|
Table of Content - Volume 15 Issue 3 - September 2020
Vinod A Yadav1, Abhimanyu S Tarkase2*, Shailendra D Chouhan3
1Junior Resident 3, 2Associate Professor, 3Professor, Department Of Anaesthesiology, SRTR Govt. Medical College Ambajogai, Beed, 431517 Maharashtra, INDIA. Email: dr.vinod_yadav@yahoo.co.in
Abstract Background: Supraclavicular brachial plexus block is one of the preferred techniques to provide perioperative anaesthesia and analgesia for upper limb surgical procedures. The present study was undertaken to compare the efficacy of dexmedetomidine and dexamethasone when used as an adjuvant to 0.25% bupivacaine in supraclavicular block. Method: Total 80 patients of age 20-50 years, ASA grade I and II, scheduled to undergo upper limb surgeries were included and randomly divided into two equal groups. Group 1 received 30 ml of 0.25% bupivacaine with dexmedetomidine 50 μg diluted in 1.5 ml normal saline to make total volume of 32 ml. Group 2 received 30 ml of 0.25% bupivacaine with 2 ml (8 mg) dexamethasone to make total volume of 32 ml solution. Parameters like onset and duration of sensory and motor blockade, duration of analgesia, pulse rate, blood pressure, SpO2 and side effects were noted and compared between two groups. Results: The onset of sensory (6.46 ± 0.63 minutes) and motor blockade (8.75± 0.91 minutes) was early in group 1 as compared to group 2 where onset of sensory (10.62±1.12 minutes) and motor blockade (13.33±1.28 minutes) was observed. Also, duration of sensory and motor blockade, duration of analgesia was prolonged in group 1. Patients from both the groups remained hemodynamically stable and no significant difference in SpO2 changes between two groups. Significant sedation was seen in group 1 patients, but it was not associated with fall in SpO2. In group 1, two patients developed bradycardia and two patients developed hypotension. Conclusion: Using dexmedetomidine as adjuvant to 0.25% bupivacaine prolongs the onset and duration of block and postoperative analgesia compared to dexamethasone with minimal side effects. Key Words: Supraclavicular block, Anaesthesia, Analgesia, Dexmedetomidine, Dexamethasone, Bupivacaine, Sensory blockade, Motor blockade.
INTRODUCTION Peripheral nerve block has taken patient care in anaesthesia to a whole new level. Among the various peripheral nerve blocks, brachial plexus block is one of the most commonly practiced blocks, as it offers almost complete anaesthesia and analgesia and an excellent operative field for surgeries of the upper extremities. Among the various approaches for brachial plexus block, supraclavicular approach gives the most effective block for all portion of upper extremity and is carried out at the level of trunks of brachial plexus. The plexus is blocked where it is most compact i.e. at the middle of brachial plexus, resulting in homogenous spread of anaesthetic throughout the plexus with a fast onset and complete block.1,2 The various local anaesthetics employed in supraclavicular block are quite effective; however there are many limitations like delayed onset of action, patchy or incomplete analgesia etc. The duration of analgesia is a major limiting factor. Bupivacaine used frequently for supraclavicular nerve block as it has long duration of action from 6 to 9 hours. Different methods have been used to extend the duration of analgesia like using higher volume of local anaesthetics3 but it may also increase the risk of local anaesthetic systemic toxicity4. Continuous catheter-based nerve blocks provide very good postoperative analgesia5 but their placement requires additional time, cost and skill6. Moreover, various drugs have been studied as adjuvants to local anaesthetics in supraclavicular block with an aim to improve the duration and quality of block. Dexmedetomidine is one of them; it is a potent a2 agonist with a1: a2 ratio of 1600:1, which is 8 times more potent than clonidine7. In addition, dexamethasone has a potent anti-inflammatory and antinociceptive action and numerous studies have shown its efficacy as an adjuvant in nerve blocks. Hence, the present study was carried out with an objective to compared addition of dexmedetomidine and dexamethasone to bupivacaine for supraclavicular brachial plexus block in upper limb orthopedic surgery.
MATERIALS AND METHODS After obtaining Institutional Ethical Committee approval and written informed consent from all the patients, this prospective, randomized double-blind comparative study was conducted in Department of Anaesthesia, at Tertiary Care Hospital during a period from December 2017 to October 2019. Total 80 patients of age between 20-50 years, ASA grade I and II undergoing elective upper limb surgeries were enrolled in the study. Patients with age <20 and > 50 years, patients refusal, patients with significant coagulopathy, peripheral neuropathy, allergy to local anaesthetics, local infection at the injection site, Geriatric patients and patients on any sedative or antipsychotics were excluded from the study. A day before the surgery complete history of patient including any known drug allergy, general and systemic examination and local examination of supraclavicular area were done. Pulse rate, blood pressure, respiratory rate and weight of the patient were noted. All relevant investigations included haematological (Hb%, TLC, DLC, BT, CT), fasting / random blood sugar, blood urea, serum creatinine, chest X ray, and ECG were done. The patients were randomly divided into two groups each of 40 patients by sealed envelope method. The medications were prepared by another person so that patient and person doing study did not know in which group a particular patient had been allotted. Group 1 (n=40) received 30 ( ml) of 0.25% bupivacaine with dexmedetomidine 50 μg diluted in 1.5 ml normal saline to make 32 cc solution. Group 2 (n=40) received 30 ml of 0.25% bupivacaine with 2 ml (8 mg) dexamethasone for supraclavicular brachial plexus block to make 32 cc solution. Intravenous access was obtained in the limb opposite to that undergoing surgery with 18 G IV cannula. Standard monitors like ECG monitoring, Pulse oximeter, Non-invasive blood pressure were connected and monitored in all the patients. The patient was placed in a supine position with the head turned away from the side to be blocked. The arm to be anaesthetized was kept adducted, and the hand was kept extended along the side towards the ipsilateral knee as far as possible. Painting and draping was done using all aseptic precaution. Using classical approach, the midpoint of the clavicle was identified and marked. The posterior border of the sternocleidomastoid was palpated when the patient was made to raise the head slightly. Palpating belly of the anterior scalene muscle moving towards interscalene groove with the fingers, a mark was made at approximately 1- 1.5 cm posterior to the midpoint of the clavicle. By palpating the subclavian artery at this site, landmark was confirmed. After appropriate preparation and injection to make a skin wheal, a 22-gauge 5cm short bevel insulated needle was inserted at the point of entry above the midpoint of clavicle in backward- inward-downward direction. A peripheral nerve stimulator was used to locate the brachial plexus. The needle was advanced until muscle contraction was noted. The location endpoint was distal motor response that is the movement of fingers and thumb with an output current of 0.5 mA. If contraction is still observed or palpated, following negative aspiration, 32 ml of solution containing Inj. bupivacaine 0.25% (30cc) with dexmedetomidine 50 μg (0.5cc) + normal saline (1.5 cc) or dexamethasone 8 mg (2cc) as mentioned above was injected. A 3 min massage was performed to facilitate an even drug distribution. Patients were monitored for haemodynamic variables such as heart rate, blood pressure and oxygen saturation every 5 mins for first 15 mins. Next every 10 mins for 30 mins and every 15 min till the completion of surgery and then every 30 mins for first 2 hours and thereafter every 1 hour postoperatively. Sensory and motor blockade was assessed for at least 12 hr postoperatively. Assessment of blood loss was done and fluid was administered as per the loss. Duration of surgery and quality of block was noted. Duration of analgesia was assessed using standard Visual analogue scale (VAS) and sedation was assessed with Ramsey sedation Score for any sedation. Rescue analgesics was given in the form of inj. Diclofenac (1.5 mg/kg) intramuscularly when VAS score is > 4 on patients request and the time of administration was noted. Intra-operative complications, if any, including vessel injury, haematoma, nausea and vomiting, dyspnea, fall in respiratory rate or oxygen saturation, any symptom/sign of LA toxicity, ECG changes, Horner's syndrome, sedation, etc were recorded, with their respective management. Statistical Analysis The comparison of mean between the two groups with respect to demographic variables, pulse rate, noninvasive blood pressure, SpO2, onset, degree, duration of sensory and motor blocks, Ramsey sedation scale and visual analogue score was analysed by using chi-square test, unpaired t-test which gives p value to be applied as- If p> 0.01 indicates that the data is non-significant, If p< 0.01, indicates data is significant at 1% level of significance (i.e. out of 100, in 99 cases there is a significant difference) and if p<0.001, it is highly significant.
OBSERVATIONS AND RESULTS A total of 80 patients were enrolled in the study and randomly divided into two groups each of 40 patients. There was no significant difference between the mean age (in years) and weight (kg) as well as sex distribution in group 1 (Dexmedetomidine) and group 2 (Dexamethasone), (p>0.01) as shown in table 1. Table 1: Demographic profile of the patients and duration of surgery
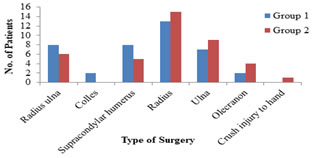
Number and type of surgeries were comparable and found no significant difference between two groups as depicted in Figure 1.
Figure 1: Type and distribution of various surgeries in group 1 and group 2
The onset of sensory and motor block was faster in group 1 as compared to group 2 and difference was statistically significant. Also, the duration of sensory and motor block was longer in group 1 as compared to group 2; there was significant difference among two groups. The quality of block was better in group 1 (3.87±0.33 min) as compared to group 2 (3.32±0.47 min). The duration of analgesia was longer in group 1 (987.22±62.48 min) as compared to group 2 (792.8±27.62 min) and difference between two groups was statistically significant as shown in table 2. Table 2: Supraclavicular brachial plexus block parameters (in Minutes)
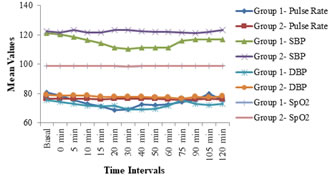
The preoperative baseline hemodynamic parameters in two groups were comparable. Although the hemodynamic parameters were significantly low in dexmedetomidine group, only 2 patients required medication. Patients from both the groups remained hemodynamically stable throughout the surgery. There was no significant difference in SpO2 changes between the two groups, (Figure 2). Figure 2: Intra-operative Hemodynamic parameters and SpO2
Baseline Ramsey sedation scale scores between the two groups were comparable. In group 1, patient started getting sedated at 5 mins intra-op and reached maximum sedation at 40 min (p<0.001). With decrease in sedation score thereafter, till it became equivalent to baseline score at 90 min. and sedation wore off. In comparison no sedation was seen in group 2, (Figure 3).
Figure 3: Comparison of Ramsey Sedation score between two groups
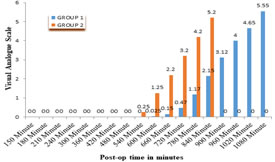
There was early onset of pain in group 2 than in group 1. Thus, group 2 requires early rescue analgesia in comparison with group 1. Figure 4 shows that group 1 had better control of pain as compared to group 2 post operatively.
Figure 4: Visual analogue scale between two groups
Only one patient in group 1 (Dexmedetomidine) was markedly sedated but no treatment was required. In group 1, 2 patients had bradycardia and were treated immediately with Inj. Glycopyrolate 0.2 mg iv stat and 2 patients had hypotension were treated immediately with Inj. Mephenteramine 6 mg iv stat. Rest no other complications were noted in either of the groups. Post-op no complications were noted in either of the groups. DISCUSSION Bupivacaine is most commonly used local anaesthetic in brachial plexus block as it has longer duration of action than other. So we have chosen bupivacaine as local anaesthetic in existing study. We selected dexmedetomidine as an adjuvant to local anaesthetics, because of its analgesic properties, stable haemodynamics and the decreased oxygen demand due to enhanced sympathoadrenal stability. A number of studies8-10 were done using 50 µg to100 µg doses with its attendant risk of side effects like sedation and bradycardia. In a few clinical studies, a lower dose of dexmedetomidine (30 µg) was used as adjuvant for brachial plexus block11. Considering the fact that Indian population has relatively lower body weight and that there are few studies with low dose, we decided to use low dose of dexmedetomidine (50 µg). Recently, dexamethasone has been studied as an adjuvant to local anaesthetic in peripheral nerve block 12, 13. In addition, dexamethasone was selected as an adjuvant to local anaesthetics in brachial plexus block because it has been reported to prolong duration of action of local anaesthetics and respiratory depression is not a major problem. The demographic profile (age, sex and weight) of the patients were comparable between two groups and found no statistically significant difference as similar to other studies13-17. The prolonged time for surgery alters postoperative recovery due to more bleeding, fluid and electrolyte imbalance. Hence we have studied surgeries lasting for 60-120 minutes and not involving too much volume shifts. The duration of surgery was comparable and found no significant difference between two groups. Both dexamethasone and dexmedetomidine shortens the onset of sensory and motor block when added to bupivacaine for supraclavicular brachial plexus block, but dexmedetomidine was more effective in shortening the time period for onset of sensory and motor block than that of dexamethasone and difference was statistically highly significant, this is comparable with the previous studies18-21. Several studies 22, 23 have shown that addition of dexamethasone and dexmedetomidine to local anaesthetics effectively and significantly prolongs the duration of sensory and motor block. In existing study, there was statistically highly significant difference among two groups in regards to duration of sensory and motor blocks. Both the drugs prolong the duration of sensory and motor block when added to bupivacaine, but dexmedetomidine was more effective in prolonging duration of sensory and motor block than dexamethasone. These findings correlated well with the earlier studies 17, 20, 22, 23. The sensory block tended to last longer as compared to motor block which agrees with the observation by de Jong et al.24. These authors explained that large fibres require high concentration of local anaesthetic than small fibres. The minimal effective concentration of local anaesthetic for large (motor) fibres is greater than that for small (sensory) fibres. Thus the motor function return before pain perception and duration of motor block is shorter than the sensory block. There was early onset of pain in group 2, so required early rescue analgesia in comparison with group 1. Maximum patients required rescue analgesia between (780-840 mins)(13-14 hrs) i.e. 10 patients at 780 mins and 38 patients at 840 mins in group 2 where as in group 1 rescue analgesia was required between (1020-1080 mins)(17-18 hrs) i.e. 26 patients at 1020 mins and all 40 patients at 1080 mins after giving block. This shows that group 1 had better control of pain as compared to group 2 post operatively. Many studies have shown that dexamethasone and dexmedetomidine when used as adjuvant to bupivacaine in regional blocks prolong the duration of analgesia. The current study found that dexmedetomidine prolongs the duration of analgesia more than dexamethasone. These findings are comparable with the previous studies [22, 25], The quality of block was better in dexmedetomidine group as compared to dexamethasone group with is in accordance with the study done by Memis et al.26 and Swami et al.27. The preoperative baseline hemodynamic parameters in two groups were comparable. There was significant difference in the two groups with dexmedetomidine showed a fall in pulse rate from 15 mins up to 105 mins and dexamethasone group having constant pulse. Though there was a significant difference between the two groups but only 2 patients required medication in group 1. This finding is in agreement with the study done by Agarwal et al.19 and Fritsch et al.28. The preoperative baseline blood pressures in two groups were comparable. Although the hemodynamic parameters were significantly low in dexmedetomidine group, only 2 patients required medication. Patients from both the groups remained hemodynamically stable throughout the surgery otherwise. In group 1 two patients developed bradycardia and two patients developed hypotension and required treatment. No such complications were seen in group 2. Group 1 patient’s sedation scores were statistically significant, but they were arousable and maintaining O2 saturation. Patients in group 2 were awake throughout intra and post-operative period. Similar observation was made in the study by Don Sebastian et al.29. Among the two groups only one patient in group 1 was significantly sedated, but it was not associated with fall in SpO2. During the study, 3 patients had patchy block and required general anaesthesia. So they were excluded from the study. CONCLUSION The present study signifies that dexmedetomidine shortens the onset of sensory and motor block, prolongs the duration of sensory and motor block and prolongs the duration of analgesia, provides better quality of block as compared to dexamethasone when used as an adjuvant to bupivacaine in supraclavicular brachial plexus block. Also, dexmedetomidine provides sedation in patients which is beneficial as additional sedation is not required. Dexamethasone does not cause sedation. Dexmedetomidine can cause bradycardia and hypotension though such incidences are very low. Dexamethasone is devoid of such complications. Other side effects like nausea, vomiting is not seen with either of the drugs used in current study.
REFERENCES
Policy for Articles with Open Access
|
|
 Home
Home