|
Table of Content - Volume 17 Issue 1 - January 2021
Efficiency of fascia iliaca compartment block as a part of multimodal analgesia for post- operative analgesia after femoral bone surgeries
P R R Kamal1, Prashant Lomate2*
1JR3, 2Associate Professor, Department of Anaesthesiology, Bharati Vidyapeeth (Deemed to be) University Medical College and Hospital, Sangli, Maharashtra, INDIA.
Abstract Background: Postoperative pain control after femoral bone surgeries is of paramount importance to decrease patient’s morbidity and mortality. In this study we assessed the effect of fascia iliaca compartment block (FICB) when it is used as a part of multimodal analgesia after surgery for femoral bone fracture. Material and Methods: A total of 100 patients of ASA grade I and II aged 18-60 years, posted for elective femoral bone fracture surgery under subarachnoid block were randomly allocated into two groups. Group A received FICB with 40 ml of 0.25% levobupivacaine post-operatively, group B did not receive FICB. The two groups were compared for the time to first rescue analgesic (Injection tramadol), number of rescue analgesic demands, total analgesic consumption in first 24 hours, VAS scores and the adverse effects. Z test was applied for data analysis. Results: Both the groups were demographically comparable. Time for first analgesic request was significantly prolonged in Group A when compared to Group B [ 8.16±0.45 vs 2.67±0.34min]. VAS pain scores within first 24 hours were lower in Group A [p= <0.00]. Total 24 hours tramadol consumption was reduced in Group A [214.29±45 vs 390.53±48 mg]. Incidence of postoperative agitation was more in Group B [ p= <0.00]. Conclusion: A single injection for FICB could lead to prolonged time for the first analgesic request and reduced total 24 hours analgesic consumption after surgery for femoral bone fracture. Key words: fascia iliaca compartment block, levobupivacaine, pain, rescue analgesic, tramadol.
INTRODUCTION Fascia iliaca compartment block has been an established technique for postoperative analgesia after surgery for femoral bone fracture. FICB is technically easy, effective for postoperative pain control after operation for femoral bone fracture and decreases the complications induced by systemic analgesic drugs.1 The severity of postoperative pain is affected by genetics, cultural and social factors across the world.2,3 In this prospective randomized study we assessed the effect of FICB when it was used as a part of multimodal analgesia (MMA) after surgery for femoral bone fracture. The block was first described by Dalens et al. in 1989.[4] This new technique of regional block was used to block the femoral lateral cutaneous nerve of the thigh and the femoral nerve. The FICB has proved to be an easy and safe technique. It is free from complications because the major nerves and vessels are far from the side of needle insertion. Though various methods including opioids, nonsteroidal anti-inflammatory drugs (NSAIDs) and different regional analgesia techniques have been described in the literature for postoperative pain management, there is still a continuous search to find an ideal way.Systemic analgesics such as opioids and Non-steroidal anti inflammatory drugs are associated with different side effects.[5,6]Even though the usual definitive treatment is surgical, pain after femoral bone fracture surgery impairs the ability of the ambulation of the patient and may delay the hospital discharge.7 Ultrasound (US) guided FICB is an easy and simple technique for postoperative pain management. We designed this study with the aim of assessment of analgesic efficacy of FICB with the hypothesis that it will provide prolonged duration of postoperative analgesia after femoral bone surgeries. This hypothesis was tested by comparing the duration of analgesia, which was our primary objective. The secondary objectives were to compare the number of rescue analgesics required, total consumption of rescue analgesics, VAS scores and complications in a 24 hour period; and patient satisfaction score.
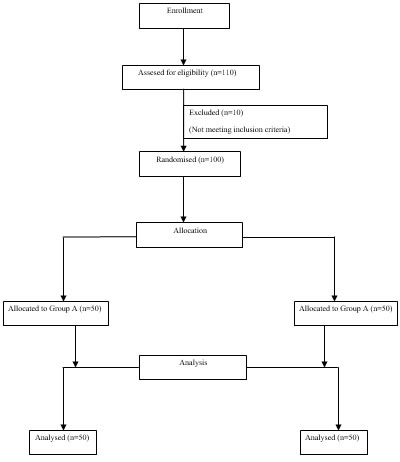
MATERIALS AND METHODS This prospective randomized double blind study was carried out in 100 ASA grade I and II patients of either sex, aged 18-60 years posted for elective femoral bone surgeries under spinal anaesthesia (SA) [Figure 1]. This parallel designed (allocation ratio 1:1) study was conducted in a tertiary care unit from January 2019 to July 2019 after obtaining hospital ethical committee approval (BV(DU)MCandH/Sangli/IEC/360/19) and informed written consent from the patients for study and publications. Patients having any cardiorespiratory, neurological or psychiatric illness, coagulation abnormalities, known sensitivity to local anaesthetics were excluded from the study. Randomization was done by a sealed envelope method. The patients and the anesthesiologist monitoring the patients were blinded to the procedure. Patients admitted for surgery following an overnight fast of 8-10 hours. At the preanaesthetic interview the patients were familiarized with a VAS scale and other postoperative questionnaire . Patients were premedicated with Ondonsetron 4mg i.v. . On arrival in the operating room, routine monitoring devices were placed, and baseline blood pressure, heart rate and pulse oximetry values were recorded. All study patients were given Injection dexamethasone 8mg IV as a part of multimodal analgesia. After surgery, the patients in group A were given FICB with 40 ml of 0.25% levobupivacaine under US guidance. The high frequency linear probe (13-6 MHz, Sonosite turbo) was placed just below the inguinal ligament in longitudinal plane. After visualization of femoral vessels the probe was moved laterally to visualize the fascia lata, fascia iliaca and psoas muscle. A 23 G spinal needle connected to 10 cm extension tube was passed from lateral to medial side parallel to the probe in longitudinal axis. A plane is created between fascia iliaca and iliopsoas muscle with two ml of normal saline. Then 40 ml of 0.25% levobupivacaine was injected into the plane and spread of drug was observed towards femoral nerve. This time was considered as zero time for assessment of parameters. In group B, only painting and draping of inguinal area was done, but block was not given. Postoperative pain scores were assessed by using a visual analogue scale score at 15 minutes, 2 hours, 6 hours 12 hours and 24 hours postoperatively. At the same time the side effects like nausea, vomiting and complications like haematoma if any were also noted. Duration of analgesia was considered as the time taken between zero time and the first analgesic demand by the patient. Injection tramadol 1mg/kg IV was given as a rescue analgesic at VAS ≥ 4 with a maximum dose 400 mg in 24 hours. Number of rescue analgesics required and total analgesic consumption in 24 hours were also recorded. The patients who required rescue analgesic in the immediate postoperative period were excluded from the study. The confounding variables like use of adjuvants which may interfere in results were eliminated. Patients with history of drug use/abuse, psychiatric disorders or chronic pain were also excluded. The sample size was calculated with the help of the reference of previous study.8 With a 5% α level of significance and 90% power of the test to detect a difference of 4.6 hours between the two groups, minimum sample size calculated by using a statistical formula was 50 per group.9,10 Data was collected and tabulated in excel sheet. Data was compared and analyzed statistically for the significance of observed differences if any. The P values < 0.05 were considered significant and P<0.01 was considered highly significant. The results were expressed as Mean ± SD (Standard Deviation) for continuous variables. Mean was obtained for VAS scores .Unpaired t-test was used for inter-group comparison of continuous variables. Numerical data were compared within the group against baseline values using paired t-test. Mann -Whitney U test was used to compare ordinal variables. Statistical package for social sciences (SPSS) version 22 for windows (IBM – Chicago) was used for statistical analysis and to draw conclusions.
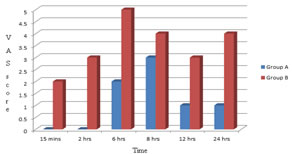
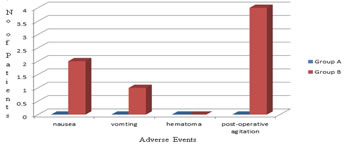
RESULTS Demographic data of two groups were comparable and nonsignificant.[Table 1] The one hundred and ten patients were enrolled for the study, out of which hundred patients were analyzed [Fig. 1]. The time for first analgesic request was significantly prolonged in FICB group (Group A = 8.16±0.45 h vs Group B = 2.67±0.34 h).[Table-1] VAS pain scores within first 24 hours were observed to be on the lower side in FICB group. [Fig-1] [Table-2] The total 24 hours analgesic consumption was found to be reduced in FICB group (Group A = 214.29±45 = mg vs Group B = 390.53±48 mg).[Fig-2] Postoperative agitation was more in Group B (n=0 vs n=4)
Table 1: Demographic data
Values are presented as mean±SD, SD – standard deviation. p<0.05 suggests statistically significant difference.
Table 2: Comparision of Analgesic demands
Figure 1: Consent flow diagram Figure 2: VAS scores Figure 3: Adverse events
DISCUSSION FICB provides good postoperative pain control and prevents negative outcomes such as tachycardia, hypertension, myocardial infarction, immobility and poor wound healing. Persistent post-surgical pain may eventually evolve into chronic pain. FICB is also a good alternative to lumbar plexus or femoral nerve blocks in hip and femur surgeries. It can be performed with Ultrasound or landmark guided “double pop” technique. [11-13] It has less complications than lumbar plexus block or femoral nerve block. It can be repeated in wards. This study shows that FICB provides effective postoperative analgesia when it is used as a multimodal analgesia in the first 24 hours as measured by pain on VAS, total analgesic consumption, and the time for the first analgesic request. In this study, there was significant difference in VAS scores between the FICB and control groups. The postoperative VAS score was reduced more significantly in the FICB group than in the control group at fifteen minutes, two, six, twelve, and twenty four hours. The result at two hours was incomparable with a study done by Monzon et al.14 This difference might be due to the high prevalence of comorbidities found in the studied groups in the study. 14 However, our finding was consistent with a study done by Hanna Let al.15 The similarity might be due to the same dose of a local anesthetic, 40 mL of 0.25% bupivacaine given for patients of 40 to 80 kg body weight. [15] The median VAS score at six hours was more significantly reduced in the FICB group than in the control group. Our finding was comparable with a similar study.9 This similarity might be related to the wear off analgesic effects of spinal anesthesia in the control group, and the efficacy of nerve block in the FICB group continued since the duration of FICB was expected for eight to ten hours.5 The VAS score at 12 hours was lower in the FICB group than in the control group this finding was consistent with a study done by Chu et al...[6] This might be due to pain management using the same class of drug, tramadol was given repeatedly at this time interval for both groups. The VAS score at 24 hours was lower in the FICB group than in the control group the result was incomparable with a study.[15] This discrepancy might be due to the involvement of different junior doctors without training of anesthesia in dealing with FICB patients and controls in the study. [15] However, our finding was comparable with a Korean study showing that FICB could have a better control of pain than intravenous alfentanil during the first 24 hours.[9] This might be related to the equivalent duration of surgery in the FICB and control groups. A study concluded that perineural dexmedetomidine as an adjuvant to LA in USG guided FICB effectively prolonged analgesic duration and also reduced the 24 h postoperative morphine consumption when compared to intravenous dexmedetomidine in elective and emergency femur surgeries.16 A study concluded that ropivacaine and levobupivacaine both are comparable in terms of efficacy and duration with ropivacaine being more cost effective and easily available than levobupivacaine which can be a good choice for FICB.17 In our study, the time for the first analgesic request was prolonged in the FICB group. A Korean study found that the first analgesic request happened after 8.6 hours (516 minutes) in the FICNB group, whereas after 4.5 hours (270 minutes) in the control group.[9] This marked difference compared to that of our study might be related to the cases dealt with by the experienced anesthetists, who also rejected patients with failure of nerve block. There was no complication induced by FICB technique because the site of needle injection for FICB is far from the femoral nerves and blood vessels. Thus accidental intraneural and intravascular injury can be avoided.18-20. Perineural dexmedetomidine as an adjuvant to LA in USG guided FICB effectively prolonged analgesic duration and also reduced the 24 h postoperative morphine consumption when compared to intravenous dexmedetomidine in elective and emergency femur surgeries.16 Its prospective randomized design, appropriate calculation of sample size from previous study, complete follow-up of study population and proper use of protocol to avoid bias are some strengths of our study. However we failed to include a single type of femoral bone surgery to get more accurate results. Multicentric study is recommended to come to the conclusion. We did not register the trial with a trial registry prospectively which is understand was important.
CONCLUSION From our study it is concluded that the fascia iliaca compartment block (FICB), when used as a part of multimodal analgesia provides prolonged duration of postoperative analgesia, reduces number of rescue analgesics required and total analgesic consumption in first 24 hours.
REFERENCES
Policy for Articles with Open Access: Authors who publish with MedPulse International Journal of Anesthesiology (Print ISSN:2579-0900) (Online ISSN: 2636-4654) agree to the following terms: Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution License that allows others to share the work with an acknowledgement of the work's authorship and initial publication in this journal. Authors are permitted and encouraged to post links to their work online (e.g., in institutional repositories or on their website) prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work.
|
 Home
Home