|
Table of Content - Volume 17 Issue 1 - January 2021
A comparative study between intravenous ondansetron with dexamethasone and ramosetron in preventing postoperative nausea and vomiting in patients undergoing middle ear surgeries
Prashanth Gowtham Raj S K1, Damodar Reddy Y2*, Chethanananda T N3, Prathiksha B Rao4, Rashmi H R5
1Assisstant Professor, 3Professor, 4,5Post Graduates, Department of Anaesthesiology, Adichunchanagiri Institute of Medical Sciences, Adichunchanagiri University, BG Nagara 571448, Mandya dist, Karnataka, INDIA. 2Consultant, Leelavathi Hospitals and Diabetic care, Near Renigunta hospital, M G road, Rly Kodur, Kadapa, Andhra Pradesh, INDIA. Email: ranjithachandru1@gmail.com
Abstract Background: Post operative Nausea and Vomiting (PONV) is the second most common complaint in the post-operative period after pain with a relatively high incidence after middle ear surgery up to 80% when no anti emetics is used. This study is intended to compare the efficacy of intravenous ondansetron with dexamethasone and ramosetron in preventing PONV in patients undergoing middle ear surgeries. To determine the efficacy of prophylactic intravenous ondansetron with dexamethasone and ramosetron in preventing PONV in patients undergoing middle ear surgeries. To assess the requirement of rescue antiemetics in postoperative period. Methods: Sixty patients belonging to American Society of Anesthesiologists (ASA) physical status classification I or II aged between 20-50 years, who were undergoing middle ear surgeries under general anaesthesia were randomly allocated into 2 groups. Group OD received dexamethasone 8mg diluted with NS upto 5ml, 5minutes before induction and ondansetron 4mg, 30minutes before the end of surgery. Group R received 5ml of NS 5minutes before induction and 0.3mg ramosetron i.v, 30minutes before the end of surgery. Postoperatively, patients were assessed at 0-2hours, 2-6hours, 6-24hours and 24-48hours for episodes of nausea, vomiting, retching. Rescue antiemetic inj. metoclopramide 10mg i.v. will be given in the events of one/more episodes of vomiting. Complete response was defined as the absence of nausea, retching and vomiting and no need for rescue antiemetic during the 48 hours observation period. Results: In our study, OD group showed 83% complete response which is higher than 57% of R group. Requirement of rescue antiemetic was less in OD group compared to R group (17% vs. 43%). Conclusion: Thus, our study showed, combination of dexamethasone(8mg) and ondansetron(4mg) is superior to ramosetron(0.3mg) alone for prevention of PONV after middle ear surgery. Key Words: Middle ear surgeries; ondansetron; dexamethasone; ramosetron; postoperative nausea and vomiting
INTRODUCTION Post operative Nausea and Vomiting (PONV) is the second most common complaint in the post-operative period after pain1 with a relatively high incidence after middle ear surgery up to 80% when no anti emetics is used2. The main cause of PONV in middle ear surgery is vestibular stimulation caused by drilling and irrigating the bone adjacent to the inner ear, increased middle ear pressure due to nitrous oxide. Acetylcholine and histamine are involved in the transmission of signals from the vestibular system to the vomiting centre. The consequences of PONV are physical, surgical and anaesthetic complications for patients as well as financial implications for the hospitals or institutions, and it is one of the most common reasons for poor patient satisfaction rating in the postoperative period.10,11 It is postulated that ondansetron and other 5-HT3 receptor antagonists exerts its antiemetic action both peripherally (vagus and sympathetic nerves) and centrally (CTZ and vomiting center) by blocking stimulation of serotonin receptors. Serotonin Receptor Antagonists (SRA) like Ondansetron has a proven efficacy and is recommended as a prophylactic antiemetic at the time of induction of anesthesia. The precise mechanism of action of Dexamethasone is unknown but it has been proposed that the antiemetic properties arise due to activation of glucocorticoid receptors in the medulla, or by inhibiting central production of prostaglandins or inhibiting the release of endogenous opioids.12,13 Ondansetron provides significant reduction in early PONV.2 Dexamethasone has been used mainly to reduce late PONV.3,4,5 Therefore, a combination of dexamethasone and ondansetron is considered the optimum choice for prevention of PONV after middle ear surgery6,7 The newer 5-HT3 antagonist ramosetron, with long duration of action, has been found to be more effective than ondansetron in reducing the early as well as delayed PONV, when used in other surgeries.8 Therefore, we conducted this study to compare the combination of ondansetron and dexamethasone with ramosetron for prevention of early and late PONV up to 48 h after the middle ear surgery. Aims And Objectives The objectives of this study are:
MATERIALS AND METHODS Approval from the ethical committee of our hospital (Adichunchanagiri Institute of Medical Sciences and Research Centre) was obtained. Written informed consent was obtained from all the patients for this prospective, randomized, double-blind study. Sixty patients belonging to American Society of Anesthesiologists (ASA) physical status classification I or II aged between 20-50 years, who were undergoing middle ear surgeries under general anaesthesia were included in this study.Exclusion criteria were ASA physical status 3 and 4,smokers,history of motion sickness, known alcohol or drug abuse, pregnancy or lactating females, patients who have received other antiemetic medications or preoperative steroid, patient with known drug sensitivity and patients with diabetes mellitus and hypertension. Patients were randomly allocated to receive a combination of dexamethasone 8 mg diluted with normal saline up to 5ml, given 5 minutes before the induction of anaesthesia and ondansetron 4 mg given half an hour before the end of surgery (group OD, n=30) or ramosetron 0.3 mg IV, given half an hour before the end of surgery (group R, n=30), by a computer-generated randomization table. Complete Pre-anaesthetic checkup was done to all patients posted for surgery. Standard fasting ASA guidelines were followed. All patients were premedicated the night before with Tablet ranitidine (150 mg, PO) and Tablet diazepam (10mg, PO). The anesthesia technique was standardized in all patients. In the operation room, monitoring was done with 5 lead electrocardiogram, pulse oximetry, noninvasive blood pressure, and capnography. General anesthesia was induced with fentanyl (2 mcg/kg), propofol (2 mg/kg), and vecuronium (0.1 mg/kg) to facilitate endotracheal intubation. Anesthesia was maintained with isoflurane 1-1.5% with nitrous oxide 50% in oxygen. Ventilation was mechanically controlled and adjusted to maintain an end-tidal concentration of CO2 between 35 - 40 mmHg. To reduce the blood loss, anesthetic depth was adjusted to keep mean arterial pressure about 20%-30% below baseline. The patients’ heart rate and mean arterial pressure were noted every 30 minutes during surgery. Neuromuscular block was reversed with neostigmine and glycopyrrolate at the end of surgery. After the clinical assessment of adequacy of the reversal of neuromuscular block, trachea was extubated. Near the end of surgery, all the patients were given paracetamol 15 mg/kg intravenously for postoperative analgesia. Primary efficacy variables assessed were the incidence and severity of nausea and the incidence of vomiting in the first 48 hours after the surgery. Secondary efficacy variables included the use of additional antiemetic as rescue and medication associated complications. The variables were assist by an investigator who is blinded to the treatment group. Evaluation were performed in the first 2-6 hours, 6-24 hours, 24-48 hours post operatively. If the patient developed nausea or vomiting in the postoperative period, then metaclopramide 10mg i.v. will be given slowly, as a rescue antiemetic. If the patients PONV persisted in-spite of rescue anti emetic, the physician is allowed to give any other anti-emetic as per their discretion. The patients were enquired about the common side effects of medication mainly head ache, dizziness, constipation and flushing. Complete response defined as the absence of nausea, retching and vomiting and no need for rescue antiemetic during the 48 hours observation period. Statistical Analysis The sample size was decided in consultation with the statistician and was based on initial pilot study observations, indicating that approximately 23 patients should be included in each group in order to ensure a power of 0.80. Assuming a 5% drop out rate, the final sample size was set at 30 patients in each group, which would permit a type 1 alpha error =0.05, with a type 2 error of beta=0.2. Statistical analysis were performed using SPSS ver. 20.0 (SPSS Inc., Chicago, IL, USA). Categorical variables were compared using the chi-square test or fisher's exact test. Continuous variables were compared using independent t-test. Data are presented as mean ± standard deviation or as the number of patients and percentages. P value of less than 0.05 was considered statistically significant.
RESULTS All the 60 patients completed the study protocol (no dropouts) and were analyzed for primary efficacy. The patient's characteristics, duration of surgery or anesthesia were not significant between the two groups. There was no significant difference in the measured mean arterial pressure and heart rate between the group[table 1].
Table 1: Patient characteristics, surgery and anaesthetics data
Table 2: Incidence of postoperative nausea and vomiting (2 hours,6 hours,24 hours and 48 hours)
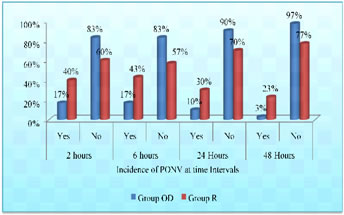
Graph 1: Incidence of PONV among OD and R group at regular intervals
There was statistically significant difference in PONV in the first 2 hours, 6 hours, 24 hours and 48 hours after the surgery. The incidence of nausea was significantly lower in the dexamethasone and ondansetron group compared to the ramosetron group (P <0.024)[Table 2] [Graph 1]. The incidence of vomiting and use of rescue antiemetic was clinically significant showing that less patients required rescue emetics compared to the R group. The patients who never developed nausea or vomiting during the 48 hours observation period were considered to have had complete response. It was observed that 25 (83%) patients in the dexamethasone and ondansetron group had complete response compared to 17 (57%) patients in ramosetron group (P=0.024)[Table 3].The incidence of adverse effects were comparable in both the groups and was statistically insignificant.
Table 3: Incidence for need for rescue antiemetics and complete response
DISCUSSION Post operative Nausea and vomiting (PONV) is a troublesome experience after general anesthesia and surgery, with an incidence ranging between 20–80% among different surgeries. Middle ear surgery (tympanoplasty or mastoidectomy) is associated with a higher incidence of PONV (60–80%) warranting the use of prophylactic anti-emetics. The etiology of PONV after middle ear surgery is multifactorial in origin and depends on age, sex, history of motion sickness and/or previous PONV, duration of surgery, type of drugs and technique used for anesthesia and postoperative pain. In the middle ear surgery, due to stimulation of the labyrinth, PONV usually persists for up to 24 hours after anesthesia2,14. Patients with a high risk of PONV needs a combination of antiemetic drugs, with a different mechanism of action to provide better prophylaxis and less side effects of each drug. In our study, we used 5-HT3 receptor antagonists (ondansetron) and dexamethasone combination because various authors confirm the effectiveness of this combination is superior to other combinations or monotherapy in a different type of surgery. In our study the dosage selection of ondansetron (4 mg, i.v.) was based on previous studies done by McKenzie et al..16 in 1993, Honkavaara P et al..,2 in 1995 , Kovac et al..,17 in 1996 and prophylactic ondansetron meta-analysis by Figueredo and Canosa18 in 1998. Ramosetron 0.3 mg is considered as appropriate dosage for preventing postoperative emesis after anaesthesia. The dosage selection of Ramosetron (0.3 mg, i.v.) was based upon the studies done by Fujii et al..19, 20. In addition the manufacturer’s recommended dose is 0.3 mg i.v. once a day21. The corticosteroid, dexamethasone effectively prevents nausea and vomiting22, 23. Dexamethasone aggravates the effect of other antiemetics by various mechanisms like prostaglandin antagonism, release of endorphins and bradykinin reduction .It is recommended at a prophylactic dose of 8 mg i.v. for patients at increased risk for PONV and the dosage selection is based on the study done by Sameer Desai et al..15, Rajeev V et al.9 and Elhakim M et al..6. The recommended timing for administration is at induction of anesthesia rather than at the end of surgery23. Studies have shown that ondansetron is more effective in preventing early but not late PONV, whereas dexamethasone was found to have more pronounced action in the late postoperative period.3,4,5 This may be due to the shorter duration of action of ondansetron (4 h) in contrast to the prolonged duration of action of dexamethasone. Thus, the combination of ondansetron and dexamethasone can decrease the incidence of both early and late nausea and vomiting. Studies done by Panda NB et al.. 6, Desai et al..15 and Usmani H et al.24, have shown that the combination of dexamethasone and ondansetron is more effective than ondansetron alone after middle ear surgery. Ramosetron is a newer 5-HT3 receptor antagonist which is more potent and has a longer duration of antiemetic action than the older agents. This has been attributed to the higher binding affinity and slower rate of dissociation from the target receptor of ramosetron compared to ondansetron. The elimination half-life of ramosetron is also longer than that of ondansetron (9 h vs. 3.5 h).9 Many of the recent studies have shown that ramosetron is more effective than ondansetron in preventing PONV for the patients undergoing various other surgeries.[8,25,26,27] Furthermore, antiemetic efficacy of combination of ramosetron and dexamethasone was found to be similar to that of ondansetron and dexamethasone, when used as prophylaxis for the spine surgeries.28 Addition of dexamethasone did not provide any advantage to ramosetron. Authors concluded that although the addition of corticosteroids could theoretically obviate the inferiority of the 5-HT3 antagonists, the more potent affinity for the 5-HT3 receptor would not lead to more synergistic pharmacodynamic results, if drugs from different classes partially involve common antiemetic mechanisms. Thus addition of steroid may not benefit ramosetron. Therefore, this study was carried out to compare the combination of ondansetron and dexamethasone with ramosetron for early and late PONV up to 48 h after surgery. We noted that the combination of two antiemetics, ondansetron and dexamethasone, had better efficacy than the single agent when used as a prophylaxis against PONV. It is recommended that the drugs with different mechanisms of action should be used in combination to optimize the efficacy.There are abundant 5-HT3 receptors present in the vicinity of trigeminal nerve and vestibular labyrinth; hence, 5-HT3 receptor antagonists are efficacious in middle ear surgeries. Dexamethasone may act by serotonin inhibition in the gut through prostaglandin antagonism. It can significantly decrease the tissue inflammation, and thus reduces the ascending impulse to the vomiting center. It also improves the action of other antiemetic drugs by sensitizing the pharmacologic receptors to the other antiemetics.17 Therefore, the combinations of dexamethasone and 5-HT3 antagonist have an additive effect in reducing the PONV.
CONCLUSION Present study shows that the combination of dexamethasone and ondansetron is superior to ramosetron for prevention of PONV after middle ear surgery. Therefore, we recommend combination of dexamethasone and ondansetron for prophylaxis of PONV in middle ear surgeries.
REFERENCES
Policy for Articles with Open Access: Authors who publish with MedPulse International Journal of Anesthesiology (Print ISSN:2579-0900) (Online ISSN: 2636-4654) agree to the following terms: Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution License that allows others to share the work with an acknowledgement of the work's authorship and initial publication in this journal. Authors are permitted and encouraged to post links to their work online (e.g., in institutional repositories or on their website) prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work.
|
 Home
Home