|
Table of Content - Volume 14 Issue 3 - June 2020
Comparison between I-gel and endotracheal tube for hemodynamic stability and perioperative complications in hypertensive patients undergoing elective surgery under general anaesthesia
V Oza1, J Mehta2*, V Parmar3, B Sharma4
1Assistant Professor,3Professor&HOD, 42nd Year Resident, Department of Anaesthesiology, P.D.U. Medical College and Hospital, Rajkot, INDIA. 2Assistant Professor, Department of Anaesthesiology, SBKS Medical institute and Research centre, Waghodiya, Vadodara, INDIA. Email: jbmehta.28@gmail.com
Abstract Background: I-gel is a second generation supraglottic device that has soft non inflatable cuff. Our study was designed to compare hemodynamic stability and perioperative complication between I-gel and endotracheal tube in hypertensive patients undergoing elective surgery under general anaesthesia. Aims and objective: Study was done to compare hemodynamic stability and perioperative complications between I-gel and endotracheal tube in hypertensive patients undergoing elective surgery under general anaesthesia. Methods: sixty patients aged between 40 to 60 of either gender and American society of Anaesthesiology (ASA) grade II were randomly assigned into either group. In Group A, patients airway was secured with I gel and in group B, patients airway was secured with Endotracheal tube. Hemodynamic parameters like pulse rate; Systolic, diastolic and mean blood pressure; oxygen saturation were recorded before induction just after induction, 3 minute, 5 minutes, 10 minutes and 15 minutes after induction. Complications like hypoxia, coughing, laryngospasm, leak, blood on device, sore-throat, gastric insufflations, hiccups, regurgitation, injury to lip, gum or teeth, dysphagia, dysphonia if occurs were noted. Result: There was increases in heart rate from 80.57 per minute before induction to 87.47 after induction, 85.21,85.3,83.53, at 3, 5 and 10 min respectively in group A and from 79.5 per minute before induction to 90.4 after induction , 87.27, 87.23 and 83.87 at 3,5 10 min respectively in group B. SBP, DBP and MBP also increased after induction. In Group A MBP was 92.95 mmHg before induction to 96.73 after induction, 94.84, 93.95, 94.44, and 93.46 at 3,5,10 and 15 min respectively. In Group B MBP was 93.28 mmHg before induction, 101.44 just after induction, 98.97, 96.33, 99.29 and 98.53 at 3,5,10 and 15 min respectively. Conclusion: Data suggest that I-gel provides stable hemodynamic condition and lesser complications than endotracheal tube in hypertensive patients. Key Words: Endotracheal tube, General anaesthesia, Hypertension, I-gel.
INTRODUCTION Laryngoscopy and endotracheal intubation is a gold standard to secure patient’s airway for general anaesthesia. But this technique is known to induce hemodynamic changes. The stress response to laryngoscope is well known to be centrally mediated sympathetic reflex1, presumed that stretching of the laryngeal and pharyngeal tissue during laryngoscopy was the major cause of the hemodynamic response. Laryngoscopy produces marked short-term stress responses2 with determined effect on the coronary and cerebral circulations in high-risk patients, particularly in those with systemic hypertension3. Laryngoscopy lead to short term rise in pulse rate and blood pressure, which can be tolerated by healthy patient but it has deleterious effect on patients having hypertension, coronary insufficiency and cerebro-vascular disease. I-gel (Intersurgical Ltd, Wokingham, UK) is a second generation supraglottic airway device (SAD) made of thermoplastic elastomer which is soft, gel-like, and transparent. Cadaver studies have shown that i-gels effectively conformed to the perilaryngeal anatomy and achieved proper positioning for supraglottic ventilation4. Studies performed on manikins and patients have shown that the insertion of the i-gel was significantly easier when compared with insertion of other SADs5,6. Insertion of I-gel does not require laryngoscopy so not associated with stress response as seen with laryngoscopy. So, we compared I-gel with endotracheal intubation for hemodynamic stability and perioperative complications in hypertensive patient undergoing elective surgery under general anaesthesia. We compared changes in heart rate (HR), systolic blood pressure (SBP), diastolic blood pressure (DBP) and mean blood pressure (MBP) at various time point to determine hemodynamic stability.
MATERIAL AND METHODS Our study was randomized comparative study conducted in hypertensive patient undergoing elective surgery under general anaesthesia in P.D.U Medical college and hospital, Rajkot. The study duration was 12 months. The study population was randomly divided in two groups (30 patients in each group) by computer generated random number table in group A and B. Group A: In this group airway was secured by appropriate size I-gel insertion. Group B: In this group airway was secured by laryngoscopy and endotracheal intubation with appropriate size endotracheal tube. Inclusion criteria:
Exclusion criteria:
Once patient met all the inclusion criteria, thorough preoperative anaesthesia check-up was done. Blood pressure was measured in supine position 3 times, 15 minutes apart. Patients having SBP < 140 mmHg and DBP < 90 mmHg were included in study. After that written informed consent for study was taken. All the patients were advised to take antihypertensive medication as per schedule and kept nil by mouth for 6 hours before operation. On the day of surgery again blood pressure was taken and if blood pressure < 140/90 mmHg then taken inside operation theatre (OT). After taking patient inside OT, 20 gauge intravenous cannula was taken. Standard monitors were attached including electrocardiogram (ECG) leads, noninvasive blood pressure (NIBP) cuff, oxygen saturation (SpO2) probe. Baseline parameters including pulse rate (PR), SBP, DBP, mean blood pressure (MBP), SpO2 were recorded. All the patients were premedicated with inj. Glycopyrrolate 0.004 mg/kg, inj. Ondansetrone 0.08mg/kg, inj. Midazolam 0.05mg/kg, inj. Tramadol 1mg/kg. Preoxygenation was done for 3 minutes and induction was done with Inj. Propofol 2 mg/kg. After confirming loss of eye reflex inj. Succinylscholine 2 mg/kg was given. After waiting for disappearance of fasciculation, in group A patients airway was secured by inserting appropriate size I-gel while in group B by laryngoscopy and appropriate size endotracheal tube (ETT) insertion. Anaesthesia was maintained with 50% oxygen with 50% nitrous oxide, isoflurane and non depolarizing muscle relaxant. HR, SBP, DBP and MBP were recorded preoperatively, before induction, just after induction, then 3 min, 5 min, 10 min and 15 min after induction. Complications like hypoxia, coughing, laryngospasm, leak, gastric insufflations, hiccups, regurgitation, aspiration, injury to lip gums or teeth, blood on device, sore throat, dysphagia, dysphonia etc were recorded. All the data were expressed as mean + standard deviation(SD). Statistical analysis were performed by students t-test and chi-square test. P value <0.05 was considered statistically significant, a P value of <0.01 as statistically highly significant and a P value of <0.001 as statistically very highly significant.
RESULT Mean age in Group A was 49.93 year and in Group B was 50.07 year. Mean weight in Group A was 52.5 kg and in Group B was 53.5 kg. in group A 60% were male and 40% were female while in group B 53.33% were male and 46.66% were female. Mean duration of surgery was 1.48 hour in Group A and 1.67 hour in Group B ( Table 1) Table 1: Demographic data
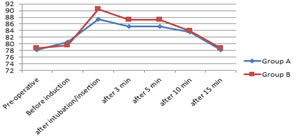
Mean heart rate increased after induction in both the group and remained elevated for at 3 min and 5 min after induction. Increase in HR was more in group B compared to group A ( table 2, figure 1)
Table 2: Changes in heart rate
Figure 1: Changes in heart rate Mean SBP, DBP and MBP increased immediately after induction and remained elevated for 15 minutes after induction in both group. But increase in blood pressure was more in group B compared to group A. ( Table 3) Figure 2: Changes in SBP,DBP and MBP Only 3 out of 30 patients in group A had blood on device at the time of I-gel removal and 5 out of 30 patients in group B had sore-throat in postoperative period. Two patient in group B has injury to lip. None of the patient in either group developed hypoxia, coughing, laryngospasm, leak, gastric insufflations, hiccups, regurgitation, dysphagia, dysphonia, etc.(Table 3)
Table 3: Perioperative complications
DISCUSSION There are several well-established advantages of using an SAD compared with a tracheal tube. The major ones include lower incidence of sore throat7, less haemodynamic upset during induction and maintenance of anaesthesia8,9,better oxygenation during emergence10 and an increased case turnover.11 Therefore, recently there has been a trend towards substituting an SAD for a tracheal tube for controlled ventilation in patients with a minimal risk of aspiration. The I-gel is a relatively new SAD made of gel-like material and does not have an inflatable cuff. It is designed to reduce airway morbidity even further. In our study we compared I-gel with endotracheal tube in hypertensive patients undergoing elective surgery under general anaesthesia. There was rise in HR, SBP, DBP and MBP in both the group but it was significantly higher in patients with endotracheal intubation compared to I-gel. Similar to our study Shrey Sharma, Beula Govindan12 done study on “A comparative study of haemodynamic response with laryngoscopic endotracheal intubation and laryngeal mask airway insertion in hypertensive patients at tertiary care hospital.” They found that, there was very highly significant difference (p< 0.000) in mean increase in heart rate (38.23% in group ET versus 28.26% in group LMA). The increase in arterial pressure were also significant. The systolic BP increased 40.16% in group ET compared with 37.60% in group LMA (p< 0.000). The diastolic BP was also seen increasing by 22.73% and 14.23% in group ET and group LMA respectively. Ahmed Said Elgebaly and Ahmed Ali Eldabaa13 done study on “Is I-gel airway a better option to endotracheal tube airway for sevoflurane-fentanyl anesthesia during cardiac surgery?” They found that None of the patients in the I-gel group required additional doses of fentanyl during the I-gel insertion, compared with 74% of the patients during laryngoscopy and endotracheal insertion in the endotracheal tube (ETT) group, for an average total dose of 22.6 ± 0.6 μg/kg. The mean blood pressure and heart rate did not significantly differ from the baseline values at any point of measurement in either group. Furthermore, central venous pressure (CVP), Peak airway pressure (PAP) and pulmonary capillary wedge pressure (PCWP) measured during the procedure were significantly lower in I-gel group than ETT group. Extubation required more amount of time in ETT than I- gel group.
CONCLUSION Our study concluded that I-gel causes less increase in heart rate and blood pressure compared to laryngoscopy and tracheal intubation and provide better hymodynamic stability compared to endotracheal intubation. I-gel also has less perioperative complication compared to endotracheal intubation. So I-gel should be preferred for airway management in hypertensive patients requiring general anaesthesia.
REFERENCES
Policy for Articles with Open Access
|
|
 Home
Home