|
Table of Content - Volume 15 Issue 3 - September 2020
Comparison of analgesic efficiency between wound site infiltration of local anaesthetic agent and transversus abdominis plane block after total abdominal hysterectomy under spinal anaesthesia
Tejaswini Bagde1, Aparna Kulkarni2*, Shailendra Chauhan3, Abhimanyu Tarkase4
1Junior Resident, 2,4Associate Professor, 3Professor, Department of Anaesthesiology, SRTR Government Medical College, Ambajogai, Beed 431517, Maharashtra, INDIA. Email: tejaswinibagde21@gmail.com
Abstract Background: Postoperative pain management is of great importance in perioperative anesthetic care. The present study was undertaken to compare duration of post-op analgesia and time of requirement of 1st rescue analgesia between wound infiltration of local anaesthestic agent and transversus abdominis plane (TAP) block in patients undergoing total abdominal hysterectomy (TAH) under spinal anaesthesia. Method: A total of 100 patients were enrolled in the study and randomly divided into two equal groups. Group I received TAP block with 20 ml of 0.25% bupivacaine bilaterally by anaesthetists while those in group II received 20 ml of 0.25% bupivacaine as local wound infiltration by surgeon. 15 mins after the completion of surgery, sensory blockade was assessed every 30 mins till the patient complaint of pain. Results: Postoperatively from 0 minutes to 6 hours, VAS score was significantly higher in group II compared to group I (p<0.05). The mean duration of analgesia was significantly longer in group I (10.12±5.99 hours) as compared to group II (2.94±1.62 hours). Thus, significantly higher number of patients in group II required rescue analgesic and at higher dosages (p<0.05). The incidence of nausea and vomiting was more in group II (16; 32%) as compared to group I (11; 22%). Conclusion: TAP block is an effective and safe technique for postoperative analgesia for gynaecological surgeries than compared to the surgical wound infiltration. Key Words: Analgesia, Transversus Abdominis Plane, Hysterectomy, Anaesthesia, Bupivacaine, VAS score
INTRODUCTION The abdominal surgeries, may it be open or laparoscopic, are associated with significant post-operative pain. Control of postoperative pain is imperative for patient comfort, early mobilization, and faster recovery1. Safe and effective modalities of perioperative analgesia are essential for enhancing recovery after surgery. Good postoperative pain management has been shown to be effective in reducing perioperative morbidity associated with acute coronary events and thrombotic events in high-risk patients2. In addition to parenteral opioids and NSAIDS, various other methods used for post-operative analgesia are infiltration of local anesthetic agents, dermal patches, patient controlled analgesia and epidural catheters, etc3. However, opioids are the most commonly used analgesics in the perioperative period, which provide analgesia but have their own side effects. Therefore, use of a multimodal analgesic strategy is very important. Regional anesthesia and analgesia has shown to provide excellent analgesia and also provide benefits, which extend beyond the perioperative period4. Rafi originally described the transversus abdomen is plane (TAP) block. TAP catheter based techniques are relatively new techniques which have been used as a part of multimodal analgesia for abdominal surgery, cesarean section, abdominal hysterectomy, and prostatectomy. They are regional anesthesia techniques which provide analgesia to the skin and muscles of the anterior abdominal wall. Ultrasound for guiding the TAP block was first described by Hebbard et al.. The advantage over neuraxial techniques is absence of hemodynamic instability, early mobilization, and not requiring prolonged urinary catheterization. Despite a low-risk of complications and a high success rate, it is an underutilized technique 5, 6. The effectiveness of this procedure as a post-operative analgesic option for patients undergoing abdominal hysterectomies has been controversial as recent studies have found mixed results on its analgesic benefits in gynecological procedures. Local anaesthetic infiltration along the surgical wounds through subcutaneous planes also provides adequate analgesia without much of side effects. Both these techniques reduce the post-operative need of opioids and other side effects 7. Hence the present study was carried out at tertiary care centre to compare duration of post-op analgesia and time of requirement of 1st rescue analgesia between wound infiltration of local anaesthestic agent and TAP block in patients undergoing total abdominal hysterectomy under spinal anaesthesia.
MATERIALS AND METHODS A hospital based prospective, observational, randomized control study was conducted in100 patients of age 40-60 years, ASA grade I and II, who consented for the study and attending Tertiary Care Centre in the Department of Anaesthesia undergoing total abdominal hysterectomy during a period of 2 years. Patients with age <18 years and > 60 years, patient’s refusal, coagulopathy, history of relevant drug allergy and any contraindications to spinal anaesthesia were excluded from the study. The study was done after due permission from the Institutional Ethics Committee and Review Board and after taking written informed consent from the patients. A thorough history and physical examination was done as per proforma. A total of 100 consecutive subjects undergoing TAH were randomly divided into two groups using computer generated random numbers: Group I: 50 patients received TAP block and Group II: 50 patients received local wound infiltration. Intravenous line was secured on the accessible side of the limb undergoing surgery. Local anaesthesia and TAP block both were performed under standard monitoring after the abdominal hysterectomy done under spinal anaesthesia with pulse oximetry, non-invasive blood pressure measurement, heart rate, ECG, and pulse oximetry and EtCo2. Before initiation peripheral vascular access was obtained with 18G intravenous cannula in all patients. Pre-operatively 500ml ringer lactate solution was loaded. All patients were pre-medicated with inj. ranitidine 50mg iv and inj metoclopramide 10 mg iv. Patient in left lateral position, painting and draping was done under all aseptic precautions, using midline approach intrathecal space was accessed by traversing the L3-L4 interspace with 23G Quincke needle after confirmation of CSF fluid flow 3.2ml hyperbaric bupivacaine was injected intrathecally. Only patients with successful spinal anaesthesia were included in the study. The patients in group I received TAP block with 20 ml of 0.25% bupivacaine bilaterally by anaesthetists while those in group II received 20 ml of 0.25% bupivacaine as local wound infiltration by surgeon. 15 mins after the completion of surgery, sensory blockade was assessed every 30 mins till the patient complaint of pain. Statistical Analysis Quantitative data was presented with the help of Mean and Standard deviation. Comparison among the study groups was done with the help of unpaired t test as per results of normality test. Qualitative data was presented with the help of frequency and percentage table. Association among the study groups was assessed with the help of Anova and Chi-Square test. ‘P’ value less than 0.05 was taken as significant.
OBSERVATIONS AND RESULTS A total of 100 patients were enrolled in the study and were randomly divided into two equal groups. The majority of patients in group I were in the age group of 51-55 years (32%) while in group II majority of patients were in the age group of 40-45 years (34%). Table 1 show the age and weight distribution of patients and these found no statistically significant difference between two groups (p>0.05).
Table 1: Distribution of patients according to age and weight
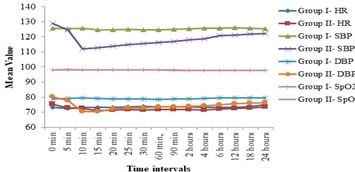
The time required for regression of spinal block till T12 in both groups was comparable (11.78 ± 2.52 mins vs. 11.16 ±1.33 mins) and statistically not significant (p>0.05). The heart rate was comparable in both the group (p>0.05). Intra-operatively from 10 minutes to 24 hours, systolic and diastolic blood pressure levels were significantly lower in group II compared to group I as per student t-test (p<0.05) while intra-operatively throughout the study, SpO2 levels were comparable between two groups (p>0.05) as shown in figure 1.
Figure 1: Comparison of hemodynamic parameters (HR, SBP and DBP) and SpO2 between two groups
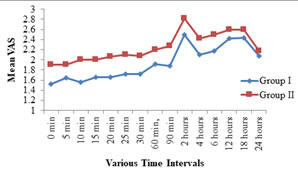
Postoperatively from 0 minutes to 6 hours, VAS score was significantly higher in group II compared to group I as per Student t-test (p<0.05) as depicted in figure 2. Figure 2: Comparison of VAS Score at various time intervals postoperatively
The mean duration of analgesia was significantly longer in group I as compared to group II (10.12±5.99 hours vs. 2.94±1.62 hours). This difference was statistically significant (p<0.05). Also, it was observed that significantly higher number of patients in group II required rescue analgesic and at higher dosages (p<0.05), (Table 2).
Table 2: Comparison of Duration of Analgesia and Requirement of Rescue Analgesic between two groups
The incidence of nausea and vomiting was more in group II (16; 32%) as compared to group I (11; 22%), however this difference was statistically not significant (p>0.05).
DISCUSSION The management of postoperative pain is an important issue. The uncontrolled postoperative pain is the major limiting factor for early ambulation and thereby puts patient to the increased risk of various complications as well. The desirable properties of an analgesic agent are that it provides safe and effective analgesia, with minimal side effects. The multimodal pain management is the answer of this. The TAP block is used for postoperative analgesia following abdominal surgeries. It provides blockade of the nociceptive inputs from the abdominal wall but not from the abdominal organs. Therefore, the block is used as a part of multimodal approach. However, TAP block is a type of abdominal field block that anaesthetizes the nerve supplying the abdominal wall and being used for providing post-operative pain relief after abdominal surgeries both in adults and children8. In the present study there was no statistically significant difference between two groups in regards to demographic profile (Age and weight distribution) of the patients (p>0.05), this is comparable with the study done by Mishra et al.9 and Prabhu et al.10. It was observed that the time required for regression of spinal block till T12 in both groups was comparable and statistically not significant difference between two groups. Also heart rate was comparable in both the group and it was statistically not significant as per Student t test (p>0.05). While intra-operatively from 10 minutes to 24 hours, systolic and diastolic blood pressure levels were significantly lower in group II compared to group I (p<0.05) whereas throughout the study, SpO2 levels were comparable between the groups (p>0.05). These findings are concordant to the studies of Prabhu et al.10 and Raghvendra et al.11. Postoperatively from 0 minutes to 6 hours, VAS score was significantly higher in group II compared to group I, (p<0.05) which is consistent with the previous studies 9-13. The mean duration of analgesia was significantly longer in group I as compared to group II and this difference was statistically significant as per Student t-test (p<0.05). This finding is in concordance to the studies of Prabhu et al.10, Raghvendra et al.11, and Selvaraju et al.14. Also, it was observed in present study that 15 (30%) patients in group I required 50 mg of rescue analgesic while 1 (2%) patient required 100 mg of rescue analgesic. 34 (68%) patients in group I did not require rescue analgesic 20 (40%) patients in group II required 50 mg of rescue analgesic while 22 (44%) and 3 (6%) patients required 100 mg and 200 mg of rescue analgesic respectively. 5 (10%) patients in group II did not require rescue analgesic. Thus, significantly higher number of patients in group II required rescue analgesic and at higher dosages (p<0.05). These results are consistent with the earlier studies 10, 12, 14-17. 11 (22%) and 16 (32%) patients in group I and group II respectively had nausea and vomiting. The difference between two groups was statistically not significant as per Chi Square test (p>0.05). Similar observations were noted in other studies9-11. The TAP block has been demonstrated to provide excellent analgesia to the skin and musculature of the anterior abdominal wall in patients undergoing colonic resection surgery involving a midline abdominal wall incision, patients undergoing cesarean delivery18 and patients undergoing radical prostatectomy 19.
CONCLUSION TAP block holds well as a part of multimodal analgesia regimen for patients undergoing total abdominal hysterectomy. These results suggest that TAP block may be an effective strategy in improving analgesic outcomes of patients undergoing abdominal hysterectomy without any complication. TAP block is an effective and safe technique for postoperative analgesia for gynaecological surgeries than compared to the surgical wound infiltration.
REFERENCES
Policy for Articles with Open Access
|
|
 Home
Home