|
Table of Content - Volume 14 Issue 2 - May 2020
Effect of dexmedetomidine on sedation and analgesia in supraclavicular brachial plexus block in children - A prospective Randomized, double blinded study
Subhashree J1*, Rajasekhar T2, Pradeep Kumar K3, Subrahmanyam G4
1,2Assistant Professor, 3Associate Professor, 4Civil Assistant Surgeon, Department of Anesthesiology, BIRRD(T) Hospital, Tirupati, Andhra Pradesh. 517501, INDIA Email: drswapnaa@gmail.com, drrajasekharr@gmail.com, drpradeep9@gmail.com, gutamsubramanyam@gmail.com
Abstract Background: Brachial plexus block is a well-accepted technique in children for upper limb procedures. Several adult human studies have concluded the superiority of dexmedetomidine as an adjuvant to local anesthetic during brachial plexus block. But similar evidence is lacking in pediatric population. Thus we conducted this prospective, randomized, double blind clinical efficacy study to evaluate the effectiveness of adding dexmedetomidine to bupivacaine in supraclavicular brachial plexus block in children, in terms of duration of analgesia, intraoperative sedation and postoperative analgesic requirement. Methodology: After institutional ethics committee approval and obtaining written informed consent from the parents, hundred children of age 1-12years, posted for elective upper limb orthopedic surgery, were randomly allocated into two groups of 50 each. All the children were premedicated with ketamine (4mg/kg) and glycopyrolate (0.2mg) IM 15 minutes prior to shifting inside the operation theatre. The children received 0.25%bupivacaine (1ml/kg) along with either 1ml saline (control group) or 1µg/kg of dexmedetomidine (study group) as per their group and brachial plexus block was given using classical supraclavicular approach. Heart rate, blood pressure and peripheral oxygen saturation were noted every 5min for first 30 minutes and then every 15minutes till the end of the procedure. Results: Demographic data and hemodynamic parameters were comparable between the groups. However there was significant statistical difference in the duration of analgesia in the study group (p value < 0.001) and also required less intraoperative sedation and less postoperative analgesia ( p value < 0.001) than the control group. Congenital anomalies like syndactyly, radial and ulnar club hand, constriction band syndrome are common in pediatric population. Key Word: supraclavicular brachial plexus block.
INTRODUCTION Brachial plexus block is a well-accepted technique in children for upper limb procedures. Several adult human studies have concluded the superiority of dexmedetomidine as an adjuvant to local anesthetic during brachial plexus block. But similar evidence is lacking in pediatric population. Thus we conducted this prospective, randomized, double blind clinical efficacy study to evaluate the effectiveness of adding dexmedetomidine to bupivacaine in supraclavicular brachial plexus block in children, in terms of duration of analgesia, intraoperative sedation and postoperative analgesic requirement.
METHODOLOGY This prospective, randomized, double blinded clinical efficacy study was conducted to evaluate the effectiveness of adding dexmedetomidine to bupivacaine in supraclavicular brachial plexus block in children, in terms of duration of analgesia, intraoperative sedation and postoperative analgesic requirement. After obtaining institutional ethics committee approval, written informed consent was obtained from the parents, after explaining about the procedure, its benefits and complications. Hundred children of aged 1-12years, belonging to ASA PS1,2, posted for elective upper limb orthopedic surgery of duration less than 2hours were included in the study. Parents who did not give consent and any patient with history of coagulation abnormalities were excluded from the study. All the children were kept fasting for 6hours for solids and 2hours for clear liquids, breast feeding was allowed up to 4hours before surgery. These children were randomly allocated into two groups of 50 each. children <6years of age were premedicated with ketamine (4mg/kg) and glycopyrolate (0.2mg) IM 15 minutes prior to shifting inside the operation theatre. Once they were sedated, they were shifted to operation theatre, monitors like saturation probe, noninvasive blood pressure monitor, and electrocardiogram were connected and Intravenous cannula was secured. For older kids, EMLA cream was applied on the dorsum of the hand or the foot in the preoperative area 30 minutes before shifting to operation theatre. After shifting to the operation theatre, monitors were connected and intravenous cannula was secured. Inj.ketamine 1-2mg/kg and glycopyrolate 0.2mg iv was given. Oxygen was given through facemask at 4l/min for all the children. Resuscitation equipments like laryngeal mask airway, tracheal tubes, and drugs required to convert the anesthetic technique to general anesthesia like propofol, neuromuscular blocking agents were loaded and kept ready. All the blocks were given by senior anesthesiology consultant in the operation theatre, who was blinded to the drug given. Supraclavicular block was performed using anatomical landmark approach; child was positioned in supine, with head ring and shoulder roll. Ipsilateral shoulder was pulled towards the feet to keep the clavicle horizontal. Area was painted with 2%betadine and draped. Under sterile aseptic precautions, midpoint of clavicle and transverse process of C6 tubercle (chassaignac’s tubercle) {if not identified, then line from the cricoid cartilage to the posterior border of sternocleidomastoid} were identified. A 23G, 2.5cm hypodermic needle with syringe attached was used. Point of needle insertion was the junction of middle and lateral third of clavicle’s midpoint and chassaignac’s tubercle. Skin weal was raised and the needle was directed downwards, backwards and medially until contact was made with the first rib. No conscious effort was made to elicit paraesthesia. Needle was withdrawn by a millimetre, and then the drug was injected after negative aspiration for blood and air, thereby ruling out the accidental injection into blood vessel or pleural puncture. The children received 0.25%bupivacaine (1ml/kg) along with either 1mL saline (control group- group A) or 1µg/kg of dexmedetomidine diluted to 1mL (study group – group B) as per their group. Heart rate, blood pressure and peripheral oxygen saturation were noted every 5min for first 30minutes and then every 15minutes till the end of the procedure. Sensory loss was assessed using needle in the areas supplied by ulnar, median, radial and musculocutaneous nerves. Motor block was assessed based on the inability to move the limb during the pneumatic tourniquet inflation and during surgical incision and the block was considered successful if there was no pain or movement during the same. General anesthesia was administered if the child started moving vigorously or complained of pain during tourniquet inflation or surgical incision and the child was excluded from the study. Midazolam 1mg IV bolus was used to sedate the child in the intraoperative period, aimed at maintaining Ramsay sedation score of 3-4. Total dose of midazolam given during intraoperative period was noted. Child was observed for any complications like bradycardia, hypotension, pneumothorax and haematoma formation and was treated accordingly. Once the surgery was over, then the child was shifted to postoperative unit and observed for 12hours. In the postoperative period, pain and sedation was assessed using CHEOPS scale. Rescue analgesia with inj.fentanyl 1µg/kg was given when CHEOPS scale was more than 6 and the total dose required in the first 12hours of postoperative period was also noted 20,21. Oral liquids were started 3hrs after receiving in the postoperative period. After starting oral food, a combination syrup of paracatemol and ibugesic (each 5ml of suspension has 100mg of ibuprofen and 162.5mg of paracatemol in a flavored syrup base, dose based on the child’s age)was started every 8th hourly. Duration of block was defined by the time between the block given and the time during which child had a CHEOPS score of more than 6 for the first time.
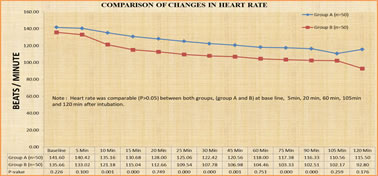
RESULTS Statistical analysis was done using SPSS software, version 15. Demographic and hemodynamic data were compared using student’s t test. Duration of analgesia, sedation and analgesic dose requirement were compared using unpaired t test. p value < 0.05 is considered statistically significant and p value < 0.001 as statistically very significant. Demographic data (age, sex, body weight) were comparable between two groups. Heart rate was comparable (p>0.05) between both groups, (group A and B) at base line, 5min, 20 min, 60 min, 105min and 120 min after block (figure 1).
Figure 1: changes in the heart rate between the groups.
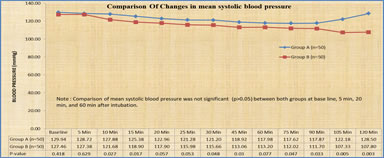
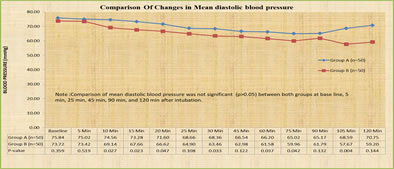
Mean systolic (figure 2), diastolic blood pressure (figure 3), at baseline, 5min, 10min, 15min, 30min, 45min, 60min, 75min, 90min, 105min and 120min were comparable between the groups (p>0.05). Figure 2: changes in mean systolic blood pressure between the groups
Figure 3: Changes in mean diastolic blood pressure
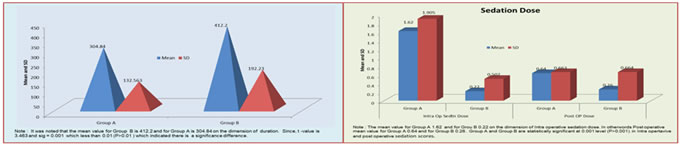
Duration of the surgery and oxygen saturation level was comparable between the groups. Duration of analgesia was higher in study group (group B) 419.20 ± 192.230 (mean ± SD) than the control group (group A) 304.84± 132.563 ( mean ± SD ) with p value < 0.001,which is statistically very significant (figure 4). Sedation dose used in the intraoperative period was lesser in the study group (group A) .22± .507 than the control group 1.62± 1.905 (mean ± SD) with p value less than 0.001. Total analgesic dose used in the first 12hours of postoperative period was lesser in study group 26 ± .664 than the control group 64± .66 (mean ± SD) with p value less than 0.001, which is statistically very significant (figure 5). No adverse effects like bradycardia, hypotension were noted in both the groups. One patient in group A and two patients in group B had failed block, were converted to general anesthesia with laryngeal mask airway and were excluded from the study.
DISCUSSION Regional anesthetic techniques, especially supraclavicular brachial plexus block is well documented technique in children undergoing upper limb surgeries16-18. Drugs like clonidine, dexamethasone, and dexmedetomidine have been used as adjuncts to local anesthetics in peripheral nerve blockade6-11. Among all these drugs, dexmedetomidine, which is often used for procedural sedation and in ICU9, is gaining popularity as an adjunct to local anesthetic, because of its selective alpha2 blockade12,14. Several studies in adult population have concluded the superiority of dexmedetomidine as an adjunct to local anesthetic in peripheral nerve blockade. But there is not much literature regarding the use of dexmedetomidine as an additive in brachial plexus blockade in children. Thus we had conducted a prospective, randomized, double blinded study to study the effect of adding dexmedetomidine to bupivacaine in supraclavicular block on the duration of analgesia, intraoperative sedation requirement and need of rescue analgesia in the postoperative period. Regional techniques in children4 are often considered as a challenge to anesthesiologists for two main reasons: 1. Younger children need sedation to let the anesthesiologists to perform a block, which itself might interfere in assessing the sensory and motor blockade in sedated children. Till now there is no standard technique to assess the efficacy of block in sedated children. 2. Older children who might cooperate to an anesthesiologist to give a block, but most of the times they may not cooperate in eliciting paresthesia, which often might result in mental trauma to the children in the postoperative period. In this study, we did not make an effort to elicit paresthesia. Instead we stick to the classical anatomical landmarks approach, we had deposited over the first rib and the success rate of the block in our study > 97 %. We attribute the success to the distribution of local anesthetic to the compact brachial plexus sheath over the first rib. As there is no standard technique to assess the motor and sensory blockade in sedated children, general anesthesia was induced if the patient started moving vigorously on tourniquet inflation or during the skin incision. Various techniques of brachial plexus block through axillary and interscalene approach have been suggested for upper limb procedures 23. We followed supraclavicular method because of our familiarity with the technique, and its ability to produce dense blockade with less complications.22,26,27 Interscalene approach has its own complications like cervical plexus block, phrenic nerve blockade 24,25, and musculocutaneous nerve can get spared in axillary approach23. Pande et al 15 used supraclvicular block technique as a sole anesthetic technique in 200 children, undergoing closed reduction of arm fractures. They had used 1.5% lignocaine with epinephrine as the block drug and have found that classical supraclavicular brachial plexus block as an acceptable, effective method with good success rate. We have used 0.25% bupivacaine with dexmedetomidine as the surgery proposed is of longer duration around 2hours. Sandhya et al 8 have used dexmedetomidine in the dose of 100µg as an additive with 0.325% bupivacaine in supraclavicular brachial plexus block in adult population. They have concluded that dexmedetomidine shortens the onset and prolongs the duration of block with adequate sedation. In our study, we have used dexmedetomidine in the dose of 1µg/Kg as an additive with 0.25% bupivacaine and we have found that it increases the duration of analgesia, reduces the sedation requirement in the intraoperative period and analgesic requirement in the postoperative period. We did not observe any bradycardia or hypotension in the perioperative period.
CONCLUSION Dexmedetomidine as an additive to bupivacaine in supraclavicular block in pediatric population prolongs the duration of analgesia with adequate intraoperative sedation and with lesser need of rescue analgesics in the postoperative period.
REFERENCES
|
|
 Home
Home