|
Table of Content - Volume 14 Issue 3 - June 2020
Segmental spinal vs general anaesthesia in patients undergoing laparoscopic cholecystectomy: A comparative study
Naresh Wamanrao Paliwal1, Jayesh Ingle2*, Sunil Lawhale3, Amol Dhakulkar4
1Associate Professor, 2Assistant professor, 3Professor and HOD, 4Sr Resident, Department of Anesthesiology, Dr. P. D. M. Medical College, Amravati, Maharashtra, INDIA. Email: drjayeshingle@gmail.com
Abstract Background: Since a new era of studies on segmental spinal anaesthesia puncturing subarachnoid space at T10 for laparoscopic cholecystectomy started to anaesthetize a patient with severe obstructive lung disease in 2006 there have been many studies about segmental spinals exploring its utility in many different surgical procedures like awake thoracoscopic or thoracic surgeries, laparoscopic cholecystectomy and breast surgeries. Segmental Spinal anaesthesia is reported to be having excellent results in terms of post-operative pain, analgesia requirement, relatively less complications and reduced hospital stay. We conducted this comparative study to compare segmental spinal anaesthesia and general anaesthesia for cholecystectomy. Materials and Methods: This was a comparative study in which 60 patients belonging to ASA I and II and undergoing laparoscopic cholecystectomy were included on the basis of a predefined inclusion and exclusion criteria. A detailed history was taken and a thorough clinical examination was done in all the cases. Preanesthetic evaluation was done. P value less than 0.05 was taken as statistically significant. Results: Out of 60 patients there were 42 (70%) females and 18 (30%) males with a M:F ratio of 1: 2.33. The most common indication for cholecystectomy was cholelithiasis (81.66%) followed by cholecystitis (11.66%) and neoplastic diseases of gall bladder (5%). The average time for duration of surgery was found to be less in group A (P<0.05). Duration of analgesia was found to be comparable in both the groups (P>0.05). Postoperative respiratory problems such as atelectasis and pneumonia were more common in group B as compared to group A (P<0.05). The difference in the mean pain score was statistically insignificant at all-time intervals of the study up to 24 h into the postoperative period (P > 0.05). The difference in the mean pain score was statistically insignificant at all-time intervals of the study up to 24 h into the postoperative period (P > 0.05). There was no statistically significant difference in mean number of analgesic doses in group A and group B (P=0.5081). Conclusion: Thoracic segmental spinal anaesthesia is a better alternative to general anaesthesia in patients undergoing upper abdominal surgeries such as cholecystectomy particularly in patients having respiratory morbidties. Segmental Spinal anaesthesia was found to be associated with comparatively less post-operative respiratory complications, early ambulation and reduced duration of hospital stay. Keywords: Segmental Spinal Anaesthesia, Cholecystectomy, Complications, Outcome.
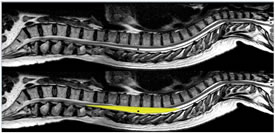
INTRODUCTION The name segmental spinal is often widely used synonymously with thoracic spinal anaesthesia. But in real sense segmental spinal anaesthesia means “Blocking of the required dermatomes essential for the proposed surgical procedure with very low effective local anesthetic drug dose.” This often necessitates dural puncture at high lumber or thoracic levels apart from the conventional spinal below L1. Lower the dose of local anesthetic drug used more likely it is to produce a true segmental block1. There are three main issues related to spinal at unconventional levels risk of neuronal injury, respiratory embarrassment due to extensive thoracic nerve blockade and cephalad spread of local anesthetic drugs causing high or total block2. Many studies performed using myelography showed that the thoracic cord lies anteriorly in theca while lumber spinal cord is situated more dorsally. The space between the dura mater and the mid to lower thoracic spinal cord on its width is actually greater than that of epidural space in lumber region because of lumber enlargement. So lumber spine is at greater risk of needle damage3. A possible anatomical explanation for the absence of spinal cord lesion during the accidental perforation of thoracic dura mater was proposed by Imbelloni and Gouveia through a study using MRI - which showed following measurements:- 5.2mm at T2, 7.75mm at T5 , and 5.88mm at T10 , a space sufficiently large to allow the entrance of a needle during accidental or intentional puncture of the dura4.
Figure 1: MRI Image of Spinal Cord- Note sufficiently large space at thoracic level
Extensive thoracic nerve blockade leads to paralysis of anterior abdominal wall muscles which may lead to some impediment in forceful expiration and coughing. However, use of low dose of drugs preserves the coughing ability by causing minimal motor weakness of expiratory muscles5. The main inspiratory muscle diaphragm is usually unaffected and expiration at rest is usually a passive process. Heart rate may decrease with high neuraxial block as a result of blockade of cardioaccelerator fibers arising from T1 to T4. But as the right atrial filling is maintained (due to lumbosacral sparing and less vasodilatation in lower limbs) that sustains the outflow from intrinsic chronotropic stretch receptors located in the right atrium and great veins6. Till date segmental spinals are being used only in high risk morbid patients for selective surgeries7. After the successful use of this technique in many intraabdominal surgeries and encouraged by its advantages (of great hemodynamic stability, minimal motor block, faster sensory recovery and early bladder control) and no added risks with careful performance, it looks very likely that it will establish itself as a routine procedure in day care anaesthesia. Patients chosen for this technique need to be evaluated carefully and the technique is to be reserved for experienced clinicians with a good learning curve8. Practically all the abdominal surgeries (upper/lower, major /minor, daycare/or not, laparoscopic/open) are possible with segmental spinal alone or CSE (combined spinal epidural). If that’s not all then the option of CSSA (continuous segmental spinal anaesthesia) is also available. Depending on the type of surgery, patient’s hemodynamic status and associated co-morbid conditions the dose of local anesthetic agent and the site of injection along the neuraxis can be varied. For all abdominal surgeries with an adequate dose, thoracic spinal above T10 is hardly required. Space between T10 and L1 is usually sufficient for all abdominal procedures. On an average a dose of 7.5 to 10 mg (1.5 to 2ml) of bupivacaine/levobupivacaine with some additive (fentanyl/clonidine) works well for 90 to 120 mins. This dose is exactly half the amount required when conventional spinal at lumber level to achieve a level of T3-T4 is used9. Amongst the available drugs isobaric drugs like 0.5% bupivacaine /levobupivacaine, 0.75% ropivacaine or chlorprocaine 1% can be used for segmental spinals. Hyperbaric bupivacaine can also be a part when gravity dependence is desired. Ropivacaine 0.75% and bupivacaine 0.5% are comparable. But for intrathecal use ropivacaine is nearly half as potent as bupivacaine because of lower lipid solubility. Ropivacaine has stronger differentiation between sensory and motor blocks. Levobupivacaine isobaric 0.5% - lower toxicity profile than racemic one. Being isobaric less sensitive to position issues. Low dose technique blocks sensory nerves in preference to motor ones (sometimes labelled as “selective”). This tends to preserve the muscle tone and power in the legs. Slightly less relaxation does not seem to be an obstacle to successful surgery. Addition of small doses of fentanyl or clonidine causes increased intensity of sensory blockade. Other advantages are - onset is gradual, hemodynamic stability even with high levels of block, motor block time is shorter leading to early ambulation, early bladder control. Onset time for isobaric drugs at thoracic level is not much as compared to lumber levels10. We conducted this study to compare segmental and general anesthesia in patients undergoing laparoscopic cholecystectomy.
MATERIALS AND METHODS This was a prospective comparative study conducted in the Department of Anesthesiology in a tertiary care medical college situated in an urban area. In this study 60 patients belonging to ASA I and II and undergoing laparoscopic cholecystectomy were included on the basis of a predefined inclusion and exclusion criteria. Institutional ethical committee duly approved the study and written informed consent was obtained from the patients. Out of 60 cases 30 cases received segmental Spinal anaesthesia (SA) with Isobaric Levobupivacaine 0.5% (Group A) and remaining 30 patients were operated under general anaesthesia using Midazolam, fentanyl, propofol, isoflurane and vecuronium (Group B). A detailed history was taken in all the cases and patients who have been included in group A were also informed about the possibility of conversion to general anesthesia if need arises. Moreover, patients in group A were also given information about the possible side effects of segmental anesthesia such as shoulder pain and vomiting. Pre-anesthetic management of patients in both the groups was similar. All patients received Iv fentanyl, ranitidine and ondansetron. Heart rate, respiratory rate, mean arterial pressure and SPo2 were recorded in all the patients. In Group A the patients were placed in left lateral decubitus position and subarachnoid space puncture was done between T9 and T10 and 2ml Isobaric Levobupivacaine 0.5% with 25 mcg fentanyl was injected. After injection patients were placed in supine position. Anesthetic effect was confirmed by pin prick (sensory). During surgery IV midazolam and IV fentanyl were given if needed. In group B anesthesia was induced with 2.0 mg/kg of propofol and 0.1 mg/kg vecuronium. Patients were maintained on controlled ventilation with oxygen, nitrous oxide and isoflurane. At the end of surgery patients were reversed with neostigmine and glycopyrrolate. All patients underwent laparoscopic cholecystectomy. Following surgery patients were shifted to ward. IV fluid were given for 6 hours. IV diclofenac 75 mg was given for post-operative pain relief. Inj fentanyl 1mcg/kg was repeated if pain was not controlled by diclofenac injections. Postoperative pain was recorded at 6,12 and 24 hours after surgery using Visual analogue Score. Any adverse effect such as nausea, vomiting, retention of urine, headache, shoulder pain and neurological involvement was noted and compared in both the groups. Patients were discharged 48 hours after surgery unless there was a reason for not doing so. Mean anesthesia time, duration of surgery, postoperative pain and complication in both the groups were compared. Inclusion Criteria
Exclusion Criteria
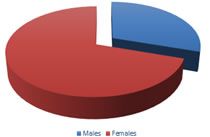
RESULTS This was a prospective comparative study in which 60 patients belonging to ASA I and II and undergoing laparoscopic cholecystectomy were included on the basis of a predefined inclusion and exclusion criteria. Out of 60 patients included in this study there were 42 (70%) were females and 18 (30%) were males with a M:F ratio of 1:2.33. Figure 2: Gender Distribution of the studied cases The patients were divided into 2 groups of 30 patients each on the basis of anesthesia given. First demographic details of the patients in both the groups were studied. The analysis of the mean age of the cases showed that the mean age of patients in Group A and Group B was 46.24 ± 7.22 and 48.12 ± 6.34 respectively. The mean age was found to be comparable in both the groups (P=0.146) with no statistically significant difference. Similarly, parameters such as height, weight, body mass index, and ASA grades were found to be comparable in both the groups with no statistically significant difference in between 2 groups (P>0.05).
Table 1: Distribution Of Patient Characteristics Among The Two Groups
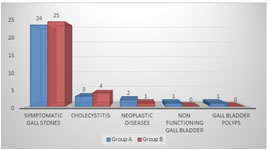
The analysis of indication of surgery showed that the most common cause of cholecystectomy in both the groups was found to be cholelithiasis (81.66%) followed by cholecystitis (11.66%) and neoplastic diseases (5%). Figure 3: Indications for cholecystectomy in studied cases The analysis of the patients on the basis of duration for surgery showed that the mean surgery time in group A was 36.12 ± 10.08 whereas in group B the mean time for surgery was 38.34 ± 9.28. The duration of surgery was found to be less in group A as compared to group B and the difference was found to be statistically insignificant (P = 0.3785). Table 2: Duration of surgery in studied cases
The analysis of the cases on the basis of presence of co-morbid conditions showed that in group A the common co-morbid conditions were hypertension (30%), diabetes mellitus (23.33%) and COPD (10%). In group B hypertension, diabetes and COPD was present in 8 (26.67%), 4 (13.33%) and 2 (6.66%) patients respectively.
Figure 4: Co-Morbidities in studied cases Duration of analgesia in both the groups before the need for the first rescue analgesic was comparable in both the groups using t test, the values were found to be statistically insignificant (P = 0.0923).
Table 3: Comparison Of Duration Of Analgesia In Both The Groups
The analysis of adverse effects of the patients during peri-operative or post-operative period showed that in group A shoulder pain was experienced by 2 (6.66 %) patients while in group B there was no patient who experienced shoulder pain. 1 (3.33 %) and 2 (6.66%) Patients undergoing laparoscopic cholecystectomy under segmental spinal were found to have episodes of hypotension and bradycardia whereas in general anesthesia group hypotension and bradycardia was noted in 2 (6.66%) and 1 (3.33%) patients respectively. Respiratory problems such as postoperative pneumonia or atelectasis was more common in general anaesthesia (26.66%) as compared to segmental spinal group (3.33%). Nausea and vomiting were present in 2 (6.66%) patients in group A. Table 4: Adverse Effects In Both The Groups
Analysis of the distribution of mean pain score between Group A and Group B showed that the difference in the mean pain score was statistically insignificant at all-time intervals of the study up to 24 h into the postoperative period (P > 0.05). Table 5: Mean Pain Scores in The Studied Cases Up to 24 hours Postoperatively
The analysis of diclofenac and fentanyl requirement within first 24 hours after surgery showed that the mean number of tramadol diclofenac and/or fentanyl in 24 hours in group A was 2.12 ± 0.48 whereas in group B this requirement was 1.98 ± 0.45. There was no statistically significant difference in mean number of analgesic doses in group A and group B (P=0.5081) Table 6: Comparison Of Mean Number Of Analgesic Doses In 24hours Between The Groups
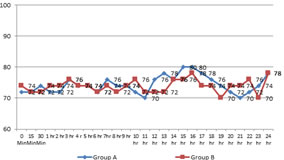
The Mean MAP in Group A was 74.37 ± 5.88 whereas in group B MAP was found to be 73.85 ± 6.14. The analysis of mean arterial pressures (MAP) of patients up to 24 hours postoperatively were found to be comparable (P=0.1713). Figure 5: Mean Arterial Pressures in studied cases up to 24 hours post-operatively The analysis of heart rates showed that the mean heart rate in Group A was 79.48 ± 6.40 whereas in group B mean heart rate was found to be 78.85 ± 3.78. The analysis of mean heart rate of patients up to 24 hours postoperatively showed that there was no statistically significant difference in mean heart rate of patients in both the groups (P=0.06).
Figure 6: Mean Heart Rates in studied cases up to 24 hours post-operatively. The patients in group A had a shorter mean hospital stay of 2.535 ± 0.56 days as compared to patients in group B who had a mean hospital stay of 4.592 ± 0.733 days. The difference in mean duration of hospital was found to be statistically highly significant. The increased mean hospital stay in group B was mainly due to postoperative respiratory complications.
Table 7: Mean Hospital stay in studied cases
DISCUSSION Since the introduction of spinal anaesthesia in 1898 by Bier, it is traditional in most cases to puncture the subarachnoid space (SAS) at level well below the termination of spinal cord to avoid the neural damage11. But in 1909, Thomas Jonessco proposed the use of general spinal block for the surgeries of head, neck and thorax, puncturing the SAS between 1st and 2nd thoracic vertebra and succeeded to produce profound analgesia for the head, neck and upper limbs12. He also punctured the SAS at mid thoracic and lower thoracic levels for thoracic and abdominal surgeries. In 2006 the new era of studies on segmental spinal anaesthesia puncturing SAS at T10 for laparoscopic cholecystectomy started when J Van Zundert used this technique to anaesthetize a patient with severe obstructive lung disease13. He used segmental spinal anesthesia in a patient who had chronic obstructive pulmonary disease with severe emphysema. The patient was a heavy smoker and was also found to have α-1-antitrypsine deficiency. The patient suffered from frequent respiratory infections, required continuous oxygen therapy and had severe functional impairment, even minimal activity. The surgeons could successfully perform cholecystectomy in this patient under segmental spinal anesthesia. The authors concluded that combined spinal/epidural anaesthesia technique, applied in the lower thoracic region and with a minute dose of local anesthetic, can be used to provide a segmental subarachnoid block sufficient to allow laparoscopic cholecystectomy to be performed, even in a patient with severely abnormal respiratory function. Since this case report there have been many studies about segmental spinal exploring its utility in many different surgical procedures like awake thoracoscopic and thoracic surgeries14, laparoscopic cholecystectomy and breast surgeries etc15. Elakany MH et al. conducted a study to compare thoracic spinal anesthesia with general anesthesia in breast cancer surgeries. Forty patients were enrolled in this comparative study with inclusion criteria of ASA physical status I-III, primary breast cancer without known extension beyond the breast and axillary nodes, scheduled for unilateral mastectomy with axillary dissection. They were randomly divided into two groups. The thoracic spinal group (S) (n = 20) underwent segmental thoracic spinal anesthesia with bupivacaine and fentanyl at T5-T6 interspace, while the other group (n = 20) underwent general anesthesia (G). Intraoperative hemodynamic parameters, intraoperative complications, postoperative discharge time from post-anesthesia care unit (PACU), postoperative pain and analgesic consumption, postoperative adverse effects, and patient satisfaction with the anesthetic techniques were recorded. The authors found that Intraoperative hypertension (20%) was more frequent in group (G), while hypotension and bradycardia (15%) were more frequent in the segmental thoracic spinal (S) group. Postoperative nausea (30%) and vomiting (40%) during PACU stay were more frequent in the (G) group. Postoperative discharge time from PACU was shorter in the (S) group (124 ± 38 min) than in the (G) group (212 ± 46 min). The quality of postoperative analgesia and analgesic consumption was better in the (S) group. Patient satisfaction was similar in both groups. On the basis of these findings the authors concluded that Segmental thoracic spinal anesthesia has advantages when compared with general anesthesia and can be considered as a sole anesthetic in breast cancer surgeries16. Similar observations were reported by Belzarena SD et al.17 and Leao DG et al.18. Yousef GT et al. conducted a study to compare spinal anesthesia, (segmental thoracic or conventional lumbar) vs the gold standard general anesthesia as three anesthetic techniques for healthy patients scheduled for elective laparoscopic cholecystectomy, A total of 90 patients undergoing elective laparoscopic cholecystectomy were randomized into three equal groups to undergo laparoscopic cholecystectomy with low-pressure CO2 pneumoperitoneum under segmental thoracic (TSA group) or conventional lumbar (LSA group) spinal anesthesia or general anesthesia (GA group). To achieve a T3 sensory level authors used (hyperbaric bupivacaine 15 mg, and fentanyl 25 mg at L2/L3) for LSA group, and (hyperbaric bupivacaine 7.5 mg, and fentanyl 25 mg at T10/T11) for TSA group. Propofol, fentanyl, atracurium, sevoflurane, and tracheal intubation were used for GA group. Intraoperative parameters, postoperative recovery and analgesia, complications as well as patient and surgeon satisfaction were compared between the three groups. The authors concluded that Segmental TSA provides better hemodynamic stability, lesser vasopressor use and early ambulation and discharge with higher degree of patient satisfaction making it excellent for day case surgery compared with conventional lumbar spinal anesthesia19. Similar better hemodynamics during surgery in patients undergoing segmental spinal anesthesia were reported by Imbelloni LE et al.
CONCLUSION In patients undergoing laparoscopic cholecystectomy segmental spinal anesthesia can be a better choice as compared to general anesthesia particularly in those patients who have co-existent respiratory co-morbidities such as chronic obstructive airway disease. Segmental spinal anesthesia is associated with decreased incidence of postoperative pneumonia and atelectasis. Moreover, segmental spinal anesthesia was found to be associated with reduced duration of hospital stay
REFERENCES
Policy for Articles with Open Access
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home