|
Table of Content - Volume 14 Issue 2 - May 2020
Efficacy of injection clonidine in attenuation of haemodynamic response to laryngoscopy and orotracheal intubation
Bhagyashri Soor1*, Suhas Jewalikar2
1Senior Resident, Department of Anaesthesiology, Seth G S Medical College & KEM Hospital, Mumbai, Maharashtra, INDIA. 2Professor & HOD, Department of Anaesthesiology, Government Medical College, Aurangabad, Maharashtra, INDIA.
Abstract Background: Laryngoscopy and tracheal intubation are commonly accompanied by increase in arterial blood pressure and heart rate. The principle mechanism is the sympathetic response, which may be the result of increase in catecholamine activity. Aims and objective: To study the efficacy of intravenous Clonidine 1 µg/kg in attenuation of haemodynamic response to orotracheal intubation and laryngoscopy and observe side effects of Inj. Clonidine if any. Material and method: The present study was carried out on 60 patients in the age group of 20-60 years of ASA grade I and II posted for elective surgery under general anesthesia. They were randomly divided in two groups of 30 patients each, received Inj. Clonidine 1 µ/kg iv (group A) and inj normal saline iv as placebo (group B) diluted to 10 ml given 10 minutes prior to induction. We compared both groups for changes in HR, SBP, DBP, MAP, SpO2, ECG ( lead V5) when the patient was shifted to OT , 5 minutes after IV Clonidine , at induction , at intubation , 1 minute after intubation , 3 minutes after intubation , 5 minutes after intubation , 10 minutes after intubation. Result: Mean heart rate, systolic blood pressure, diastolic blood pressure mean arterial pressure significantly fall down after intubation compared to baseline value in group A whereas increased compared to baseline value in group B. Conclusion: Clonidine at a dose of 1 μg/kg attenuates the haemodynamic responses to laryngoscopy and orotracheal intubation with minimal side effects like bradycardia. Keywords: Clonidine, haemodynamic response, laryngoscopy, orotracheal intubation
INTRODUCTION Laryngoscopy and tracheal intubation are commonly accompanied by increase in arterial blood pressure and heart rate1. The principle mechanism in this hypertension and tachycardia is the sympathetic response2,, which may be the result of increase in catecholamine activity3. Transitory hypertension and tachycardia are probably of no consequence in healthy individuals. But either or both may be hazardous to those with hypertension, myocardial insufficiency and cerebrovascular diseases3. This laryngoscopic reaction in such individuals may predispose to development of pulmonary edema, dysrhythmias, myocardial insufficiency and cerebrovascular accident4. Intravenous anaesthetic induction agents do not adequately or predictably suppress the circulatory responses evolved by endotracheal intubation5. So prior to initiating laryngoscopy, additional pharmacological measures like use of volatile anaesthetics6, topical and intravenous lidocaine7, opioids8, vasodilators–SNP (Sodiumnitroprusside)9, NTG(Nitroglycerine)10, Calcium channel blockers 11 and β-blockers 12, have been tried by various authors. Besides minimizing the cardiovascular response, anaesthesia induction for patients at risk must also satisfy the following requirements: it must be applicable regardless of patient group, prevent impairment of cerebral blood flow and avoid awareness of the patient, it should neither be time consuming nor affect the duration or modality of the ensuing anaesthesia and also should not have any effect on the recovery characteristics. Among the recommended procedures, intravenous Clonidine appears to fulfill the criteria13. Intravenous Clonidine, a central α–2 agonist has become a popular agent for obtunding haemodynamic responses to laryngoscopy and intubation. Further clonidine has sedative, analgesic, antihypertensive actions in addition to reducing the anesthetic drugs requirement13. Not many studies have been done in India using Clonidine in the parenteral form for suppression of intubation response. Hence, we studied the effects of intravenous Clonidine for attenuation of haemodynamic responses to laryngoscopy and orotracheal intubation.
MATERIALS AND METHODS STUDY DESIGN: Prospective randomized double blind clinical study. STUDY APPROVAL: Study was approved by Institutional Medical Ethical Committee. Written informed valid consent was obtained from all patients participating in the study. STUDY POPULATION: Sixty patients of either sex, between 20-60 years of age of ASA Grade I and II scheduled for surgery under General Anaesthesia at Govt. Medical College and hospital, Aurangabad were studied. Group A (30) in which patients received Inj. Clonidine 1 µ/kg IV diluted in 10 ml normal saline 10 minutes prior to induction. Group B (30) in which patients received 10 ml normal saline IV 10 minutes prior to induction. INCLUSION CRITERIA: ASA Grade I and II , Age 20 -60 years of both sex, Weight between 40 -60 kg, patients posted for elective surgical procedure requiring general anaesthesia, patients with written, valid and informed consent,MPC Grade I and II EXCLUSION CRITERIA: Patient refusal to participate in the study, ASA Grade III and IV, pregnant patients, Patients on beta blocker drugs, patients with cardiovascular disorders, Patient suffering from renal disease, patients of COPD and with recent history of URTI, drug or alcohol abuse, patients with anticipated difficult intubation (MPC Grade III and IV), patient in whom time required for intubation exceeded 15 seconds and more than one attempt of intubation Patients scheduled for elective surgeries under general anaesthesia were thoroughly evaluated and assessed preoperatively for inclusion in the study. Preanaesthetic evaluation comprising of history of previous medical and surgical illnesses, previous anaesthesia exposures, drug allergies along with general, physical examination , airway assessment was done by Mallampati grading to anticipate the possibility of difficult intubation. Basic blood investigations of Haemoglobin, Complete blood counts, Liver function test, PT(INR), Bleeding time, Clotting time, Urine analysis, Renal function test, Electrolytes, radiograph of Chest, Electrocardiogram were performed. Other investigations if indicated were carried out.On the day of surgery patients NBM status was confirmed. Patient was taken inside the operation theatre, an intravenous (IV) line was secured with angiocatheter number 18 gauge on nondominant hand. Monitoring was continued using pluse-oximeter, noninvasive blood pressure monitor, ECG lead V was recorded. After intubation carbon dioxide monitoring along with agent analyzer were attached. Preinduction heart rate and blood pressure recording were taken. Preloading was done with Ringer Lactate 10 ml/kg. All patients were premedicated with tab. Diazepam 5 mg and tab. Ranitidine 150 mg night before surgery. All patients were premedicated with inj. Midazolam 0.03 mg/kg IV and inj. Ondansetron 0.08 mg/kg IV before induction. Patients of group A received inj. Clonidine 1 µg/kg diluted in 10ml normal saline 10 minutes before induction and Patients of group B received intravenous 10 ml normal saline 10 minutes before induction. Then they were preoxygenated for 5 min with 100% oxygen. General anaesthesia was induced in patients with injection Thiopentone Sodium 6mg/ kg IV until loss of eye lash reflex. Intubation facilitated with inj. Vecuronium 0.1 mg/kg. All patients were ventilated with 100% oxygen at the rate of 10-12 L/min until intubation after administration of injection Vecuronium IV for 3 minutes. Direct laryngoscopy was done and patient was intubated by expert anaesthesiologist within 15 seconds with proper size of endotracheal tube. Anaesthesia was maintained with oxygen 50% , nitrous oxide 50%, and isoflurane . Muscle relaxation was maintained using injection Vecuronium IV. Patients were monitored throughout the surgical procedure with pulse-oximeter, noninvasive blood pressure monitor and ECG lead V. Haemodynamic responses were compared in both groups by measuring HR, SBP, DBP, MAP, SpO2, ECG ( lead V5). Basal reading when the patient was shifted to OT (T0), 5 minutes after IV Clonidine (T1), at induction (T2), at intubation (T3), 1 minute after intubation (T4), 3 minutes after intubation (T5), 5 minutes after intubation (T6), 10 minutes after intubation( T7 ). Isoflurane concentration was adjusted to maintain systolic B.P. within 20% of preoperative values. Heart rate <60 beats/ minutes was managed by inj. Atropine 0.6 mg IV. Mean Arterial Pressure< 60 mm Hg was managed with fluid challenges and Inj. Mephentermine 6 mg bolus IV and incremental doses if required. Upon completion of surgery, neuromuscular block was reversed with inj. Neostigmine and inj. Glycopyrrolate IV and patient was extubated. STATISTICAL METHOD EMPLOYED: All quantitative data was presented as mean ±SD (standard deviation). Quantitative data was analyzed by Student’s t test. p<0.01- Statistically highly significant (HS) p<0.05- Statistically significant (S) p>0.05- Statistically not significant (NS) The statistical software SPSS version was 23.0, used for the analysis of the data and Microsoft Word and Excel was used to generate graphs, tables etc.OBSERVATIONS AND RESULTS Both the groups were comparable in terms of age,sex,weight,ASA grading
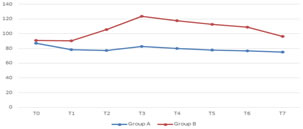
Graph 1: Comparison between the groups according to Heart Rate (bpm) Graph 1 shows that the baseline heart rate was comparable in both groups (p=0.233). In group A (Clonidine), the baseline mean HR was 87.33 ±14.868 bpm. Mean HR after intubation at 0 minute, 1 minute, 3 minutes, 5 minutes and 10 minutes were 82.57± 9.765, 80.30±9.200, 77.97±8.946, 76. 80±9.499, 75.30±8.879 bpm respectively. Thus there was significant fall in mean HR after intubation compared to baseline value and this was statistically highly significant. (P=0.0001) In group B the baseline mean HR was 91.13±8.842 bpm. Mean HR after intubation at 0 minute, 1 minute, 3 minutes, 5 minutes, and 10 minutes were 123.60±9.350, 117.77±7.555, 112.77±7.257, 109.23±6.725, 96.63±8.160 bpm respectively. Thus there was a statistically significant increase in HR (P=0.000) compared to baseline value.
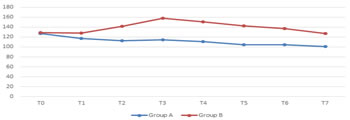
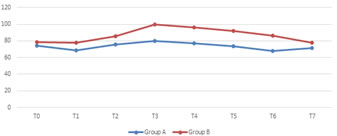
Graph 2: Comparison between the groups according to Systolic BP (mmHg) Graph 2 shows that the baseline SBP was comparable in both groups. In group A (Clonidine), the baseline SBP was 127.40 ±11.752 mmHg. The mean SBP after intubation at 0 minute ,1 minute, 3 minutes, 5 minutes and 10 minutes were 114.30±9.333, 111.10±9.007, 104.30±17.117, 104.23±10.897, 101.90±8.814 mmHg respectively. It showed significant fall in SBP after intubation compared to baseline value and this was statistically highly significant. In group B the baseline SBP was 129.00±6.465 mmHg. SBP after intubation at 0 minute, 1 minute, 3 minutes, 5 minutes and 10 minutes, were 158.07±4.378, 150.37±4.460, 142.57±5.643, 137.13±7.820, 126.80±6.261 mmHg respectively. There was statistically significant increase in SBP at 0 minute, 1 minute, 3 minutes and 5 minutes whereas negligible decrease after 10 minutes compared to baseline value. Graph 3: Comparison between the groups according to Diastolic BP (mmHg) Graph 3 shows that the baseline DBP was comparable in both groups (P value - 0.008). In group A (clonidine), the baseline DBP was 74.47±4.493 mmHg. The DBP after intubation at 0 minute, 1 minute, 3 minutes, 5 minutes and 10 minutes were 80.10±9.841, 77.17±8.667, 73.77±7.290, 67.97±7.695, 71.63±8.032 mmHg respectively. There was significant fall in DBP after intubation compared to baseline value and this was statistically highly significant. In group B the baseline DBP was 78.43±6.252 mmHg. DBP after intubation at 0 minute, 1 minute, 3 minutes, 5 minutes and 10 minutes were 99.40±4.430, 96.30±4.935, 92.03±5.282, 86.47±7.262, 78.07±6.838 mmHg respectively. After intubation there was statistically significant increase in DBP (P<0.01) compared to baseline value.
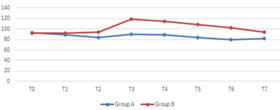
Graph 4: Comparison between the groups according to Mean Arterial pressure (mmHg) Graph 4 shows that the baseline mean arterial pressure was comparable in both groups (p=0.2842). In group A (clonidine), the baseline MAP was 93.03±3.746 mmHg. The MAP after intubation at 0 minute, 1 minute, 3 minutes, 5 minutes and 10 minutes were 90.00±6.192, 88.47±7.507, 83.94±7.804, 79.30±4.260, 81.63±7.717 mmHg respectively. It showed significant fall in mean BP after intubation compared to baseline value and this was statistically highly significant. In group B the baseline mean arterial pressure was 91.94±3.53 mmHg. MAP after intubation at 0 minute, 1 minute, 3 minutes, 5 minutes and 10 minutes were 118.53±4.058, 114.32±4.281, 108.88±4.777, 102.80±6.462, 94.13±5.144 mmHg respectively. This showed after intubation there was a statistically significant increase in mean BP (P<0.01) compared to baseline value.
DISCUSSION Most of the general anaesthesia procedures in the modern anaesthetic practice are carried out with endotracheal intubation. Laryngoscopy and tracheal intubation are considered as the most critical events during administration of general anaesthesia. Laryngoscopy and tracheal intubation provoke transient but marked sympathoadrenal response leading to hypertension and tachycardia1. In our study the patients in all the groups did not show any statistically significant differences in their age, sex or weight distribution HEART RATE In our study there was decrease in heart rate after intubation in group A and increase in heart rate in group B. The basal mean HR in the present study group and control group were 87.33 bpm and 91.13 bpm respectively. There was increase in heart rate in group B, 123.60±9.350, 117.77±7.555, 112.77±7.257, 109.23±6.725, 96.63±8.160 bpm at 0 minute, 1 minute, 3 minutes, 5 minutes, and 10 minutes after intubation respectively, Whereas decrease in heart rate in group A were 82.57±9.765, 80.30±9.200, 77.97±8.946, 76.80±9.499, 75.30±8.879 bpm at 0 minute, 1 minute, 3 minutes , 5 minutes and 10 minutes after intubation respectively. In group A, there was significant decrease in heart rate by 5, 7, 9, 11, 12 beats per minute at 0 minute,1 minute, 3 minutes, 5 minute, 10 minutes respectively after intubation. Where as in control group B, heart rate increased by 32, 26, 22, 18, 6 beats per minute at 0 minute, 1 minute, 3 minutes, 5 minutes, 10 minutes after intubation respectively. U.A Carabine et al.25 used 1.25 µg/kg and 0.625 µg/kg IV Clonidine and noted that the degree of tachycardia was significantly lower at induction (p<0.01) and intubation (p<0.05) with 1.25 µg/kg, but one patient developed bradycardia of 45 beats/minute. While with 0.625 µg/kg the significantly lower rate was noted from intubation for 3 minutes period (p<0.05).Deepshikha C Tripathi et al. (2011)28 used 1 µg/kg and 2 µg/kg IV Clonidine in 100 ml normal saline 30 min before induction found that heart rate decrease at intubation but not more than 20% of baseline with 1 µg/kg (p<0.05). While with 2 µg/kg IV Clonidine heart rate decrease was more than 20% from baseline. Sakshi Arora et al.34 used 1 µg/kg and 2 µg/kg IV Clonidine with fentanyl 2 µg/kg and found decrease in heart rate at laryngoscopy and intubation by 2.81% below base line (P<0.05) with 1 µg/kg and by 8.1% below base line with 2 µg/kg. Similar to U.A Carabine et al., Deepshikha C Tripathi et al., Sakshi Arora et al. we found decrease in heart rate at intubation compared to baseline with 1 µ/kg Clonidine IV. Zalunardo MP. et al. 91 noted that the plasma catecholamine concentration increased to the maximum at 1 minute after the laryngoscopy. The decrease in the pulse rate after the Clonidine administration was due to the reduction of the sympathetic outflow, the simultaneous increase of the parasympathetic tone of central origin and the influence of Clonidine on the neurons which receive the baroreceptor afferents42. BLOOD PRESSURE In our study, decrease in systolic blood pressure after intubation was seen in group A and increase in systolic blood pressure seen in group B .The basal mean SBP in the present study group and control group were 127.40 mmHg and 129.00 mmHg respectively. There was increase in SBP in groupB, 158.07±4.378, 150.37±4.460, 142.57±5.643, 137.13±7.820, 126.80±6.261 at 0 minute, 1 minute, 3 minutes, 5 minutes and 10 minutes after intubation respectively, Whereas decrease in SBP in group A were 114.30 ± 9.333, 111.10±9.007, 104.30±17.117, 104.23±10.897, 101.90±8.814 mmHg at 0 minute, 1 minute, 3 minutes, 5 minutes and 10 minutes after intubation respectively. In group A there was significant decrease in SBP by 13, 16, 24, 24, 26 mmHg at 0 minute, 1 minute, 3 minutes, 5 minutes, 10 minutes respectively after intubation. Where as in control group B, SBP increased by 29, 21,13, 8 mmHg at 0 minute,1 minute, 3 minutes, 5 minutes after intubation respectively. In our study, diastolic blood pressure in group A was increased from baseline by 6, 3 mmHg at 0 minute and 1 minute after intubation, then decreased by 1, 7, 3 mmHg at 3 minutes, 5 minutes and 10 minutes respectively. Where as in control group B, DBP increased by 21, 18, 14, 8 mmHg at 0 minute, 1 minute, 3 minutes, 5 minutes after intubation. At 10 minutes DBP was equal to baseline.In our study, mean arterial pressure in study group A decreased from baseline by 3, 5, 10, 14, 11 mmHg at 0 minute, 1 minute, 3 minutes, 5 minutes, 10 minutes respectively. Whereas in control group B, it increased by 26, 22, 16, 10, 2 mmHg at 0 minute, 1 minute, 3 minutes, 5 minutes, 10 minutes respectively. U.A Carabineet al.25 used 1.25 µg/kg, 0.625 µg/kg IV Clonidine, normal saline and noted that in all three groups MAP increased significantly on laryngoscopy and intubation. Compared to control group, MAP remained significantly lower in groups with 1.25 µg/kg and 0.625 µg/kg from induction and intubation, continuing to 5 minutes after intubation. Similarly, Deepshikha C Tripathi et al. (2011)28, SakshiArora et al.34 found that with 1ug/kg SBP, DBP and MAP decreased from baseline after intubation.Though, various studies found intravenous clonidine effective in attenuating the haemodynamic changes during laryngoscopy and intubation, there is wide difference in the dose of clonidine used. Harshavardhana H.S.et al.30, Irfan Waris.et al.35, Narayan Acharya et al.37 used 3 ug/kg IV Clonidine in attenuating haemodynamic response during intubation and Sameenakousar et al.32, Dr. Rushikesh C Desai et al.36, Vinay Marulasiddappa et al. 39 used 2 ug/kg IV Clonidine effectively attenuated the heart rate response and also arterial pressure response to laryngoscopy and intubation. They did not find any adverse effect in perioperative period, though they felt the need of further research to determine the ideal dose of clonidine required. This study was planned with the objective of determining the minimum dose (1 ug/kg) which is safe and effective as premedication in attenuating haemodynamic response during laryngoscopy and orotracheal intubation. A decrease in sympathetic tone by central action and presynaptically mediated inhibition of norepinephrine and vagomimetic action at nucleus tractus solitarius by clonidine is responsible for bradycardia. Three patients out of 30 patients in our study group had bradycardia <45 beats/minutes and it was managed by inj. Atropine 0.6 mg IV while none in control group had bradycardia. No significant ECG changes were found in both the groups. Hypotension, nausea, vomiting, dryness of mouth were not observed. The results of the present study should encourage the routine use of clonidine as a premedication for the patients who undergo laryngoscopy and intubation as it provides-
CONCLUSION Clonidine at a dose of 1 μg/kg body weight diluted in 10 ml Normal saline given 10 minutes before induction significantly attenuates the haemodynamic responses to laryngoscopy and orotracheal intubation with minimal side effects like bradycardia. However, the study has to be done on a larger population and in high risk patients for further evaluation.
REFERENCES
Policy for Articles with Open Access Authors who publish with MedPulse International Journal of Anesthesiology (Print ISSN:2579-0900) (Online ISSN: 2636-4654) agree to the following terms: Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution License that allows others to share the work with an acknowledgement of the work's authorship and initial publication in this journal. Authors are permitted and encouraged to post links to their work online (e.g., in institutional repositories or on their website) prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work.
|
|
 Home
Home