|
Table of Content - Volume 14 Issue 1 - April 2020
Assistant Professor, Department of Anaesthesiology, SriMuthukumaran Medical College and Hospital, Chennai, INDIA. Email: kawinkumar8419@gmail.com
Abstract Background: Tonsillectomy is one of the commonest surgical procedures performed in the field of otorhinolaryngology. The most common and distressing symptoms, which follow anaesthesia and surgery, are pain and emesis. Effective preventive analgesic technique may not only be useful in reducing the acute pain, but also chronic post surgical pain and disabilities. Paracetamol is an effective analgesic and an antipyretic agent. Aim of The Study: The aim of the present study was to evaluate the efficacy, safety and hemodynamic variables of Intravenous Paracetamol as a pre-emptive analgesic in relieving the post operative pain. Materials and Methods:70 ASA I physical status patients undergoing tonsillectomy were selected between the age group of 6-16 years. The patients were divided into two groups. One group was administered I.V Paracetamol and the other group were given I.V saline as placebo. Pain score and sedation score were noted after the tonsillectomy procedure. Results: Data were analysed using SPSS version 13.0 computer software at level of significance p = 0.05. Iv paracetamol provided effective pain control in the post operative period upto a period of 6 hours. Conclusion: Intravenous Paracetamol can Key Word: Intravenous Paracetamol, Tonsillectomy, Pre emptive analgesia, Ramsays sedation scale, Visual Analog Pain Scale.
INTRODUCTION Tonsillectomy is one of the commonest surgical procedures performed in the field of otorhinolaryngology. The most common and distressing symptoms, which follow anaesthesia and surgery, are pain and emesis1. The provision of adequate analgesia after tonsillectomy presents the anaesthesiologist with difficulties, as this is a painful procedure and may be associated with significant bleeding into the airway2. The objective of the present study is to evaluate the post-operative analgesia, the haemodynamic profile and the side effects of IV Paracetamol.
MATERIALS AND METHODS The study was planned as a Prospective, randomized, double blinded, comparative study. After obtaining the institutional ethical committee approval and written informed consent from the parent/guardian, 70 ASA I physical status patients undergoing tonsillectomy and weighing between 10-30 kg between the age group of 6-16 years were selected for the study. All the 70 patients were randomised in two groups and the entire sample of patients stood an equal chance of getting into any group. Double blinding was done by taking appropriate dose of intravenous paracetamol calculated in mg/kg and was added to a solution of normal saline to make a volume of 100 ml. This was labelled as drug A. Plain 100 ml of normal saline was labelled as drug B. Neither the person administering the drug nor the person observing the patient in the post-operative period knew the drug dose. The following data were collected from the patients, viz.,
The exclusion criteria for the study included,
History regarding previous anaesthesia, surgery, any significant medical illness, medications and allergy were recorded. Age, Inpatient Number, Body Weight, Baseline vital parameters were recorded. Complete physical examination and airway assessment were done. Following laboratory investigations were done:
The routine Anaesthesia protocol was followed viz.,
GROUP N- normal saline 100ml infusion as placebo
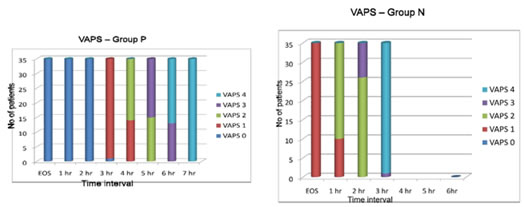
The following criteria were noted -Duration of surgery -Sedation score using Ramsays Sedation Scale -Visual analogue pain scale at the end of surgery, 1h 2h,3h,4h,5h,6h. -Post operative complications such as Drug intolerance, Nausea and vomiting, Epigastric pain, Bleeding Post-operatively the patients were monitored for changes in pulse rate, MAP, Spo2 for a period of 6 hours and were instructed to mark a point on the 10 point visual analog pain scale according to the intensity of pain. The pain relief was graded as follows in VAPS.
The pain score was assessed for a period of 6 hours and the total duration of post operative analgesia was taken as the period from the end of surgery till the first requirement of systemic analgesic medication. In both the groups patients were given the first analgesic medication when the VAPS score was 4 and above. Patients were observed for any side effects like intolerance, bleeding, epigastric pain, PONV. Sedation score was assessed using Ramsays sedation scale as follows.
RESULTS Data were analysed using SPSS version 13.0 computer software at level of significance p = 0.05. Numerical variables were presented as mean and standard deviation (SD) and categorical variables were presented as frequency (%). Unpaired Student 't' test was used for between-group comparisons between categorical variables. Time to first analgesic administration was analysed by the Kaplan-Meier survival analysis. The mean ages between the two groups were 9.7 ± 1.9 and 9.8 ± 2.8 for P and N group respectively. The difference between two mean ages was not statistically significant (P>0.05). The ratio of male to female remained the same in both P and N groups. The difference in percentage between two groups was not statistically significant. The mean weights between the two groups were 61.1 ± 3.2 and 59.7 ± 3.5 for P and N group respectively. The difference between two mean weights was not statistically significant (P > 0.05). The duration of surgery for both groups was comparable and was found statistically not significant. The two groups were compared with reference to their age, sex, weight and duration of surgery and they were amenable for comparison of other variables like duration of analgesia and haemodynamic variables such as MAP, PR and SpO2. Statistically significant (p<0.001) prolongation of duration of analgesia in the paracetamol group lasting for about 6.1 hours in the postoperative period as compared to placebo group which was only 2.6 hours. Table 1: Haemodynamic variables in the preoperative period
The pulse rate, MAP and SpO2 of both groups reveals that there was no statistically significant difference between both the groups before surgery (p>0.05).
Table 2: Haemodynamic variables in the intra operative period
TABLE 3- HAEMODYNAMIC VARIABLES IN THE POST OPERATIVE PERIOD
As shown in the table above, the mean pulse rate at 0 - 6 hours in the post operative period for P group was significantly lower than the N group with P < 0.001. The mean MAP at 0 - 6 hrs in the post operative period was significantly higher in N group than P group with P < 0.001. There was no significant difference in respect to mean post operative SpO2 in both groups.
TABLE 4: POST OPERATIVE SEDATION SCORE
Statistically significant conscious sedation was observed in paracetamol group with a score of 2.6 at the end of first hour, 2 at the end of second hour, 1.7 at the end of 3 hours after that both the groups were with a mean score of 1 up to six hours in post operative period.
This graph compares the quality of analgesia assessed by using VAPS score between 0-10 with 0 being excellent pain relief and score of 10 being the worst pain ever. Patients in both the groups were given rescue analgesic in the form of intramuscular diclofenac 1.5mg/kg if the VAPS score was more than 4. In the P group all patients had a VAPS score of 4 after a mean duration of 6 hours while in the N group a VAPS score of 4 was attained even before the end of 2.5 hours and rescue analgesic was given. The Kaplan Meier survival curve shows the cumulative survival of all the patients in respect to time to analgesic requirement. The above graph shows the existence of post operative analgesia in both the groups. 62.9% of the patients had been continuing analgesia upto 6 hours and the remaining 37.1% had been experiencing analgesia upto a period of 8 hours in the post operative period. But the same analgesic effect was present in the N group only upto 4 hours after which there were no patients continuing the analgesia. There were no adverse events of intolerance, bleeding, epigastric pain, PONV observed in both the groups.
DISCUSSION Pain is a personal, subjective experience that involves sensory, emotional and behavioral factors associated with actual or potential tissue injury. What patients tell us about their pain can be very revealing and an understanding of how the nervous system responds and adapts to pain in the short and long term is essential if we are to make sense of patients' experiences. The wide area of discomfort surrounding a wound, or even a wound that has healed long ago, such as an amputation stump, is a natural consequence of the plasticity of the nervous system. An understanding of the physiological basis of pain is helpful to the sufferer, and the professionals who have to provide appropriate treatment. It must be stated at the outset that in humans pain is invariably associated with pain behavior and pain generally results in some degree of suffering. Nociception, neuropathy or psychological and environmental factors may singly, or in combination, result in pain. As evidence continues to accumulate concerning the role of central sensitisation in post-operative pain, many researchers have followed methods to prevent central neuropathic changes from occurring, through the utilization of pre-emptive analgesic techniques. Effective preventive analgesic technique may not only be useful in reducing the acute pain, but also chronic post-surgical pain and disabilities. Pre-emptive analgesia3,4,5 is an attractive concept of addressing pain even before it starts. The concept was propounded in the early 1980s when experimental studies showed that measures to antagonize the nociceptive signals before injury, prevented central hypersensitisation, thereby reducing the intensity of pain following the injury. Transmission of pain signals evoked by tissue damage leads to sensitization of the peripheral and central pain pathways. Pre-emptive analgesia is a treatment that is initiated before the surgical procedure in order to reduce this sensitization. The only way to prevent sensitization of the nociceptive system might be to block completely any pain signal originating from the surgical wound from the time of incision until final wound healing. It refers to the administration of an analgesic before a painful stimulus, such as tissue injury during surgery, in an attempt to obtain better pain relief compared with when the same analgesic intervention is used after the painful stimulus. Pre-emptive analgesia is known to prevent central sensitization of pain, thereby reducing hyperalgesia. There is also the "wind-up" phenomenon which causes persistent spontaneous pain even in the absence of peripheral stimuli. Paracetamol is an effective analgesic and an antipyretic agent6,7. The efficiency and tolerability for intravenous Paracetamol are well established. It has a favourable safety profile and it is the most commonly prescribed drug for the treatment of mild to moderate pain. The mechanism of action includes inhibition of a central nervous system COX-2, inhibition of a putative central cyclooxygenase 'COX-3' that is selectively susceptible to paracetamol, and modulation of inhibitory descending serotinergic pathways. Paracetamol has also been shown to prevent prostaglandin production at the cellular transcriptional level, independent of cyclooxygenase activity. Paracetamol acts on both the peripheral and central component of pain pathway with cellular proteins and nucleic acids causing irreparable damage. Atef A et al.8 performed a prospective placebo-controlled study to evaluate the analgesic efficacy and safety of intravenous paracetamol in patients undergoing elective standard bipolar diathermy tonsillectomy and concluded that intravenous paracetamol significantly reduced pethidine consumption over a 24-hour period. The present study also compared the analgesic efficacy and tolerability of IV Paracetamol where in, the administration of 15mg/kg of paracetamol IV provided analgesia upto 6 hours in the post-operative period which was superior to placebo in managing postoperative pain. Alhashemi JA et al.9 compared IV Acetaminophen with IM Meperidine with regard to analgesic effects in paediatric patients undergoing tonsillectomy and concluded that compared with IM Meperidine, IV Acetaminophen provided adequate analgesia, less sedation and earlier readiness for recovery room discharge among paediatric patients undergoing tonsillectomy. In the present study, IV Paracetamol produced acceptable sedation in the post-operative period without any compromise to the airway. Alhashemi JA et al.10 from his study revealed that IV Acetaminophen resulted in slightly higher pain scores than IM Meperidine but earlier readiness for recovery room discharge in paediatric patients undergoing dental restoration. In the current study, IV Paracetamol had better recovery profile as compared to placebo and better pain relief with no adverse effects. C Remy, E Marret, F Bonnet, et al.11 in their study analyzed the effect of paracetamol on morphine side-effects and consumption after major surgery and concluded that paracetamol combined with PCA induced a significant morphine sparing effect. Ahmed AI Fadly et al.12 studied the analgesic effect of IV paracetamol, morphine and their combination for post-operative pain after release of post burn neck contractures and concluded that IV Paracetamol effectively reduces morphine requirements by 60% or even replaces it with less incidence of adverse events and more safer course during postoperative pain management after release of post burn neck contracture in adults. The present study also unveiled the fact that there were no adverse events and the time to first rescue analgesia was significantly longer in the paracetamol group as compared to the placebo group with mean duration of pain relief upto a period of 6 hours. Murat-et al.13 evaluated the relative analgesic efficacy of paracetamol with propacetamol for 6 hours after inguinal hernia repair under GA with ilioinguinal block in children. They concluded that a single infusion of IV Paracetamol 15 mg/kg provides analgesia similar to single infusion of propacetamol 30 mg/kg following inguinal hernia repair in children. Iolter Cattabriga et al.14 studied the efficacy of IV paracetamol as an adjunctive analgesic to a tramadol-based background analgesia after cardiac surgery and concluded that in patients undergoing cardiac surgery, intravenous paracetamol in combination with tramadol provides effective pain control. But in the present study, the postoperative pain was evaluated by visual analog scale and a rescue dose of 1.5 mg/kg of i.m diclofenac was administered whenever the VAPS score was greater than 4. Here IV paracetamol provided effective pain control in the post operative period upto a period of 6 hours. In the present study, the mean pulse rate at 0 - 6 hours in the post operative period for P group was significantly lower than the N group (P <0.001). The mean MAP at 0 - 6 hrs in the post operative period was significantly higher in N group than P group (P < 0.001). These statistics explain the analgesic efficacy of paracetamol which resulted in a stable hemodynamic status. Thus IV Paracetamol produced a better haemodynamic profile in the post-operative period.
CONCLUSION ‘Your pain is the breaking of the shell that encloses your understanding’ - Khalil Gibran Intravenous Paracetamol can be used as an effective analgesic for providing pre-emptive analgesia. It provides excellent post operative pain relief and has a better hemodynamic profile and is safe for use in patients.
REFERENCES
Policy for Articles with Open Access Authors who publish with MedPulse International Journal of Anesthesiology (Print ISSN:2579-0900) (Online ISSN: 2636-4654) agree to the following terms: Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution License that allows others to share the work with an acknowledgement of the work's authorship and initial publication in this journal. Authors are permitted and encouraged to post links to their work online (e.g., in institutional repositories or on their website) prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work.
|
|
 Home
Home