|
Table of Content - Volume 14 Issue 3 - June 2020
A study of effectiveness of thermal radiofrequency nerve ablation of genicular nerves for the management of chronic osteoarthritis of knee joint
Tsering Yougyal1*, Jasa Ram Thakur2, Vijay Kumar Sauhta3, Girish Sharma4, Shweta Mahajan5
1,2Department of Health & Family Welfare Himachal Pradesh Government, Operation Theatre Incharge Civil Hospital Joginder Nagar, Distt Mandi, Himachal Pradesh, INDIA. 3Operation Theatre Incharge Civil Hospital Theog Shimla Himachal Pradesh, INDIA. 4Professor, Department of Anaesthesia, Dr Y. S. Parmar Government Medical College, Nahan, District Sirmour, Himachal Pradesh, INDIA. 5Associate Professor, Department of Anaesthesia, Indra Gandhi Medical college, Shimla. Himachal Pradesh, INDIA. Email: yougyal1001@gmail.com. , jassathakur821@gmail.com , d.sauhta@gmail.com
Abstract Background: Knee osteoarthritis (OA) is one of the most common conditions and cause of disability in older adults. Genicular nerve block with radiofrequency (RF) has recently emerged as a novel alternative treatment for chronic knee pain. Aim and objective: To compare the pain relief in the radiofrequency group with the control group after 1st, 4th, 8th and 12th week in patients with chronic osteoarthritis of knee joint Methodology: The study was conducted in randomized double blinded controlled prospective manner on the patients diagnosed clinically with osteoarthritis of knee from the period July 2016 to Jan 2017. The target sample was 50 ASA I/II patients, divided into two groups of 25 each. Group I did not receive any thermal radiofrequency ablation and Group II received it. Outcome observed with VAS. Results and discussion: In the consecutive follow up at 4th,8th and 12th week, patients in group I complained of progressive rise in the pain of the affected knee joint with the return to the initial VAS score. The patients in the group II continuously showed lower VAS score with mean score of 1.96 ± 0.978, 2.36 ± 1.075 and 2.60 ± 1.041 at 4th,8th and 12th week respectively. (P<0.05) Key Word: thermal radiofrequency nerve.
INTRODUCTION Osteoarthritis knee joint is one of the most common cause of chronic pain and disability in the older people. Over 100 millions people worldwide suffer from osteoarthritis, which is one of the most common cause of disability in the world. 1 Patients with OA have pain that typically worsens with weight bearing and activity and improves with rest, as well as morning stiffness and gelling of the involved joint after periods of inactivity. On physical examination, they often have tenderness on palpation, bony enlargement, crepitus on motion, and/or limitation of joint motion. While OA knee joints is equally present in men and women, it appears to be more common among younger men (<45years) and in the older women (>45 years). 2 Although there is no known cure for OA, In 1995, the American College of Rheumatology (ACR) published recommendations for the medical management of OA of the hip and knee.3 The OA treatment Guidelines emphasizes that these recommendations are not fixed, rigid mandates, and recognizes that the final decision concerning the therapeutic regimen for an individual patient rests with the treating physician. 4 Medications used in the pharmacological approach primarily include analgesics, nonsteroidal anti-inflammatory drugs (NSAIDS), intraarticular glucocorticoids and chondroitin and glucosamine (orally). 5-8 Invasive Treatment Modalities like Surgical intervention is reserved for patients with knee OA who have failed conservative treatment approaches. More invasive therapies primarily include arthroscopic debridement and Total knee arthroplasty (TKA). Radiofrequency neurotomy of genicular nerves seems to be a safe, effective and minimally invasive therapeutic procedure for chronic knee OA patients. This randomised controlled double blinded study will target to examine the effectiveness of thermal radio frequency treatment of genicular nerves around knee joints in patients with chronic osteoarthritis of knee joints Aim and objective: To compare the pain relief in the radiofrequency group with the control group after 1st, 4th, 8th and 12th week in patients with chronic osteoarthritis of knee joint
MATERIAL AND METHODS Present study was a controlled prospective randomized double blinded study carried out in the pain clinic centre of Indra Gandhi medical college and hospital Shimla. Study population was the patients diagnosed clinically with osteoarthritis of knee from the period July 2016 to Jan 2017. Inclusion criteria: 1. Patients between Stage 1 and Stage 3 radiological changes, according to the Kellgren-Lawrence classification 9 2. Patients with Age from 40 to 70 years.3. Patients with Pain localised to knee joint with no referred pain. 4. Patients without visible gross structural deformity of the knee joint. 5. Patients within ASA Grade I and II. 6. Patients on conservative treatment such as physical therapy, analgesic drugs including NSAIDs or opioids, for at least six months Exclusion criteria: 1. Patients refusal for the intervention. 2. Patients at Stage 4 radiologically, according to the Kellgren Lawrence classification. 3. Patients with Age less than 40 and more than 70 years. 4. Patients with visible gross deformity of the knee joint. 5. Patients of ASA Grade III or more. 6. Existence of general contraindications against application of invasive intervention 7. Psychiatric disorders. Study was approved by ethical committee of the institute. A valid written consent was taken from the patients after explaining study to them. The target sample was of 50, and they were divided into two groups of 25 each and assigned to their group using random allocation software. All the patients had undergone routine pre-anaesthetic check up including general history and examination of the patients. Routine investigations i.e. Hb, FBS/RBS, blood urea and serum creatinine, serum electrolytes, ECG, bleeding time (BT), clotting time (CT), chest X ray were checked. All the patient’s vascular access was taken and isotonic solution of 0.9% normal saline started. Standard monitoring protocol was followed (3-lead ECG, non invasive BP monitoring, pulse oxymetry). The procedures were carried out under intravenous sedation using Injection Fentanyl (Verfen, Verve health care limited, India) at dose 1 microgram per kilogram body weight, and local anaesthesia. C-Arm guidance was used for the placement of the radiofrequency needle. After the area to be intervened is wiped with an iodine-based antiseptic solution and spirit, it was draped properly. The nerve targeted includes superior lateral genucular nerve, superior medial genicular nerve and the inferior medial genicular nerve. The procedure was carried out using Radio frequecy machine G4 Cosman (Cosman medical, Burlington, Massachusetts, USA) for sensory and motor stimulation prior to the procedure and also used for the radio frequency genicular nerve ablation. Under all aseptic precautions, radiofrequency cannula was placed extra-articularly around the knee joint under C-Arm guidance. After satisfactory placement, the stylet in the cannula was removed and RF probe (Cosman RFK, Cosman medical inc, USA) was placed through the cannula and motor (2 hz and 0.5 V) and sensory (50 Hz and 0.2 V) stimulaton was done. After localising the Genicular nerve, 1 ml of 1% lidocaine was injected at each needle site and waited for two minutes. GROUP I Control group. (n = 25) No thermal or Pulsed radiofrequency was given. GROUP II Radiofrequency group. (n = 25) after the above procedure, Radiofrequency was given with target temperature at 70 degree Celsius for three cycles each of 1.5 minutes duration. Following the procedure, patients were transferred to the recovery room and observed for one hour for any possible side effects or complications and was discharged after one hour. Post procedure observation and follow up were made by independent anaesthetist not associated with the block giving team. During the 1st, 4th, 8th and 12th week, they were asked to attend the pain clinic date on the specified days (Wednesday/Saturday) or were contacted on phone and inquired about the Level of relief of pain according to Visual Analogue Scale (VAS) {0 for no pain at all and 10 for worst pain imaginable}. Data was analysed with appropriate statistical tests.
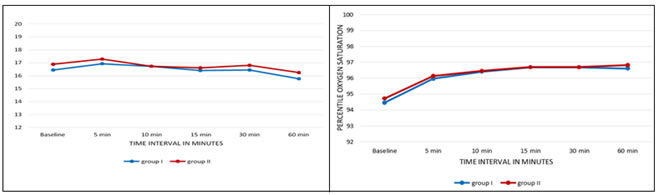
RESULTS Mean age (in years) in Group I was 63.68±6.479, and in Group II was 61.40±5.752 (p-value = 0.194). Mean age in both the groups was comparable. (p-value >0.05) Out of the total patients, 62% (31/50) were females and 38% were males (19/50). Mean weight (in kg) in Group I was 60.00±6.331, in Group II was 62.20±8.251 (p-value = 0.296). Mean weight in both the groups was comparable. Baseline HR in Groups I and II was 83.56±5.760 and 83.32±5.956 beats per minute respectively, showing no significant intergroup difference statistically (p-value=0.885). There was no statistically significant difference in heart rate between the groups during the period of procedure and while in the recovery room with total duration of 60 minutes (p-value >0.05). (table 1) Baseline MAP in Groups I and II was 98.76±8.084 and 97.92±9.151 mm of Hg respectively, showing no significant intergroup difference statistically (p-value=0.732). There was no statistically significant difference in MAP between the groups during the period of procedure and while in the recovery room upto total duration of 60 minutes (p-value >0.05). (table 2) Baseline respiratory rate (RR) in Groups I and II was 16.44±1.158 and 16.88±1.236 per minute respectively, showing no significant intergroup difference statistically (p-value=0.200). There was no statistically significant difference in respiratory rate between the groups during the period of procedure and while in the recovery room upto total duration of 60 minutes (p-value >0.05). (fig 1) Baseline percentile oxygen saturation (SpO2) in Groups I and II was 94.44±2.162 and 94.72±2.264 respectively, showing no significant intergroup difference statistically (p-value=0.657). There was no statistically significant difference in percentile oxygen saturation (SpO2) between the groups during the period of procedure and while in the recovery room upto total duration of 60 minutes (p-value >0.05). (fig 2) The VAS in group I at pre procedure time was 6.80±0.645 and group II was 7.00±0.707 and difference was found to be statistically insignificant (p-value=0.302). In group I, VAS in the immediate post procedure period was decreased to 0.80 ± 0.500 from 6.80 ± 0.645 (p value = 0.001), and was statistically significant. While in group II the VAS decreased to 0.92 ± 0.572 from the baseline VAS of 7.00 ± 0.707 (p value = 0.001), was statistically significant. When both the groups were compared for the VAS in immediate post-procedure period, the change was statistically insignificant (p value = 0.302). In the group I, the VAS at one week follow up was 6.56 ± 0.651, which was close to the baseline initial VAS of 6.80 ± 0.645 and difference was statistically insignificant (p = 0.056). In group II, the VAS at one week was 1.84 ± 0.987 from the baseline VAS of 7.00 ± 0.707 and difference was statistically highly significant (p value = 0.001). In the group I, the VAS at 4th week follow up was 6.88 ± 0.666 which was almost same as the baseline initial VAS of 6.80 ± 0.645 and was statistically insignificant (p >0.05), while in group II the VAS at 4th week was 1.96 ± 0.978, from the baseline VAS of 7.00 ± 0.707 was statistically highly significant (p value = 0.001). In the group I, the VAS at 8th week follow up was 6.92 ± 0.640 which was close to the baseline initial VAS of 6.80 ± 0.645 and was statistically insignificant (p >0.05), while in group II the VAS at 8th week was 2.36 ± 1.075, from the baseline VAS of 7.00 ± 0.707 was statistically highly significant (p value = 0.001). In the group I, the VAS at 12th week follow up was 6.92 ± 0.572 which was close to the baseline initial VAS of 6.80 ± 0.645 and was statistically insignificant (p >0.05), while in group II the VAS at 12th week was 2.60 ± 1.041, from the baseline VAS of 7.00 ± 0.707 was statistically highly significant (p value = 0.001). When both the groups (I and II) were compared for the VAS at 1st, 4th, 8th and 12th week follow up period, the VAS recorded were significantly lower in group II and the changes were statistically highly significant (p value = 0.001). (table 3)
Table 1: Comparison of mean heart rate between both groups
Table 2: Comparison of mean MAP between both groups
Figure 1: Comparison of mean respiratory rate between Figure 2: Comparison of mean Oxygen saturation between both group both group
Table 3: Comparison of mean Visual Analogue Scale (VAS) between both groups
DISCUSSION In our study, both the groups were comparable in the demographic variables like age, weight, ASA and sex. The baseline parameters like heart rate, mean arterial pressure and SpO2 were all comparable and statistically insignificant. During the period of procedure and one hour of observation in the recovery room, the parameters like heart rate, mean arterial pressure, respiratory rate and SpO2 were all comparable and statistically insignificant. The VAS recorded in both the groups prior to procedure was comparable. The VAS recorded in both the groups decreased immediately after the procedure and was comparable. This could be explained by administration of injection fentanyl 1 microgram per kilogram body weight and by injection of lidocaine at the needle sites after localization of nerves in both groups. When both the groups (I and II) were compared for the VAS at 1st, 4th, 8th and 12th week follow up period, the VAS recorded were significantly lower in group II and the changes were statistically highly significant (p value = 0.001). The results were comparable with studies by Mashahiko Ileuchi et al.. where the RF treated group had significantly decreased knee pain measured by the pain VAS for 2–3 months compared with the control group. RF group averaged lower than control group and there were significant differences between groups at 4 weeks (P = 0.028), 8 weeks (P = 0.007) and 12 weeks (P = 0.006) (94) in above study 10 Our study results were consistent with studies by Choi et al.., where the VAS knee pain scores were lower at all post-procedure assessment points compared with baseline (p < 0.001) in both the case and control group. By contrast, in the control group the VAS pain scores were only lower than baseline upto one week. When comparing knee pain improvement from baseline, the RF group showed superior improvement compared with the control group at both 4th week (p < 0.001) and 12th week (p < 0.001). 11 Our study is further supported by the findings of the study conducted by Wen-Sheng Shen et al.., both cases and controls presented significant difference between visual analogue scale scores during treatment and those at the termination of 3-month follow-ups (both P < 0.05). All patients felt less pain after treatments, cases group (RF group) presenting better improvement (P < 0.05). After carefully interviewing and statistically analysing, they concluded that RF have better efficacy in relieving refractory pain for longer duration and promoting function recovery in patients with knee OA than regular treatment.12 There were resembling and comparable results with the study by Pakize KIRDEMİR et al.., where the mean VAS score before the procedures was 8.9 ± 0.8, while at 1st, 4th and 12th weeks after the procedure it was 4.73 ± 3.23 ( p value < 0.01 ), 3.89 ± 2.9 ( p value < 0.01 ) and 3.93 ± 2.95 ( p value < 0.01 ) respectively, which shows statistically significant improvement with patient’s pain and lifestyle. 13 There was comparable results with the studies done by Ferdinand Iannaccone et al.., where the follow up done on the knee joint osteoarthritis patients treated with thermal radiofrequency on 3rd and 6th month had significant relief in the knee joint pain. 14 CONCLUSION Radiofrequency thermal ablation of genicular nerves of knee joint is a effective, safe and minimally invasive method that can be applied to the patients with osteoarthritis- related chronic knee pain.
REFERENCES
Policy for Articles with Open Access
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home