrospinal fluid. SA is a routinely used anaesthetic technique for operations involving the lower limbs, lower abdomen, pelvis and perineal surgeries.2,3,4 An increasing proportion of the patients undergoing these surgical procedures are the elderly.5 Age-related changes in physiology and pharmacology can affect every aspect of pre-operative care.6 The use of spinal anaesthesia is increasing in popularity compared to general anaesthesia.2,3,7 Used widely, safely and successfully for almost 100 years spinal anaesthesia has many potential advantages over general anaesthesia, especially for operations involving the lower abdomen, the perineum and the lower extremities.2,3,4 The role of an anaesthesiologist is to render pain free during surgical procedures. However, the patient's problem with pain does not end with surgical procedures. Pain during the postoperative period is a cause of concern not only for the patient but also for the surgeon and the anaesthesiologist. Postoperative pain control is generally best managed by an anesthesiologist because they offer regional techniques of anaesthesia as well as pharmacological expertise in analgesics. Spinal anesthesia is advantageous in that it uses a small dose of anaesthetic, is simple to perform and offers a rapid onset of action, gives reliable surgical and good muscle relaxation. These advantages are sometimes offset by a relatively short duration of action and complaining of postoperative pain when it wears off. Spinal anesthesia with hyperbaric bupivacaine 0.5% is a popular method, but there is a need for increasing the duration of analgesia without increasing the duration of motor blockade and thus prolong the duration of postoperative analgesia. The addition of fentanyl has been suggested as a method to accomplish these goals. This study is designed to quantitatively examine the effects of adding fentanyl to hyperbaric bupivacaine on the duration and recovery of sensory and motor block. AIM The aim of the study is to compare the hyperbaric bupivacaine 0.5% and hyperbaric 0.5%+ Fentanyl 20 micrograms in spinal anesthesia for elective lower abdominal and lower limb surgery.
MATERIALS AND METHODS A prospective comparative study was conducted in the PSG hospitals, Coimbatore over a period of 18monthstocompare the Hyperbaric bupivacaine 0.5% and hyperbaric 0.5%+ Fentanyl 20 micrograms in spinal anesthesia for elective lower abdominal and lower limb surgery under different study parameters like onset and duration of analgesia, duration of sensory and motor blockade, quality of analgesia and side effects or complications. Inclusion criteria include ASA grade I and II physical status, undergoing elective surgeries of lower abdomen and lower extremities aged 18 to 65 years and exclusion criteria include the history of allergy or sensitivity to local anaesthetic or opioids, any contraindication to regional anaesthesia and ASA grading III and IV. A detailed pre-anesthetic examination including history, clinical examinations, the systemic examination of the cardiovascular, respiratory, central nervous system and examination of spine for deformity was performed. Routine investigations like haemogram, bleeding time, clotting time, blood sugar, blood urea, serum creatinine, ECG, Chest X-Ray were done wherever necessary. Patients' weight and height were also recorded prior to surgery. Premedication was standardized with Tab diazepam 0.2mg/kg preoperative on the night before surgery. All patients were instructed about the visual analogue scale(VAS).Patients were allocated into two groups viz., groups A, group B. In Group A 30 patients received 2.5ml of hyperbaric bupivacaine 0.5% with 0.4ml of Normal saline and in Group B 30 patients received 2.5ml of hyperbaric bupivacaine 0.5% with 0.4ml of (20ug) of fentanyl citrate andnormal saline was added to 5ml syringe containing 2.5ml of bupivacaine using a 1ml syringe for accuracy. Before the start of the procedure, patients' pulse rate, blood pressure, respiratory rate, oxygensaturation was recorded. An intravenous line was secured using an 18G intravenous cannula. All patients were preloaded with 500ml of Ringer’s lactate prior to spinal anaesthesia. The patients were kept nil per orally for 8 – 10 hours before surgery. The side effects of intrathecal fentanyl-like nausea, vomiting, pruritis, shivering respiratory depression (respiratory rate <10min), drowsiness, hypotension euphoria, chest tightness and urinary retention were noted. Hypotension was defined as a decrease in systolic blood pressure more than 20% of the baseline values and was treated with injection mephentermine 5mg intravenous increments and bradycardia (pulse rate <60/min) was treated by atropine 0.6mg intravenous stat. Under aseptic precautions lumbar puncture was performed in the left lateral position or sitting position by midline approach by using disposable quincke spinal needle (23-26G) at L3-L4, intervertebral space. Patients were monitored continuously using sphygmomanometer, pulse oximeter and electrocardiogram, patients pulse rate, blood pressure, oxygen saturation were recorded at 0,5,10,20,30,60,120 and 180 minutes. The sensory level was tested by pinprick using a hypodermic needle and the motor level was assessed by the Bromage scale. A pretested proforma will be used for collecting relevant data. Quantitative data will be analysed by students' “t” test and qualitative data will be analyzed by the chi-square test.
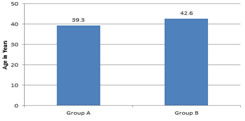
RESULTS The mean age group A was 39.3 years and group B 42.6 years. The two groups did not differ significantly (P=0.28) with respect to their age. In Group A There were 10 male and 20 female patients. In Group B there were 12 male and 18 female patients. The height of patients in group A ranged from 4 feet (ft) 1 inch to 5 feet 9 inch with a mean height of 5.33 ft. In group B also the height ranged from 4 feet 1 inch to 5 feet 9 inches but the mean height was 5.24ft. The height of patients in group A ranged from 4 feet (ft) 1 inch to 5 feet 9 inch with a mean height of 5.33 ft. In group B also the height ranged from 4 feet 1 inch to 5 feet 9 inches but the mean height was 5.24ft.
Figure 1: Age wise distribution
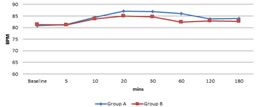
Figure 2: Distribution of Heart rate In Group A the mean baseline heart rate was 80.8bts/min. In Group B the mean baseline heart rate was 81.33 beats/min.
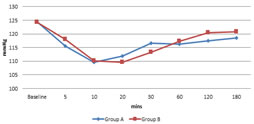
Figure 3: Distribution of Systolic BP In Group A the mean systolic BP was 116.3mmHg. In Group B the mean systolic BP 116.75mmHg.
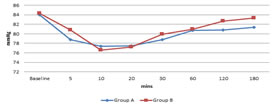
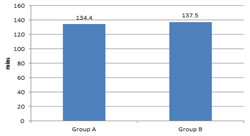
Figure 4: Distribution of Diastolic BP The preoperative mean diastolic blood pressure in group A was 84.0mmhg, In Group B the preoperative mean diastolic blood pressure was 84.3mmhg. The mean time of onset of sensory blockade in Group A was 134.4 ± 14.9 seconds and group B was 137.5 ± 13.5 seconds.
Figure 5: Onset of sensory blockade
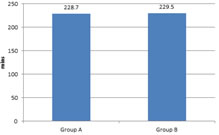
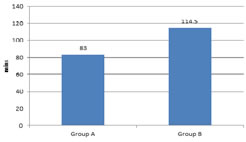
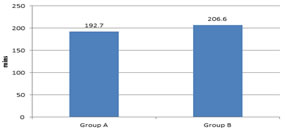
Figure 6: Onset of motor blockade The mean time of onset of motor blockade group A was 228.7 ± 20.5 seconds and the meantime of the onset of the motor blockade in Group B was 229.5 seconds. In this study out of 60 patients the meantime for two-segment regression in group A was 83.0 Minutes and in group B was 114.5 minutes. Figure 7: Time for two segment regression of sensory level In this study out of 60 patients, the time for full motor recovery in group A was 192.7 minutes and in group B was 206.6 minutes.
Figure 8: Time to full motor recovery
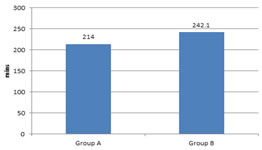
In this study out of 60 patients the meantime for complete sensory recovery in group A was 214 minutes and in group B it was 242 minutes.
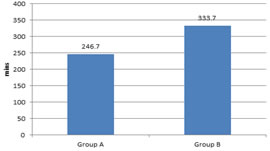
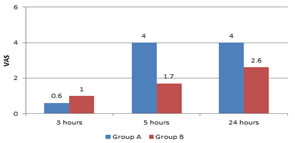
Figure 9: Time for complete sensory recovery In this study out of 60 patients the time for the first request of analgesics postoperatively in group 246.7 minutes and in group B it was 333 minutes. Figure 10: Time for the first request of analgesics In this study out of 60 patients the visual analogue score at 3 hours was 0.6 in group A and 0.1 in Group B. At 6 hours postoperatively VAS was 4 in group A and 1.7 in group B. At24 hours VAS `was 4.0 in group A and 2.6 in Group B.
Figure 11: Visual analogue scores (vas) at different time
DISCUSSION The subarachnoid block is one of the commonest local anaesthetic technique and would probably maintain its place in the developing countries, because of simplicity minimal skill requirement, rapidity of onset, economy and minimum postoperative complications. It has the advantage thatit is easy to perform, requires a small dose of the drug, making systemic absorption unimportant. The disadvantage is the limited duration of action and lacks postoperative pain relief. The drugs used for the spinal subarachnoid block are lignocaine and bupivacaine. The disadvantage of spinal anaesthesia with local anaesthetic is that analgesia ends with regression of the block, which means there is an early postoperative need for analgesia. The use of neuraxial opioids has increased dramatically in recent years, augmenting the analgesia produced by local anaesthetic by binding directly to opiate receptors. The synergistic action of local anaesthetic and morphine is well known, but Fentanyl may have an advantage over morphine because of its rapid onset of action and superior intraoperative conditions. In the present study the patients studied in both the groups did not vary much with respect to age, sex, weight or height. Majority of the patients were middle-aged in both groups between 26-55years, with mean age of 39.3 years in group A and 42.4 years in group B. In both the groups' females were more, 66.66% of females were studied in group A and 60% of females in group B. The mean height and weight in either group were also identical. The type of surgeries performed was also identical in both groups. These parameters were kept identical in both groups to avoidthe intraoperative and postoperative outcomes of patients. In the present study all the patients were monitored clinically in the intraoperative period. Pulse rate, systolic blood pressure and diastolic blood pressure was monitored at regular intervals. The incidence of hypotension was noticed in four patients of group A and in only two patients of group B. Hypotension was corrected by administration of injection mephentermine 5 mg IV in incremental doses, giving IV fluids and foot end elevation. Systolic diastolic blood pressure in both groups did not vary significantly in other patients. The incidence of bradycardia was not seen in any of the patients of either group and there was no significant difference in the onset of sensory and motor blockade and respiratory rate. In our study we found that time for two-segment regression was significantly prolonged inFentanyl group. Liu S et al.8 in 1995, Harbhej Singh et al.9 in 1998, Techanivate A et al.10in 2004 found that two-segment regression was significantly prolonged in patients who received intrathecal Fentanyl with bupivacaine and was similar to our studies. Hunt CO et al.11 in 1989 conducted a study in 50 patients who received either 0, 2.5, 5,6.25, 25, 27.5 or 50ug of fentanyl along with bupivacaine. He noticed that at 60 minutes the number of segments regressed was prolonged in 50ug fentanyl groups. But by 120 minutes there were no differences= between groups in the number of segments regressed. In the study, the duration of motor and the sensory block was significantly prolonged in the fentanyl group. Techanivate A et al.10 in 2004 concluded that fentanyl increases the duration and the intensity of bupivacaine in spinal anaesthesia, whereas Liu Set al.8in 1995, Harbhej Singh etal9 in 1998found that addition fentanyl to 0.5% bupivacaine does not prolong the duration of motor blockade but it only increases the time of sensory blockade without prolonging recovery to micturition or street fitness. In a study conducted by Kuusniemi KS et al12 in 2000 he found there was no difference in the duration of motor block among patients who received bupivacaine 10mgonly and bupivacaine 7.5ug and fentanyl 25ug, but the duration were prolonged in thethe group which received 10mg bupivacaine and 25ug fentanyl. The duration was shortest among the group which received 5mg bupivacaine + 25ug fentanyl. Similarly, the duration of sensory block was maximum in the group which received 10mg bupivacaine and fentanyl 25ug and least in the group which received 5mg bupivacaine 25ug of fentanyl. In our study the meantime for the first request of analgesics in group A was 246 minutes and group B was 333 minutes. This was statistically highly significant. Hunt CO et al.13 in 1987 found in their studies that fentanyl increases the duration of analgesia. Harbhej Singh et al.9 in 1998 concluded that intrathecal fentanyl 25 micrograms with 0.5% bupivacaine reduced analgesic the requirement in the early postoperative period. The visual analogue pain score (VAS) at 3 hours was 0.6 ± 0.8 in group A and 0.1 ± 0.3 in group B. At 6 hours it was 4 ± 0.9 in group A and 1.7 ± 0.9 in group B. At 24 hours it was 4.0 ± 1.3 and 2.6 ± 1.3 in groups A and B respectively. The VAS was lower in group B at all time intervals, which indicates that the quality of analgesia was better in group B patients even upon 24 hours postoperatively. Hunt Co et al.13 in 1987, Techanivate A et al.10 in 2004 found that the use of intrathecal Fentanyl significantly reduces pain scores in the early postoperative period extending upon 12 hours.Hunt CO et al.11 in 1989 found that fentanyl added to bupivacaine increased the quality of perioperative analgesia.
CONCLUSION The addition of 20ug of fentanyl to 0.5% hyperbaric bupivacaine in spinal anaesthesia, prolongs the duration of sensory and motor blockade, increase the duration and quality of postoperativeanalgesia 12 – 24 hours without causing any gross haemodynamic disturbances or adverse effects. Based on the above facts we conclude the addition of fentanyl has many advantages and can be recommended with all spinal anaesthesia techniques.
REFERENCES
|
|
 Home
Home