|
Table of Content - Volume 16 Issue 1 - October 2020
Gautam Kumar Goel1, Gopal Krishan2*, Malti Agrawal3, Ram Pal Singh3, Sarfraj Ahmad4, Chandra Prakash Pandey5
{1Junior Resident, 2Associate Professor, 3Professor, 4Assistant Professor, Department of Anaesthesiology} {5Professor, Department of General Surgery} RMCH Bareilly, INDIA. Email: gkgsvm@yahoo.com
Abstract Background: Many anaesthetic techniques have been used for inguinal mesh hernioplasty. The use of regional anaesthesia techniques are the most satisfactory methods for high risk patients who are unfit for general or spinal anaesthesia. Aims and objectives: The aim of this study was to compare the effectiveness, safety, and complications of ultrasound guided ilioinguinal and iliohypogastric nerve block with subarachnoid block for inguinal mesh hernioplasty. Materials and Methods: This study was carried out on 60 patients of ASA Grade I or II undergoing mesh hernioplasty. Group A patients received ultrasound guided ilioinguinal and iliohypogastric nerve block with 25 ml of 0.5% isobaric levobupivacaine. Group B patients received subarachnoid block with 3 ml of 0.5% isobaric levobupivacaine. Onset and duration of sensory blockade was studied in both the groups. Motor power was assessed at 5 minutes and just postoperatively in both the groups.All patients were sedated using continuous propofol infusion. Results: Postoperative ambulation was significantly earlier in group A patients. Patients in Group A had better hemodynamic stability when compared with group B. Conclusion: Ultrasound guided ilioinguinal and iliohypogastric nerve block under sedation is a better alternative anaesthetic technique for inguinal mesh hernioplasty in high risk patients. Key Words: Ilioinguinal, Iliohypogastric, Levobupivacaine, Propofol, Ultrasound.
INTRODUCTION Many anaesthetic techniques have been used for inguinal mesh hernioplasty. The choice of the anaesthetic technique depends on its acceptability by the patient and surgeon, the feasibility and safety of the procedure, surgical method, medical history, co morbidities, and the cost. Epidemiological data have found that general anaesthesia (GA) is used in 60–70% of cases, central neuraxial block in 10–20%, and regional anesthesia techniques with sedation in 5–15% of the cases.1,2 The use of local anaesthesia (LA) techniques is the most convenient method for patients who are unfit for general or spinal anaesthesia due to cardiovascular disease, cerebrovascular disease, severe respiratory disease, severe liver impairment, or coagulopathies. Ultrasound guided Ilioinguinal and iliohypogastric nerve block may be used for inguinal hernia repair surgeries as well as postoperative analgesia.3,4 Direct sonographic visualization of the ilioinguinal and iliohypogastric nerves improve the quality of the block, increases success rate to 95%, and reduces the risk for complications, whereas the conventional technique of ilioinguinal and iliohypogastric nerve block is associated with a failure rate of 40%. The postoperative requirements for additional analgesics are significantly lower in the ultrasound guided nerve block technique compared with the conventional blind fascia click technique.5,6,7 The use of intravenous sedation increases the acceptability of local anaesthetic techniques. Moreover, it improves the success rate of the block. Propofol sedation provides rapid recovery due to rapid distribution and short elimination half-life. The brief duration of action ensures prompt responsiveness to change in its infusion rate and could easily be maintained at the desired level of sedation by varying the infusion rate. The use of propofol decreases the level of postoperative sedation, drowsiness, and confusion. 8,9,10,11
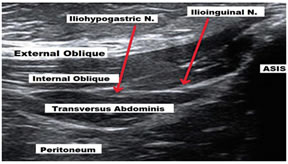
MATERIALS AND METHODS After approval from the institutional ethical committee, the present one year study was conducted in the department of anaesthesiology, Rohilkhand Medical College and Hospital, Bareilly starting from November 2018 to October 2019. The current study was carried out on 60 patients of American Society of anesthesiology class I or II. Patients with recurrent, bilateral, irreducible, or large scrotal hernias were excluded. The patients were randomly divided into two equal groups using the computer-generated random sequence of numbers. All patients were evaluated the evening before surgery and informed on whether they will be undergoing ultrasound guided ilioinguinal and iliohypogastric nerve block or subarachnoid block and how the procedure will be performed in either technique. All patients were trained to use visual analogue scale (VAS) to express their pain. All patients received a sedating dose of Midazolam (2–3 mg) before the procedure. Group A (n=30): All patients received ultrasound guided ilioinguinal and iliohypogastric nerve block with 25 ml of 0.5% isobaric levobupivacaine. Group B (n=30): All patients received subarachnoid block with 3 ml of 0.5% isobaric levobupivacaine. In group A, patients, under all aseptic precautions, a linear ultrasound probe with 10 Hz frequency at a depth of 3 cm from skin was placed at the anterior superior iliac spine in an oblique manner at the line joining the umbilicus and the anterior superior iliac spine. The nerves lie in the fascial split between the internal oblique and the transversus abdominis. After negative aspiration, 25 ml of 0.5% isobaric levobupivacaine was deposited between the transversus abdominis and the internal oblique. After local anaesthetic injection, the split widens because of spread of the drug. In group B, under all aseptic precautions, the patients were given subarachnoid block with 3 ml of 0.5% isobaric levobupivacaine, between the L3 and the L4 intervertibral space in sitting position with the help of 27 G quincke type spinal needle. The propofol infusion was started at the rate of 25 microgram /kilogram/minute in both the groups. Exclusion criteria - Patient refusal. Coagulopathy. Allergy to Local Anaesthetic or any included medications. Severe liver, renal, or cardiovascular diseases. Recurrent, bilateral, irreducible, incarcerated, or large scrotal hernias. Infection at the site of injection. Psychiatric disorder. Obesity (BMI >35). Lengthy operation duration of more than120 min. Neurological disease. Severe deformities of the spinal column, such as severe kyphoscoliosis, arthritis, and previous lumbar fusion surgeries. Sample size was estimated before study using duration of motor blockade as a primary outcome. A sample size of 60 patients was required at α =0.05, β =0.001 and power of study 95%. Statistical analysis of the data was done using the statistical package for the social sciences (SPSS 22.0) using independent t-test to determine mean significant difference between the two variables. p<0.05 considered as statistically significant and p < 0.001 considered as statistically highly significant. The data was compiled using Microsoft excel sheet (windows 2010). Measurements Age and weight of the patients and the surgery duration were measured. Onset and duration of sensory blockade was recorded. The total amount of intraoperative propofol consumed in each group was measured. Assessment of motor power was carried out 5 min after the block and immediately postoperatively using the modified Bromage Scale (Table 1). Ambulation time was also documented.
Table 1: Modified Bromage Scale
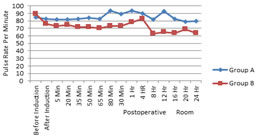
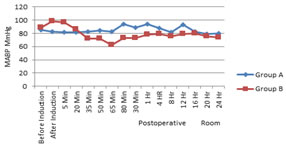
Heart rate and mean arterial blood pressure (MABP)were recorded before induction of anesthesia, after induction, 5 min and then every 15 min intraoperatively, and 30 min, 1 h, and every 4 h for the first 24 h postoperatively. Postoperative pain was assessed at 30 min, 1 h, and every 4 h postoperatively for 24 h using the Visual Analogue Scale (0–10), in which 0=no pain and 10=severe possible pain. The time of first need for rescue analgesia and the total rescue analgesia doses were recorded. Total propofol used intraoperatively was recorded. Postoperative sedation score was recorded using Ramsay sedation score (Table 2) immediately upon arrival into the post anaesthesia care unit and after 30 minutes. Patients’ and surgeon’s satisfaction was assessed.
Table 2: Ramsay Sedation Score
Anxious, agitated, or restless -1; Co-operative, oriented, and tranquil -2; Responding only to verbal commands- 3; Brisk response to loud auditory stimulus or light glabellar tap -4; Sluggish response to loud auditory stimulus or light glabellar tap-5; No response- 6
OBSERVATIONS AND RESULTS No significant difference was recorded as regards the demographic data and surgery duration (Table 3). The onset of sensory blockade was earlier in group B (SAB) 3.7±0.6 sec in comparison to Group A (IINB) 11.2±1.07 sec which was statistically significant (p=0.001). The duration of sensory blockade was significantly longer in group A (IINB) 307.8±8.25 Min. in comparison to Group B (SAB) 184.1±31.7 Min. which was statistically significant (p=0.001). Assessment of motor power at 5 Min and just postoperatively revealed that it was significantly different between the groups. The ambulation time was significantly shorter in group A (IINB) 317.8±62.5 in comparison to Group B (SAB) 411.6±78.7 sec. which was statistically significant (p=0.001). (Table 4). The Visual Analogue Scale when compared between the two groups revealed that significantly higher readings were found at the fourth and sixteenth hour measurements in group B (SAB). The time to first need for rescue analgesia was significantly longer in group A (IINB) and the total analgesia requirements were lesser (Table 5). The total dose of propofol used intraoperatively was significantly higher in group A (IINB) and the sedation score showed no statistical significance difference between the two groups in all measurements. As regards the vital signs, on comparing the two groups, the heart rate changes showed no significant difference between the two studied groups (Fig. 1), whereas the Mean Arterial Blood Pressure changes between the two studied groups revealed that it was significantly lower at 5, 15, 30, and 45 min after induction in group B (SAB) (Fig. 2). The patient satisfaction showed no significant difference between the two groups. Surgeon satisfaction was significantly higher in group B (SAB).
Table 3: Demographic Profile
Table 4: Comparison of onset and duration of sensory blockade, motor power and ambulation time (minutes)
Table 5: VAS and postoperative analgesia requirement
Image 1: Sonographic view of ilioinguinal and iliohypogastric nerve Figure 1 Figure 2 Figure 1: Comparison of mean pulse rate between Group A (IINB) and Group B (SAB); Figure 2: Comparison of mean arterial blood pressure between Group A (IINB) and Group B (SAB)
DISCUSSION In our study we demonstrated that Ultrasound guided ilioinguinal and iliohypogastric nerve block with sedation provides better anaesthetic technique in comparison to spinal or general anaesthesia for inguinal mesh hernioplasty in high risk patients. In the support of our study Bang et al., 12 Kurzor M et al., 13 Al alami et al.,14 Susuoka N et al.,15 Okur O et al.16 and Kamal K et al.17 also reported that various nerve block techniques are better alternates for inguinal herniorraphy as well as postoperative analgesia especially in high risk patients. Although in our study the onset of the sensory blockade is slower in group A, the use of the ultrasound guidance was proved to shorten the onset time of the sensory blockade. Koscielniak-Nielsen et al., [18] who reviewed the benefits of the ultrasound guided blocks, reported that the block onset was reduced in all ultrasound guided blocks while comparing ultrasound guided methods in six different peripheral nerve blocks with the nerve stimulator and the landmark-based methods. In our study the motor power was assessed using the modified bromage scale 5 min after the block and immediate postoperatively. The difference in motor power was statistically significant between the two groups. The illioinguinal and illiohypogastric nerve block does not affect the motor power, whereas the subarachnoid block produces intense sensory, motor and sympathetic blockade. Ghani et al..19 showed that the illioinguinal and illiohypogastric nerve block does not affect the motor power except if femoral nerve palsy accidently occurs, especially with blind infiltration. Transient femoral nerve palsy is a recognized complication after Ilioinguinal and iliohypogastric nerve block which causes knee weakness. The reported time of onset of transient femoral nerve palsy following surgery varies from 2–6 h. It usually resolves within 24–36 h. In the current study, the visual analogue scale in group B (SAB) was significantly higher at the 4th hour (p=0.002) and the 16th hour (p=0.002) postoperatively when compared with visual analogue scale in group A (IINB). In disagreement with the present study, Bang et al..12 reported that the visual analogue scale of patients receiving illioinguinal and illiohypogastric nerve block with monitored anesthesia care measured just after surgery was significantly higher than that of patients receiving subarachnoid block. However, clinically, the situation did not demand analgesics even though the difference was statistically significant. It also showed that the difference in visual analogue scale on postoperative day one was not significant between the two studied groups. A study conducted by Song et al.20, Kulaceylu et al.21 comparing General Anesthesia. Spinal Anesthesia, and Illioinguinal and illiohypogastric nerve block with monitored anesthesia care showed that the visual analogue scale in the recovery room 30 min postoperatively was lower in the Illioinguinal and illiohypogastric nerve block group. Using the 100 mm visual analogue scale, the score was 15±1.4 mm in the Illioinguinal and illiohypogastric nerve block group and 34±3.2 mm in the subarachnoid block group. In agreement with our study, Dongare and Dongare22 showed that the time when the patient demanded first rescue analgesic postoperatively was significantly earlier in the subarachnoid block group compared with the Illioinguinal and illiohypogastric nerve block group. They observed that the mean analgesia duration was 188.5±24.6 min in the subarachnoid block group and 361.5±74.4 min in the Illioinguinal and illiohypogastric nerve block group. In disagreement with the present study, Yilmazlar et al.24 conducted a study to compare subarachnoid block with Illioinguinal and illiohypogastric nerve block and he demonstrated that the time to first dose of rescue analgesia postoperatively was 3.30±0.2 hours in the subarachnoid block group and 2.7±0.13 hours in the Illioinguinal and illiohypogastric nerve block group. The difference in the result may be attributed to the use of ultrasound guidance in the present study. Hu et al..5 conducted a pilot study to evaluate ultrasound guided Illioinguinal and illiohypogastric nerve block. The study showed that all patients had successful blocks, without complications. The mean opioid consumption was 10 mg of intramuscular morphine during the first 24 hours .In the present study, total amount of propofol used intraoperatively in group B (SAB) was significantly lesser than that in group A (IINB). The intravenous sedation may be required as local anaesthetics blocks pain sensation, but pressure sensation and traction on deeper tissues are not eliminated. The anaesthesiologist must adjust the level of the sedation that makes the patient and the surgeon comfortable until the end of the procedure10. In agreement with our study, a study conducted by Song et al.20 illustrated that the total dosage of propofol used during surgery was higher in the Illioinguinal and illiohypogastric nerve block group with monitored anaesthesia care and significantly different from the spinal and general anaesthesia groups. Propofol has rapid redistribution and short elimination half-life that results in a rapid recovery from the effects of a single bolus dose, as well as following a continuous infusion. Propofol has rapid onset and short duration of action ensures prompt responsiveness to changes in its infusion rate, which can be achieved using a variable rate of infusion. Propofol is the nearest to an ideal agent for sedation during regional anesthesia. [11] A study conducted by Dongare and Dongare[22] to compare Illioinguinal and illiohypogastric nerve block versus subarachnoid block for hernia repair as a day care surgery showed that, during the hernia sac handling, local anesthesia infiltration, supplemental sedation, or analgesia may be required. For any discomfort during surgery, supplementation was given with bolus propofol up to 1 mg/kg. Like ours Dorreya M. Fekrya et al..23 also concluded in a study that Ultrasound guided Illioinguinal and Illiohypogastric Nerve Block and genital branch of Genitogemoral nerve block under sedation are good anaesthetic techniques for inguinal hernia repair surgeries. In the present study, the ambulation time in Group A (IINB) was significantly earlier than that in the group B (SAB). Song et al..20 showed that the time to home readiness was significantly earlier in patients receiving Illioinguinal and illiohypogastric nerve block with monitored anesthesia care (133±68 min) than in patients receiving subarachnoid block (280±80 min). In the study conducted by Dongare and Dongare,22 there was a significant difference in time to postoperative ambulation between the two groups. The mean duration of postoperative ambulation was longer (298.6±27.9 min) in group 1 (SAB) in comparison to group 2 (IINB) where it was 120.1±15.8 min. In our study comparison between the two studied groups according to the patient and surgeon satisfaction was nonsignificant. In accordance with our results, Bang Ys et al.12, who conducted a study to compare subarachnoid block with Illioinguinal and illiohypogastric nerve block under monitored anesthesia care, showed that patient’s satisfaction in the recovery room was nonsignificant between the two groups. On comparing surgeon satisfaction, in group 2 (SAB), surgeons were significantly more satisfied. The reasons for this limited use could be the surgeon’s desire for a relaxed operating area or the reputation of local anesthesia because of a previous non optimal technique with unacceptable intraoperative pain as a consequence. Another drawback is the surgeon’s lack of familiarity with the technique [19]. In contrast to the present study, Bang et al.12, who conducted a study that compared subarachnoid block with ilioinguinal and iliohypogastric nerve block under monitored anesthesia care, showed that surgeon satisfaction was significantly better in the ilioinguinal and iliohypogastric nerve block group. In our study the significant difference in the intraoperative mean arterial blood pressure between the two study groups may be due to the hypotensive effect of subarachnoid block as it causes preganglionic sympathetic blockade, thus decreasing the systemic vascular resistance resulting in peripheral pooling of blood, which reduces the venous return and preload. 25
CONCLUSION Ultrasound guided ilioinguinal and iliohypogastric nerve block provides good alternate anaesthetic technique for inguinal mesh hernioplasty in high risk patients with contraindicated spinal or general anesthesia. Intraoperative sedation in the form of intravenous infusion of propofol enhances patient and surgeon acceptability to local anesthesia techniques.
REFERENCES
Policy for Articles with Open Access
|
|
 Home
Home