|
Table of Content - Volume 17 Issue 1 - January 2021
Post-operative analgesia following mastoid surgeries: Comparison between selective nerve blocks (greater auricular and auriculotemporal) v/s parenteral opioid (pentazocine)
Rutvi M Mody1, Sonali Joshi2*, Divyang Shah3
1IIIrd Year Resident, 2Assistant Professor, 3Professor & HOD, Department of Anaesthesiology, SMIMER, Surat, Gujrat, INDIA. Email: sonalij6877@gmail.com
Abstract Background and aim: Aim of the study is combining peripheral nerve block to general anaesthesia technique to reduce the intra operative requirement of opioid analgesic and thereby reduce incidence of opioid induced side effects like post-op nausea-vomiting (PONV) without compromising on quality of analgesia and patient comfort in intra-operative and immediate post-operative period by using VAS score, Ramsay Sedation score, PONV Impact scale score. Materials and methods: 70 patients of ASA grade I and II undergoing elective mastoid surgeries were studied prospectively and were randomly devided in two groups N and P, who received selective nerve blocks (greater auricular and auriculotemporal nerve blocks) and Intravenous Injection pentazocine (0.03-0.07 mg/kg IV) respectively. Results: At the end of 3 hour after surgery mean VAS score (≥4) of group P was significantly higher than group N. Most of the patients of group P required rescue analgesia at the end of 3 hours where as group N patients required rescue analgesia at the end of 22-24 hours and group N patients had a less frequent incidence of vomiting requiring intervention. Conclusion: Greater auricular and auriculotemporal nerve block holds considerable promise in producing effective and prolonged post-operative analgesia, minimal sedation and less post-operative nausea and vomiting for patients undergoing mastoid surgeries. Key Words: Post-operative analgesia, Mastoid surgeries, Intravenous opioid, Greater auricular nerve block, Auriculotemporal nerve block
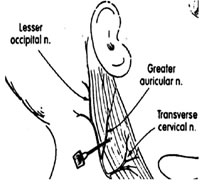
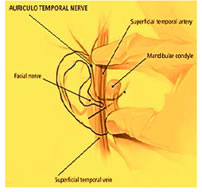
INTRODUCTION Mastoid surgeries are common procedures in otorhinolaryngology practice. Proper analgesia is vital for postoperative compliance. So, regional anaesthesia is often combined with general anaesthesia to provide better postoperative outcomes.1 Immediate post-operative pain relief could decrease postoperative use of opiates and in turn limits its side effects like nausea, vomiting, respiratory depression, urinary retention, constipation etc. Greater auricular nerve block and auriculotemporal nerve block techniques are relatively easy to learn and have a variety of uses both in the operating room and outpatient environments for all practitioners. The superficial anatomic location of these nerves ensures successful blockade without any damage to neighbouring structures. Utmost care must be taken by repeated negative aspiration to avoid any intravascular deposition of local anaesthetic agents.12 Avoidance of deep placement of needle during GAN blockade prevents occasional facial and cervical plexus blockade and the consequent Horner’s syndrome. MATERIALS AND METHOD The study was conducted among 70 indoor patients admitted to our tertiary care hospital and divided them in 2 groups (n=35). Study type: Observational Inclusion Criteria: Age - between 18-50 years. ASA Grading I and II. Type of surgery – Mastoid surgeries Exclusion criteria: Pt’s refusal. Pt having history of known allergy to local anesthetic agent. Any infection at the site of anatomical landmark. Pt having altered coagulopathy. Patients who are unable to understand visual analogue score. The sensory nerve supply of the ear is mostly from the Greater Auricular Nerve (GAN) and the Auriculo Temporal Nerve (ATN). Anatomical landmark of these two nerves are well defined for blockade with local anaesthetics. Anatomy of Greater auricular and Auriculotemporal Nerves: The GAN (Fig. 1), a branch of the superficial cervical plexus (C2-3), emerges from the plexus at the Erb point at the posterior border of the sternocleidomastoid muscle and supplies the back of the auricle (except its upper part), the lobule and the concha. The ATN (Fig. 2) branches out from the mandibular nerve very high on the level of the temporomandibular joint, and then becomes superficial and goes up towards the tragus, posterior to the superficial temporal vessels. It gives superficial branches starting to the tragus, the entry of the auditory canal and the anterior part of auricle of the ear.[13] Figure 1 Figure 2 Technique of nerve blocks Greater auricular nerve block: first Identify the posterior borders of the sternocleidomastoid muscle, and draw a line at the posterior border of the muscle. Draw a line from the inferior edge of the mastoid process 2 centimeter below it. The point where this 2 lines intersect, inject a 3.5 ml of local anaesthetic in a fan shaped manner.[16]
Auriculotemporal nerve block technique: To avoid facial nerve blockade, a potential complication of auriculotemporal nerve block, we have used modified technique, in which we have injected 1.5 ml local anaesthetic 1 cm above the level of tragus, just behind the superficial temporal artery after negative aspiration for blood.[6,8] Preoperative evaluation of patient was done before the surgery by taking history, general and systemic examination, vitals and necessary investigations and fitness for anesthesia is declared accordingly. Written informed consent was taken. NBM status of patient was noted. In recovery room after assessing patient’s heart rate, blood pressure, SPO2 on air, IV line was secured with 18/20 gauge IV cannula for IV fluids and patients were premedicated 30-35 mins prior to induction of anesthesia with patients in both the groups were given Inj.Glycopyrrolate 0.005 - 0.01 mg/kg IM. Intraoperatively preoxygenation was done with 100% O2 for 3 min. Induction done with Inj. Thiopentone Sodium 5 mg/kg and Inj Succinylcholine 1.5mg/kg with IPPV. Oral intubation done with adequate size portex cuffed ET tube. Maintenance with 50% N2O in 50% O2 with 0.5-1% isoflurane and muscle relaxant Inj Vecuronium 0.08 mg/kg initial dose and 0.01 mg/kg maintenance dose given. Group N : After intubation ,Patients were given Greater auricular and Auriculo temporal nerve block by landmark technique with Inj Bupivacaine Plain (0.5%) (5 ml) after negative aspiration for blood. Group P : Inj. Pentazocine 0.5 mg/kg was given . Intraoperatively hemodynamic parameters were monitored. At the end of surgery patients were reversed by inj.glycopyrrolate 0.01 mg/kg IV and inj.neostigmine 0.05 mg/kg and extubated by standard criteria of extubation. Post operative vitals were noted and assessment was done for the following:
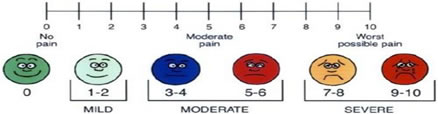
Visual Analog Scale (0-10) was used for post-operative pain assessment.
RAMSAY SEDATION SCALE SCORE
OBSERVATIONS AND RESULTS Patient’s Characteristics In demography, there was no difference between group P and N regarding age, sex, weight, BMI, type and duration of procedure performed.
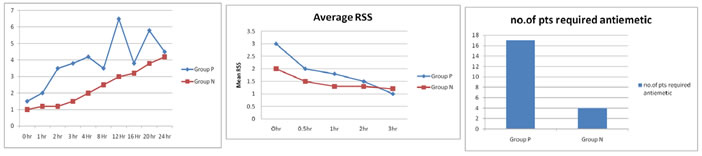
Mean VAS
Mean RSS
PONV Impact Scale Score
PONV impact score of ≥ 5 was seen more in group P (17patients) as compared to group N (4 patients). A score of ≥ 5 was clinically important and was treated with IV Metoclopramide (10mg).
DISCUSSION Our study was aimed at combining peripheral nerve block to general anaesthesia technique to reduce the intra operative as well as post operative requirement of analgesic. Combining Local anaesthesia with general anaesthesia has many advantages over general anaesthesia alone like less bleeding, Less postoperative nausea and vomiting, less expensive. According to results obtained from our study, more patients in the pentazocine group as compared to Nerve block group complained of pain and had to be administered injection diclofenac as rescue analgesic within 24 hours. Above graph further confirmed that statistically significant difference in mean VAS scores was seen at 3 hours between both the groups. At 3 hours almost all the patients in group P had VAS of ≥ 4 as compared to group N, in which VAS ≥ 4 reached at 24 hours. These findings were in contrast to the study by Suresh et al. on children between 2 to 18 years. They had observed higher pain scores at 0 h in the Nerve block group. This may be due to the fact that they had conducted GAN block only whereas, we had combined ATN block along with GAN.12 The comparison of Ramsay Sedation Scores indicated that 23 patients in group P as compared to 8 patients in nerve block group had clinically significant sedation (RSS > 3) on arrival at PACU. Out of the group P patients who needed rescue analgesic at 3 hour, 19 patients were either, anxious, agitated or restless (RSS = 1). This was significantly higher in comparison to Group N, where 8 patients had RSS of 1. The average RSS of group P was lower than group N only at 3 hour. For the rest of the observation period the average RSS was always comparable in both the groups. Comparing the overall incidence of post operative nausea and vomiting with the help of PONV Impact scale score indicated that, significantly more number of patients in group P had clinically significant PONV. In this, 17 patients in group P as compared to 4 patients in group N required rescue administration of injection Metoclopramide. GAN block had been studied by Burtles et al. for bat ear surgery and Cregg et al. for otoplasty. Here we combined GAN with ATN block so as to reversibly abolish all the sensory distribution of the ear.1,2 The results of following studies were comparable to our study: Santoshkumar et al. in 2017 did comparative study between greater auricular and auriculotemporal nerve block v/s intravenous morphine in mastoidectomy patients. They conluded that VAS score and requirement of rescue analgesics was significantly less in the N group for the first 3 hours post operatively and group N patients had a less frequent incidence of vomiting. Their study results were comparable to our study.13 In 2018, Korgun Okmen studied the effect of ultrasound guided greater auricular v/s superficial cervical plexus block for postoperative tympanomastoid surgery analgesia. He found that there was no statistically significant difference in VAS score at all measured time between both the groups (p>0.05),but the disadvange of SCP block application is that the complication that can occure are more serious than those that can occure in GAN block application.[9] Marzieh and Elizabeth et al. in 2017, treated greater auricular neuralgia patient with ultrasound guided greater auricular nerve block.[3] Michael and Colin et al. gave greater auricular nerve block in a patient with comorbidities for surgical resection of an ear skin lesion in 2016.7 In addition to this, GAN block can also be used for outpatient on a day care basis or emergency department procedures without the need for a separate anaesthesia team.[4] Here we had used landmark techniques, but the ultrasound guided technique of this block can also be used, which increases reliability of this block, as well as prevention of inadvertent vascular puncture.[14,15] We performed this block with landmark technique, as we didin’t have facility for ultrasound guided block at our hospital. All above studies favours use of GAN and ATN block in mastoid surgeries for introperative as well as post operative analgesia with excellent result.
CONCLUSION The GAN and ATN have predictable anatomy and are readily amenable to local anaesthetic blockade by anatomical landmark techniques. Here, our study concludes that combination of GAN and ATN block with general anaesthesia is an uncomplicated, effective and well tolerated method for the safe conduct of mastoid surgery. This can facilitate early recovery, quality analgesia, minimal nausea vomiting, early return to oral feeding and thereby shorter hospital stay for these patients. As daycare surgery and anaesthesia is evolving in India, combination of regional analgesia techniques with general anaesthesia can help in popularizing the day care concept.5,10,11,13 We suggest that this technique decrease analgesic requirement and shorter the hospital stay.
REFERENCES
Policy for Articles with Open Access: Authors who publish with MedPulse International Journal of Anesthesiology (Print ISSN:2579-0900) (Online ISSN: 2636-4654) agree to the following terms: Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution License that allows others to share the work with an acknowledgement of the work's authorship and initial publication in this journal. Authors are permitted and encouraged to post links to their work online (e.g., in institutional repositories or on their website) prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work.
|
 Home
Home